Discharge is one of the intimate topics that worries many expectant mothers. What is going on “there”? What causes all this discharge? In the early stages of pregnancy, vaginal discharge may increase, and at the end of pregnancy, mucus with traces of blood can be one of the signs of impending labor - this is how the mucus plug that protects the entrance to the uterus throughout pregnancy comes off. Some discharge that has a specific odor and color may be a sign of infection. In this article, you will learn about the types of discharge you may encounter during pregnancy, which ones are harmless, and which ones require medical intervention.
What discharge is normal during pregnancy?
Normally, discharge during pregnancy is clear or white, usually sticky, without a distinct odor. If the discharge leaves yellowish marks on your underwear or sanitary pad, don't worry. During pregnancy, levels of the hormones estrogen and progesterone rise and blood flow to the vagina increases, so there may also be more discharge, especially in the second trimester. In fact, the discharge protects the fetus from infection, because this is how the vagina naturally cleanses itself and removes dead cells. After the full gestation period (at the 39th week), the discharge may become mucous. This is a mucus plug, which we will talk about in more detail below.
Color
Vaginal discharge may vary in shades and colors of impurities, namely:
- Light yellow discharge during pregnancy, which is not accompanied by any other signs of the development of pathological processes, is the norm. This secretion is associated with the formation of a mucus plug, the purpose of which is to protect the fetus from various external infections.
- Dark yellow discharge during pregnancy is pathological, as it represents an accumulation of pus, thereby indicating that the microflora is actively multiplying Escherichia coli or staphylococcal coli.
- Secretion during pregnancy in the early stages of a yellow-green color is pathological and can signal vaginal dysbiosis or genital infections of bacterial origin, for example, trichomoniasis. In addition to color, other symptoms may also indicate the presence of diseases, such as discomfort, burning or the presence of an unpleasant odor.
- Pregnant women may experience yellow-brown mucus in the first weeks, this is due to the fact that the embryo is attached to the wall of the uterus, and the woman may have scanty bleeding. But if the brown tint predominates, then this feature should alert you, because this may be a signal of pathologies such as: ectopic pregnancy, frozen pregnancy, cervical erosion, detachment of the ovum, spontaneous miscarriage.
- Yellow secretion with bloody impurities usually occurs at the very beginning of pregnancy, when the fetus is attached to the wall of the uterus. But also the occurrence of such secretion may indicate a slight placental abruption, ectopic or frozen pregnancy, the presence of fibroids, cervical erosion, genital injuries, and so on.
- White-yellow discharge during pregnancy can be either a natural process or a sign of an allergy to underwear made of synthetic material, hygiene products, or be a sign of thrush. It is worth noting that thrush occurs in approximately 30 percent of pregnant women.
Candidiasis during pregnancy is a fairly common phenomenon, its main symptoms are:
- cheesy white-yellow discharge with a sour odor;
- itching, burning sensation;
- The labia minora swell.
Candidiasis requires timely treatment, since a fungal infection can be transmitted to the baby.
Is discharge a sign of pregnancy?
As a rule, discharge is not a sign of pregnancy, but at the very beginning of pregnancy, spotting is sometimes observed. This is implantation bleeding that occurs when a fertilized egg attaches to the lining of the uterus. In early pregnancy, this discharge is usually pink in color, slightly paler than menstrual bleeding.
By the way, if you just recently found out that you will become a mother, we recommend calculating your approximate due date using our calculator.
Discharge in early and late stages
To summarize, we can say that these discharges during pregnancy are not always a sign of pathology. They can arise against the background of the individual characteristics of the female body and are regarded as a variant of the extreme norm.
At the beginning (in the first month) and up to the 6th week of pregnancy, the yellow discharge is uniform, transparent, and odorless. From the 7th week their volume increases, mucus predominates in the discharge.
Week 8 is a period of special control. Often it is at the end of the 8th month of pregnancy that candidiasis occurs. The development of thrush is associated not only with changes in immunity, but also with an increase in pH, which creates favorable conditions for the development of fungi.
From the 13th week, the dominant role in the hormonal sphere is given to estrogens, under the influence of which the discharge becomes more abundant and watery. If there are no signs of infection and the appearance of blood, there is no need to sound the alarm. This condition will accompany the entire 2nd trimester. The appearance of dark or brownish impurities in the discharge is unacceptable. You need to immediately notify your doctor.
The presence of yellow discharge in the last weeks of pregnancy (in the third trimester) is no longer a sign of pathology. However, their density increases again, which is a clear clinical sign of the onset of labor.
What discharge during pregnancy is a sign of infection?
Unfortunately, during pregnancy the body is more susceptible to vaginal infections. The reason is that due to pregnancy hormones, the composition of the vaginal flora changes, so the body is more susceptible to diseases such as thrush and bacterial vaginosis.
Any change in the color, odor, or consistency of vaginal discharge may indicate an infection, so be on the lookout for it during pregnancy. Changes also occur with bacterial vaginosis - because of it, the discharge, as a rule, acquires a sharp fishy odor and a gray, white or green color. With thrush, the discharge may be viscous, lumpy, and white. If you notice these symptoms or if anything else is causing you concern, discuss it with your doctor so that you can decide on treatment. An untreated vaginal infection can spread to the uterus, and this is already dangerous for the health of the fetus.
Causes of yellow discharge during gestation
Various factors can provoke the appearance of yellow vaginal leucorrhoea during pregnancy:
- External reasons. These include allergies caused by the use of inappropriate intimate products, sanitary pads, and wearing poor-quality underwear).
- Infectious diseases (venereal pathologies).
- Internal inflammation. The cause of the formation of yellow discharge can be inflammatory pathologies of the bladder, uterus and other genitourinary organs.
- Physiological features. In the female body during gestation, various hormonal changes occur that affect the functioning of the reproductive glands.
- Infected abortion. These are the consequences of surgical interventions that led to infection of the uterine cavity or were carried out in the presence of contraindications. Remnants of the fertilized egg can also provoke infection of the uterine cavity.
A woman has vaginal discharge throughout her life. This process does not stop during pregnancy. Their color, consistency and quantity depend on the period of gestation, characteristics of the female body, the presence of infections and other factors.
In addition, the following diseases of the genitourinary system can contribute to the appearance of yellow leucorrhoea during pregnancy:
- Colpitis. First, the membranes of the vaginal cavity react to genital infections. The cause of inflammation of the vagina can be the pathogenic activity of streptococci, staphylococci, chlamydia, mycoplasma, trichomonas and other bacteria.
- Cervicitis. The appearance of yellow leucorrhoea during pregnancy may be a manifestation of inflammation of the uterine cervix. The causative agents of the pathology are the same bacteria as in colpitis, but they are localized in the uterus or cervical canal.
- Thrush (candidiasis). White or yellow profuse discharge, accompanied by itching, may be a symptom of a fungal infection of the genitourinary system. The formation of thrush can be caused by wearing synthetic clothing, using inappropriate intimate products, taking antibiotics, decreased immunity, etc. Since candida bacteria are opportunistic microorganisms of the vaginal microflora, pregnancy leads to their active growth.
- Bacterial vaginosis (gardnerellosis). The disease develops as a result of a disturbance in the vaginal microflora, which is characterized by the replacement of normal lactoflora by anaerobic bacteria and gardnerella. The main reason for the appearance of vaginosis is hormