Streptococcus viridans is part of the natural human microflora. The microbe lives on the mucous membrane of the respiratory, digestive and urogenital tracts. Normally, its amount should not exceed 30% of the number of all microorganisms inhabiting these loci.
Bacteria are ubiquitous. In their normal state they are not dangerous to humans. Suppression of immune defense is the reason for the active reproduction of Streptococcus viridans and its acquisition of pathogenic properties. The microbe causes local inflammation and destruction of the cells of the mucous membrane lining the respiratory, digestive and urinary organs. Over time, the pathogenic streptococcus leaves its “territory”. It penetrates the blood and spreads throughout the body, causing severe illnesses that lead to disability of patients and even death.
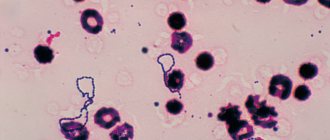
Streptococcus viridans means green in Latin. This name is associated with the ability of bacteria to produce a green color during hemolysis. A microbe can be detected in biological material using bacteriological testing or PCR. Treatment of infection is etiotropic, pathogenetic, symptomatic. Patients are prescribed penicillins, immunomodulators and drugs that eliminate clinical manifestations and improve the general condition of patients.
Streptococcus viridans treatment.
Streptococcus viridans is a non-taxonomic group of commensant low-pathogenic streptococcal bacteria, some representatives of which give a green color during hemolysis, hence the name “viridans” from the Latin.
Viridis, green. They are a significant part of the non-pathogenic microflora (about 30-50% of the total number of microflora microorganisms) of the pharynx, oral cavity and gastrointestinal tract. These streptococci are very common in the natural environment and usually do not pose a danger to a healthy person, however, in various immunodeficiency states, Streptococcus viridans can cause a number of serious diseases - endocarditis, pneumonia, pharyngitis, nephritis, postpartum sepsis, rheumatism, numerous diseases of the skin and soft tissues, invasive infections.
One of the representatives of this group, Streptococcus mutans, secretes a protein in the oral cavity that binds to salivary glycoproteins, which causes destruction of tooth enamel and further causes caries.
Infectious endocarditis is mainly caused by Streptococcus viridans (together with staphylococci and enterococci). Microorganisms reach the heart through the bloodstream, then attach to the inner lining of the heart (especially damaged heart valves) and provoke an inflammatory process.
To diagnose streptococcal infection, the PCR method (polymerase chain reaction method) is successfully used.
It is advisable, for prevention, to use antibacterial drugs before surgical operations and dental procedures and strictly follow the rules of asepsis, use syringes and disposable infusion systems.
Symptoms
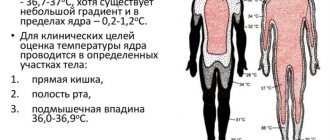
Streptococcus viridans usually causes diseases of the upper respiratory tract. In a child, this microbe is found in the throat and becomes the causative agent of pharyngitis or sore throat. Against the background of a pronounced intoxication syndrome with fever, malaise and apathy, a sore throat, nausea, and hoarseness appears. Sick children are often capricious, cry, refuse to eat, and do not breastfeed. They develop yellow-green nasal discharge, cough, and headache.
Upon examination, specialists detect hyperemic mucous membrane of the pharynx, swelling and hypertrophy of the tonsils. In patients, the face becomes puffy, regional lymphadenitis occurs, a pustular rash appears on the skin, myalgia, arthralgia, hyperhidrosis.
Complications of diseases caused by Streptococcus viridans:
- Acute otitis media,
- Rheumatism,
- Myocardial inflammation
- Glomerulonephritis,
- Bacterial inflammation of the meninges,
- Abscesses of parenchymal organs,
- Sepsis,
- Shock.
The pathogenesis of such complications is not fully known. Their cause is considered to be autoimmune inflammation: antibodies produced to fight infection react to their own cells affected by streptococcus.
Streptococcus viridans 10^5 koe/tamp. Basic information
Ekaterina Vladimirovna (parasitologist)
Heartworms can lead to numerous health problems, shortening your precious life by several years. In the human body, many parasites are extremely difficult to detect. They can be anywhere - in the blood, intestines, lungs, heart, brain. Symptoms of helminthic infestation can be confused with ARVI, gastrointestinal diseases and others. The main mistake in such cases is not caring about your health! If you suspect the presence of parasites, you should urgently contact a specialist. If we talk about medications and self-treatment, then this anti-parasitic complex is suitable for the most common parasites.
Streptococcus viridans - what is it? Bacteria group of alpha-hemolytic streptococci. Some are classified as gamma hemolytic. Microorganisms are included in the list of normal microflora of the oral cavity and pharynx.
This is a beneficial bacterium. Streptococcus viridans performs protective functions - it prevents Pseudomonas aeruginosa and other pathogens of dangerous diseases from entering the body.
Microbiology
Streptococcus viridans is a type of simple bacteria. When hemolysed, they give a green tint, which is why they are called greening. They are Gram-positive and appear blue when stained with Gram.
In addition to the oral cavity and pharynx, bacteria live in the gastrointestinal tract, respiratory and genitourinary systems. They enter the body with food, during meals. During dental procedures and surgical interventions, microbes can enter the general bloodstream.
Externally, microorganisms look like a motionless chain assembled from balls. Microbes do not have flagella and are enclosed in a capsule that protects them from phagocytes. Streptococci can live and reproduce without oxygen.
Streptococcus viridans remain pathogenic in the external environment for a long time, tolerate high and low temperatures well, and remain viable for a long time even in the absence of moisture. When treated with disinfectant solutions during boiling, the bacteria die after half an hour.
Normally, viridans streptococci make up approximately 40% of all bacteria that live in the human body.
Seeding and virulence
Streptococci viridans have low virulence. They do not produce toxins, and they rarely cause serious illnesses and only in the presence of provoking factors.
Author:
Trofimova Irina
Didn't understand the article or need help? Ask a question now and get an answer.
To identify bacteria, a swab is taken from the throat and throat. Microorganisms may be present in venous blood, sputum, urine, depending on the location of the infectious process.
After collecting the biomaterial, inoculation is done, serum or blood agar is used as a nutrient medium, and a bacteriological study is carried out. In liquid, viridans streptococci form a cloudy precipitate; in solid media, they grow into small grayish-green colonies.
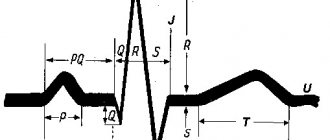
Additional diagnostic methods - PCR, clinical blood and urine tests, ultrasound, ECG - allow you to assess the general condition of the internal organs.
Normally, the number of viridans streptococci in the throat is 10 to 4 units.
General therapeutic measures
Streptococcal infection is dangerous due to its complications, so its treatment should be started immediately. Treatment of infection caused by Streptococcus viridans consists of treating the root cause—the microbe—and eliminating clinical manifestations that worsen the well-being of patients. For this purpose, traditional medicinal and physiotherapeutic methods, as well as traditional medicine, are used. An integrated approach gives the most positive results. On average, a course of medication lasts 7-10 days. Treatment is carried out under the supervision of specialists - ENT doctors, infectious disease specialists or pulmonologists.
Treatment of streptococcal infections requires the use of antibiotics. Patients are prescribed penicillins Augmentin, Amoxicillin and cephalosporins Ceftriaxone and Ceftazidime. Antibiotic therapy is carried out until complete sanitation, after which the patient is retested for microflora.- Gargling with streptococcal bacteriophage, Miramistin, Chlorhexidine.
- Enterosorbents for detoxification – “Polysorb”, “Smecta”.
- To restore the disturbed intestinal microflora, pre- and probiotics are taken - “Linex”, “Acipol”, “Bifidumbacterin”.
- Immunostimulating drugs – “Likopid”, “Bronchomunal”, “Polyoxidonium”.
- Desensitizing agents for relieving swelling - “Tavegil”, “Zirtek”, “Loratodine”.
- Antipyretic and anti-inflammatory drugs - Paracetamol, Nurofen.
- Vasoconstrictor nasal drops - “Tizin”, “Xylometazoline”.
- Detoxification and dehydration consists of drinking a sufficient amount of fluid, taking Regidron orally, and parenterally administering saline and glucose.
- Rinsing the mouth and throat with infusions and decoctions of medicinal herbs.
- Ingestion of natural antiseptics - honey, propolis, garlic, onions.
- Enriching the diet with vitamins – vegetables and fruits.
- Rosehip decoction and cranberry juice saturate the body with vitamin C and increase immunity.
- A decoction of blueberry leaves and berries is a good antiseptic and immunostimulant.
- Treatment of endocarditis is carried out through surgery - microbial vegetations on the valves are removed, the thickened endocardium is excised, and then plastic surgery is performed.
Particular attention should be paid to the care of patients, their nutrition and compliance with the drinking regime.
Streptococcus viridance forum. View full version : Streptococcus viridans - dangerous?
Julia*
According to the culture results, Staphylococcus aureus 10*2 and Streptococcus viridans 10*5, penicillin-resistant, were cultured from the throat. I read in this forum that this is not the same streptococcus that can cause complications of chronic tonsillitis. But when I try to look on the internet what kind of beast this Str. viridans - one of the first links - to the Russian Medical Journal, with an article where it is written that this particular species is the main causative agent of infective endocarditis and other serious diseases. I’m afraid of something... My throat has been hurting for two months now, washing the tonsils and all sorts of rinses only help a little, streptococcus is apparently blooming in full bloom, and they haven’t prescribed anything else for me yet. The throat is not even as worrying as the possibility of complications due to the unsuppressed growth of streptococcus.
Anton Verbine
According to the culture results, Staphylococcus aureus 10*2 and Streptococcus viridans 10*5, penicillin-resistant, were cultured from the throat. … …it would be strange if it didn’t fall out of the throat. Viridans streptococcus (more precisely, several dozen species of streptococci that partially hemolyze blood in culture) is a normal inhabitant of the oral cavity. That is why it is a common causative agent of endocarditis - the oral cavity with frequent microtraumas when eating - is statistically often the entry point for infection, which develops in people with some predisposition. It gets into everyone’s blood, more often or less often. A throat culture is usually done to look for another beta-hemolytic streptococcus (alpha-hemolytic streptococcus). The causative agent of sore throat, and sometimes rheumatism and nephritis. Everything else in this analysis is from the evil one.
Julia*
Thank you for reassuring me! No, they didn’t find beta-hemolytic... only Staphylococcus aureus and this streptococcus, nothing else was written. Both, as I understand it, are always normal - but what then causes the infection? My throat hurts and won’t go away on its own.
Tamagod
I was also found out about the presence of Str. viridans 10*5, instead of the prescribed 10*3 they prescribed a course of physio (quartz) and ampicillin tablets 0.500 each, I don’t have a sore throat, nothing, it’s just that the constant swallowing of saliva has been going on for six months, along with the feeling of its excess accumulation. I went to one hospital where, without any tests at all, they diagnosed sinusitis (!), they injected me with cefazolin for 2 weeks with the same physio, it didn’t bring any results, now I’m at the stage of re-treatment, already in another hospital. I have a question for Yulia: did you somehow cure your throat? and a question to the doctors: am I sick or not? if there is any discomfort in the throat, it means you are sick.. how can you get infected? Should my loved ones (wife and son) get checked?
Tamagod
...it would be strange if it did not fall out of the throat. Viridans streptococcus (more precisely, several dozen species of streptococci that partially hemolyze blood in culture) is a normal inhabitant of the oral cavity. That is why it is a common causative agent of endocarditis - the oral cavity with frequent microtraumas when eating - is statistically often the entry point for infection, which develops in people with some predisposition. It gets into everyone’s blood, more often or less often. A throat culture is usually done to look for another beta-hemolytic streptococcus (alpha-hemolytic streptococcus). The causative agent of sore throat, and sometimes rheumatism and nephritis. Everything else in this analysis is from the evil one. If this is normal, why then was I prescribed an antibiotic and a course of physio? normal content is 10*3, but mine is 10*5
dr.Ira
If this is normal, why then was I prescribed an antibiotic and a course of physio? This is for the doctors who prescribed “treatment” for you. Let them explain why it is needed. Normal content is 10*3, and I have 10*5. Under normal conditions (I mean normal modern recommendations and guides, and not the standards of the Muhosransky University), no one counts streptococci and staphylococci in the nasopharynx.
Tamagod
This is for the doctors who prescribed “treatment” for you. Let them explain why it is needed. Under normal conditions (I mean normal modern recommendations and guides, and not the standards of the Mukhosran University), no one counts streptococci and staphylococci in the nasopharynx.
Preventive procedures
Specific prevention of streptococcal infection has not currently been developed. To prevent the development of pathology, experts give the following recommendations:
- Observe the rules of personal hygiene: regularly wet clean the room, wash your hands before eating, keep household items, dishes, and children's toys clean.
- Temper yourself, lead an active lifestyle, engage in feasible sports.
- Eat nutritiously and properly, include foods enriched with vitamins and microelements in your diet, prepare fresh meals every day, monitor the expiration dates of raw materials and products.
- Fight bad habits, give up excessive and frequent consumption of alcoholic beverages, do not smoke, and avoid passive smoking.
- Timely identify and isolate patients in a hospital for adequate and comprehensive treatment under the supervision of specialists.
Streptococcus viridans can peacefully coexist with people. The development of pathology occurs when immunity decreases or microbes with pathogenic properties penetrate from the outside. In the absence of treatment, streptococcus from its traditional foci - the pharynx and throat - descends into the lower parts of the respiratory tract - the bronchi and lungs, and also penetrates through the bloodstream into other organs. Timely and adequate therapy makes the prognosis of the pathology favorable, preventing life-threatening complications from developing.
Streptococcus in the throat treatment forum. View full version : Hemolytic streptococcus
Arteum
Hello! A throat swab showed the presence of Streptococcus pyogen haemolytan. The fact is that I have reactive arthritis (the joints of my legs hurt, mainly) and rheumatologists sent me to an ENT specialist. ENT put: xr. tonsillitis, carriage of hemolytic streptococcus. What kind of infection is this and how to get rid of it and is it necessary, and most importantly, can it cause arthritis? Thank you!
dr.Ira
What kind of infection is this and how to get rid of it and is it necessary? Necessarily. The drug of choice is penicillin. can it cause arthritis? Alas! Maybe.
Arteum
Need to. Necessarily. The drug of choice is penicillin. Thanks for the answer! Is it really that simple? And what will really lead to freedom from streptococcus? Why was I prescribed local treatment - washing the lacunae with hexoral, lubricating the pharynx, rinsing with malavit and also lysobact? After this, lubricate with rivanol and IRS-19-zev. It's too much? I asked the nurse at the clinic if it was possible to kill the bacterium with an antibiotic, she said if everything were so simple... and that now I would need to regularly wash the lacunae... But I thought, another bacterium that cannot be gotten rid of. Maybe then I should just take penicillin? This is very, very important for me, because the arthritis is already bad, it’s difficult to walk, my feet hurt, and now I want to eliminate as many chronic infections as possible.
Anton Verbine
Is it really that simple? And what will really lead to freedom from streptococcus? Why was I prescribed local treatment - washing the lacunae with hexoral, lubricating the pharynx, rinsing with malavit and also lysobact? After this, lubricate with rivanol and IRS-19-zev. It's too much? I asked the nurse at the clinic if it was possible to kill the bacterium with an antibiotic, she said if everything were so simple... and that now I would need to regularly wash the lacunae... But I thought, another bacterium that cannot be gotten rid of. Maybe then I should just take penicillin? This is very, very important for me, because the arthritis is already bad, it’s difficult to walk, my feet hurt, and now I want to eliminate as many chronic infections as possible. ...Unfortunately, it’s not even simple at all. Penicillin (“drink” - if you have V-penicillin, but usually “prick”, or get a course of another “penicillin” antibiotic in tablets as prescribed by a doctor) - will indeed destroy your streptococcus. However, nothing guarantees that you will not get it again, as well as curing chronic tonsillitis, which, apparently, otolaryngologists are planning to treat. And it is completely unlikely that the removal of streptococcus (as well as other “chronic infections” - with the exception of chlamydia - if any) will somehow affect chronic arthritis of the feet. Streptococcus pyogenes sometimes actually causes reactive arthritis (and rheumatism) - but usually arthritis of large joints, and in childhood and adolescence. Therefore, your arthritis should be treated by a specialist rheumatologist.
A study to identify the causative agent of streptococcal infection (Streptococcus pyogenes), during which the genetic material (DNA) of streptococcus in a sample of biomaterial is determined using the real-time polymerase chain reaction method.
Synonyms Russian
Streptococcus pyogenes, group A beta-hemolytic streptococcus, GABHS, group A beta-hemolytic streptococcus, β-HSA [real-time polymerase chain reaction, real-time PCR].
English synonyms
S. pyogenes, Group A streptococcus, GAS, β-hemolytic streptococcus group A, β-hemolytic streptococcus group A.
Research method
Real-time polymerase chain reaction.
What biomaterial can be used for research?
A swab from the pharynx (oropharynx), a swab from the nasopharynx, a urogenital scraping.
General information about the study
S. pyogenes is a Gram-positive, spherical bacterium that is the causative agent of acute pharyngitis and impetigo, as well as a spectrum of more severe destructive diseases such as pneumonia, sepsis and septic arthritis, toxic shock syndrome, cellulitis and necrotizing fasciitis.
Traditionally, to confirm the diagnosis of streptococcal infection, bacteriological seeding of biomaterial on special media is used. The biomaterial can be discharge from the tonsils or nasopharynx (if acute pharyngitis is suspected), or sputum (for pneumonia). As a rule, the result can be obtained only after a few days, which is associated with a delay in making an accurate diagnosis and prescribing specific treatment. However, it has been revealed that timely diagnosis and specific treatment not only reduce the duration of the disease and the intensity of symptoms, but also reduce the risk of developing complications such as peritonsillar abscess, otitis media, acute rheumatic fever and post-streptococcal glomerulonephritis (for acute pharyngitis), streptococcal sepsis (for pneumonia ), joint destruction and disability (with septic arthritis). Empiric therapy with penicillin antibiotics is based on the premise that S. pyogenes is the main bacterial causative agent of acute pharyngitis (5-15% of cases in adults and 20-30% in children). It should be noted that acute pharyngitis can be caused by other bacterial or viral agents, for which the appointment of such empirical therapy is not only not justified, but is also dangerous due to the development of resistant strains of microorganisms. Such diagnostic difficulties can be overcome using RT-PCR - polymerase chain reaction - this method allows you to get an accurate result in a shorter time.
The RT-PCR reaction uses specific primers for the S. pyogenes DNA fragment. This feature makes it possible to identify only pyogenic streptococcus, and not other streptococci related to it - representatives of the normal microflora of the pharynx (Streptococcus mutans, Streptococcus viridians). In terms of specificity, RT-PCR is not inferior to bacteriological culture and is significantly superior to other methods of identifying the pathogen (for example, a rapid test for determining the antigen).
Quite often, biomaterial is taken for research during the treatment of the disease. As a result, the sensitivity of diagnostic methods decreases and the likelihood of obtaining a false negative result is higher. In such a situation, the RT-PCR method has some advantages over other types of diagnostics. This is explained by the fact that to identify the pathogen in the reaction, the genetic material of the pathogen is used - both the genomic DNA of a living microorganism and DNA fragments of a bacterium that has undergone lysis. In this case, it becomes possible to identify not only living, actively reproducing microorganisms, but also bacteria killed as a result of treatment. Unlike RT-PCR, a prerequisite for other diagnostic methods (enzyme-linked immunosorbent assay or bacteriological culture) is the presence of living microorganisms. Therefore, if the biomaterial is given during treatment, the RT-PCR method should be preferred to other diagnostic methods.
The high sensitivity of RT-PCR allows this method to be used in the diagnosis of complications of acute pharyngitis: acute rheumatic fever and post-streptococcal glomerulonephritis. Complications of acute pharyngitis are autoimmune diseases in which S. pyogenes - associated pharyngitis is a causative factor in the pathological immune response, but at the time of diagnosis of these complications it has already resolved (on its own or as a result of treatment). Therefore, it is possible to identify the pathogen through bacteriological culture of tonsil and nasopharynx discharge in patients with complications of acute pharyngitis only in a small percentage of cases. On the other hand, proof of previous S. pyogenes infection is a necessary criterion for diagnosis, and also greatly facilitates the differential diagnosis of diseases. The RT-PCR method is characterized by high sensitivity and therefore can be used in the diagnosis of complications of acute pharyngitis.
The detection of S. pyogenes in so-called sterile environments is always a pathological sign. On the other hand, the detection of this microorganism in non-sterile environments (sputum, nasopharyngeal discharge) does not always indicate the presence of a disease. It was found that about 12-20% of school-age children and 2.4-3.7% of adults are asymptomatic carriers of S. pyogenes. In such cases, the interpretation of a positive test result should be assessed taking into account the bacterial load and in combination with some other clinical and laboratory signs. Typically, asymptomatic carriage is characterized by fewer bacteria compared to active infection. Therefore, the finding of a high bacterial load of S. pyogenes in a throat swab from a patient with fever, sore throat, and painful regional lymphadenitis confirms the diagnosis of acute streptococcal pharyngitis. And, conversely, the detection of a low bacterial load of this microorganism in a throat smear in the absence of complaints and clinical picture should be regarded as asymptomatic carriage. RT-PCR is a semi-quantitative method that allows an indirect assessment of bacterial load. Therefore, it turns out to be especially useful when examining “healthy carriers” of streptococcus. Asymptomatic carriage of S. pyogenes should be suspected in a patient when streptococcus is detected after an adequate course of antibiotic therapy, as well as in family members of a patient with frequent exacerbations of streptococcal pharyngitis.
What is the research used for?
For diagnostics:
- acute pharyngitis;
- acute rheumatic fever and post-streptococcal pharyngitis in patients with or without a history of an episode of acute pharyngitis;
- asymptomatic carriage of S. pyogenes in a patient with frequent relapses of pharyngitis;
- asymptomatic carriage of S. pyogenes in family members of a patient with frequent relapses of streptococcal pharyngitis;
- community-acquired pneumonia;
- septic arthritis.
When is the study scheduled?
- For symptoms of acute pharyngitis: pain when swallowing, swelling and erythema of the pharynx mucosa, purulent discharge from the surface of the tonsils, painful regional lymphadenitis;
- for symptoms of acute rheumatic fever: migratory polyarthritis or arthralgia, a feeling of interruptions in the heart, pain in the heart, unmotivated weakness, ring-shaped erythema and subcutaneous nodules, as well as neurological symptoms in the form of choreic hyperkinesis;
- for symptoms of post-streptococcal glomerulonephritis: edema (periorbital or generalized), gross hematuria, unmotivated weakness, proteinuria less than 3.5 g/day, arterial hypertension;
- when examining a patient with recurrent pharyngitis;
- when examining family members of a patient with recurrent pharyngitis;
- when examining family members of a patient with frequent relapses of acute streptococcal pharyngitis;
- in the presence of a risk factor for S. pyogenes (associated pneumonia) such as the H1N1 influenza virus;
- with symptoms of community-acquired pneumonia: sudden onset of illness, fever, shortness of breath, chest pain, cough with purulent sputum;
- in the presence of risk factors for septic arthritis: infancy and old age, immunosuppressive therapy, somatic diseases, hemodialysis;
- for symptoms of septic arthritis: pain in the joint at rest and with movement, erythema of the skin over the joint area, impaired mobility in the joint, increased body temperature and unmotivated weakness.
What do the results mean?
Reference values: negative.
Reasons for a positive result
In the discharge of the nasopharynx and tonsils:
- acute pharyngitis;
- acute rheumatic fever;
- poststreptococcal glomerulonephritis.
In sputum:
- pneumonia;
- acute bronchitis, smoker's bronchitis.
What can influence the result?
- The use of penicillin antibacterial drugs (amoxiclav, ampicillin), cephalosporins (cefixime, ceftibuten) and macrolides (azithromycin, clarithromycin) before taking the material for analysis can lead to a negative result.
Streptococcus agalactiae treatment. Streptococcus in the vaginal microflora
Most of the normal vaginal flora is lactobacilli. Opportunistic flora include streptococci, staphylococci, candida, gardnerella, ureaplasma and mycoplasma. If the number of these microorganisms does not exceed the norm, the condition of the vagina will be satisfactory.
One of the causative agents of nonspecific inflammation is Streptococcus agalactia. The group of streptococci includes a large number of different microorganisms with similar morphological characteristics. Based on the type of growth on a nutrient medium, hemolytic, non-hemolytic and greening microorganisms are distinguished.
Streptococci of groups B and D, as well as viridans, are found in the vaginal environment. Agalactia is a beta-hemolytic streptococcus from group B. The norm for streptococci is 10 to 4 CFU/ml.
The colonization of streptococci in the vaginal environment occurs during puberty, especially at the beginning of sexual activity. Self-infection from the anal folds is also possible if, while washing, you direct movements away from the anus.
At-risk groups:
- women who have suffered premature birth;
- increased temperature during childbirth;
- anhydrous period of more than 18 hours;
- birth of a premature baby;
- underweight infants;
- C-section;
- the presence of bacteria in the urine.
During childbirth, a woman can infect her newborn. Streptococci are also transmitted through household means through shared hygiene items. A man can become infected during oral or anal intercourse.
Complications of streptococcus
The progression of any infection, including streptococcal infection, threatens the emergence of complications, especially with late initiation of therapy. The main danger of the viridans bacterium at the early stage of infection is the appearance of purulent foci on the surface of the mucosa, which increases the threat of infectiousness to others.
During the first week of illness, there is a high probability of the child developing the following pathological conditions:
- acute inflammation of the middle ear;
- infection of the membranes of the brain;
- purulent inflammation of lung tissue;
- formation of abscesses in the liver and kidneys;
- acute reaction of the body to infection (toxic shock).
Late complications are no less dangerous. Pathologies that appear 3-5 weeks after infection include damage to the heart and articular tissue structures, small joints, rheumatic heart disease, and the development of an autoimmune inflammatory process in the kidneys.
Is a vaccination against streptococcal infection necessary and when is it given?
Since 2014, compulsory vaccination of children has been carried out; children are vaccinated from 2 months of age. The age group under 5 years is vaccinated against Streptococcus pneumoniae, the bacteria responsible for the development of pneumonia (pneumococcal).
To ensure strong immunity against streptococcal infection, the vaccine is given 3 times over 4 months. Then, after 12 months, revaccination is carried out. Adults do not need to be vaccinated, since the adult body is armed with lasting immunity against pathogens.
Infections caused by streptococcus viridans are classified as seasonal diseases; in the fall and winter, a child with a weakened immune system increases the risk of infection.
If compliance with sanitary rules does not help to avoid the appearance of Streptococcus viridans in the throat, then the patient must be isolated and immediately call a doctor to prescribe antibiotics as soon as possible. In this case, you can count on a favorable prognosis and a speedy recovery.
Streptococcus viridans 10^6 koe/tamp. 24 answers
Don't forget to rate doctors' answers and help us improve them by asking additional questions about the topic of this question. Also, don’t forget to thank your doctors.
Agadzhanova Irina Yurievna
Hello! The number of bacteria found is slightly higher than normal (10⁴). In this situation, broad-spectrum antiseptics are recommended, including Miramistin, Chlorhexidine, Octinecept at least 3 times a day. During the day, you can dissolve Grammidin neo no more than 3 times a day. P.s. be healthy!
9
Agadzhanova Irina Yurievna
This temperature can be caused by the tonsils, which most likely have chronic inflammation. It is worth sanitizing them using the Tonziolor MM device, and then doing a magnetic laser on the tonsils.
6
Hello, I was diagnosed with chronic tonsillitis, I took a complete blood count: hemoglobin 137g/l, red blood cells 3.83*10″12/l; color index -0.96; leukocytes 5.0*10″9/l; ESR 7 mm/h; Eosinophils 1%; Band neutrophils -2%; Segmented neutrophils -56%; Lymphocytes - 38%; monocytes -3%; Scraping for eosinophils -3%; ECG is normal; Also, bacteriological culture for microflora and sensitivity to antibiotics + fungi revealed streptococcus viridans 10 in 9 degrees and revealed candida krusei 10 in 3 degrees, the doctor has not said anything yet, I read on the Internet about candida krusei 10 in 3 nothing has been written about it since it occurs in 1% of the population, why do I have it? What does this mean? I read on the Internet that this could mean an HIV infection, I’m very worried, I can’t sleep at night now, and the appointment is only on Wednesday, tell me what it is, I’m really looking forward to your answer, also tonsils with pus, I washed them once, the posterior lymph node is enlarged, I take lymphomyosot , I’m waiting for your answer regarding the identification of candida krusei 10v 3, thank you very much!
Treatment
Streptococcus viridans in a child's throat can only be diagnosed during a laboratory test. Modern laboratories are equipped with express tests, the use of which accurately identifies Streptococcus viridans in just a few minutes, which speeds up the start of the treatment process.
Antibiotics are recognized as the main treatment for streptococcal infections, the action of which is directed specifically against gram-positive agents.
Antibiotics
The most active agents that eradicate streptococcus include antibiotics of the penicillin group, as well as broad-spectrum drugs - cephalosporins.
- Representatives of the penicillin series have a specific property to disrupt the synthesis of the cell membrane of microorganisms. The antibiotic Augmentin, produced on the basis of the semi-synthetic substance amoxicillin, which is resistant to acids, copes well with infection.
- Drugs from the cephalosporin group have a prolonged effect. Ceftriaxone is often prescribed for the treatment of streptococcal infections. The antibiotic is highly active against the viridans group, and even acts on bacilli that have become tolerant to penicillin drugs.
During the treatment of Streptococcus viridans that has infected a child's throat, the local antibiotic Bioparox is often used.
The aerosol form of the drug based on fusafungin is easy to use, and during injection the active substance immediately reaches the surface of the pharynx infested with streptococci. Treatment must be prescribed by a doctor, since there is a certain list of contraindications and side effects.
Bacteriophages
Viridans throat infection responds well to treatment with streptococcal bacteriophage. Bacteriophages are the general name for a group of microorganisms used to produce modern antimicrobial drugs.
Bacteriophages selectively infect the cells of only certain bacteria, multiplying inside them. This results in the dissolution of bacterial structures (lysis), which is why antimicrobial agents are used as an alternative to antibiotic treatment.
Antihistamines
Medicines of this class are prescribed to adults and young patients to block a possible allergic reaction to antibiotics.
To avoid complications during antibiotic therapy, antihistamines of both early generations (Suprastin) and more modern drugs - Loratadine, Cetrin, Claritin - are suitable.
Strengthening the immune system
The rapid growth of Streptococcus viridans colonies indicates insufficient immune defense of the body. To stimulate the immune system during the treatment of a bacterial infection, regardless of its location, the patient needs the help of immunostimulants - IRS-19, Immunal, Imudon.
The most popular immune stimulant is ascorbic acid in tablets or powder. To strengthen the body's defenses, it is necessary to strengthen the diet with foods rich in vitamin C.
Restoration of intestinal microflora
The most dangerous side effect of treatment with antibacterial drugs is the suppression of intestinal microflora. To protect and restore normal functioning of the digestive organs, taking medications called probiotics is recommended.
These are medications containing adequate amounts of living organisms necessary to maintain health and prevent gastrointestinal disorders. The most effective drugs are Linex, Bifiform, Bifidumbacterin.
Traditional methods of fighting streptococcus
In the arsenal of traditional medicine there are many recipes that destroy microbes, including the viridans group. Throat diseases of streptococcal etiology are treated by rinsing the mouth with decoctions of bactericidal herbs (calendula, chamomile).
Internally, healers advise using products recognized as natural antiseptics (garlic, honey, onion, propolis). It is useful to eat a portion of apricot pulp in the morning and before bed, and eat at least a glass of currants, rich in vitamin C, every day.
No less useful in the treatment of streptococcal infections in the throat is the pharmaceutical drug Chlorophyllipt. A diluted alcohol solution is used to gargle the throat and nose; an oil solution is used to lubricate the sinuses and tonsils.
Features of treatment of newborns and older children
Streptococcus viridans in a child’s throat is especially dangerous due to the bacteria’s ability to produce toxins and aggressive enzymes. Harmful agents disrupt blood flow, suppress the immune system, causing the development of infectious pathologies.
However, under the influence of timely prescribed antibiotics, they die quite quickly. Sick newborns are treated in a hospital under close medical supervision; the course of drug therapy lasts from 7 to 14 days.
Key points in the treatment of preschool and school-age children are similar to the treatment tactics for adults for the treatment of infection caused by Streptococcus viridans:
- a course of antibiotic therapy together with probiotics;
- taking immunostimulating drugs;
- anti-inflammatory and painkillers;
- antihistamines;
- taking liquids that reduce fever and constrict blood vessels.
To speed up recovery, therapeutic measures are not prohibited from being supplemented with traditional medicine recipes, but only after approval by the attending physician. It is unacceptable to prescribe antibiotic therapy on your own. Due to poor drug choices, bacteria become resistant to antibiotics, causing treatment problems.
Streptococcus treatment. What is streptococcus
A small number of pathogenic microorganisms are part of the microflora of the human body. If the human immune system loses the ability to control the number of pathogenic bacteria, they begin to actively multiply and penetrate the blood, heart, brain, nose, and genitourinary system. To prevent this, you need to know what streptococcus is, how it is transmitted and how to treat it. As a rule, at the site where the bacteria invades the body, a serous focus of inflammation with tissue necrosis develops.
Streptococci (streptococcus) are pathogenic microorganisms of egg-shaped or spherical shape that live in humans and animals in the digestive tract and respiratory tract. Bacteria can be found on the skin, their predominant number settles in the mouth, nose, large intestine, throat, in the woman’s vagina and the urethra of the male organ. These anaerobic parasites often exist on the surface of fungi and plants. The source of infection is a sick person, possibly an asymptomatic carrier.
Kinds
Streptococcal infection is considered an opportunistic microflora, which is always present in the human body. It does not pose any danger, because its presence controls the immune system. Although, as soon as a person weakens a little (hypovitaminosis, stress, hypothermia), bacteria actively begin to multiply, release poison into the body and provoke various diseases. There are 100 known species of streptococci. For convenience, depending on the type of hemolysis of red blood cells, this genus of bacteria was divided into 3 main groups (according to Brown’s classification):
- Beta streptococci (β). They cause complete hemolysis and are pathogenic bacteria. Group A beta-hemolytic streptococcus is considered the most insidious.
- Viridans or alpha streptococci (α). Cause incomplete hemolysis.
- Gamma streptococci (γ). Non-hemolytic bacteria.
Epidemiology
Streptococcus viridans in a certain concentration is not dangerous to humans. Rather, on the contrary, bacteria prevent the invasion of other pathogens and protect the human body from dangerous microbes such as Pseudomonas.
When the number of streptococci begins to grow rapidly, pathology occurs. Replenishment of streptococcus is also possible from the outside - from sick people, especially with respiratory forms of the disease, as well as from asymptomatic bacteria carriers. Patients with respiratory disease constantly release microbes into the environment.
Sources of infection can be your own foci - inflamed sinuses or carious teeth. Mucus from the nose, flowing down the back wall of the throat, periodically causes inflammation of the throat and tonsils.
Ways of spread of infection:
- Aeration - when swallowing air containing microbes,
- Contact, including sexual - with a kiss, hug, coitus,
- Nutritional - when consuming infected food products: eggs, milk, ham,
- Transplacental - intrauterine infection of the fetus.
People's susceptibility to streptococcal infection is quite high. The disease is characterized by autumn-winter seasonality. The microbe primarily affects young children and the elderly.
Factors contributing to the development of pathology:
- Immunodeficiency,
- Post-acute ARVI,
- Hypothermia,
- Contact with a sick person
- Oncopathology,
- Long-term immunosuppression
- Concomitant chronic diseases in the stage of decompensation.
After the introduction of Streptococcus viridans into the human body, local inflammatory processes develop and the primary lesion forms. This microbe has a tropism for the epithelium of the respiratory tract, so most often the place of its localization is the upper respiratory tract. In more rare cases, the organs of the urinary and digestive systems become inflamed. Bacteria actively multiply in epithelial cells. When their number becomes prohibitive, streptococci break into the bloodstream and spread to the internal organs.
Streptococcus viridans can cause severe intoxication with dyspepsia and confusion. The cell wall of bacteria is perceived by the body as an allergen, to which autoantibodies and hypersensitivity are produced. Allergization of the body occurs, autoimmune processes develop in the form of glomerulonephritis, myocarditis, and rheumatism. Despite its low virulence, Streptococcus viridans is able to penetrate through the bloodstream even into sterile environments - cerebrospinal fluid, urine.
Diseases caused by Streptococcus viridans:
- Demineralization and destruction of hard tooth tissues with the formation of a cavity defect,
- Inflammation of periodontal tissues,
- Tonsillitis, pharyngitis,
- Otitis,
- Inflammation of the renal glomeruli,
- Urethritis,
- Cervicitis,
- Inflammation of lymph nodes, muscles, skin,
- Endocarditis.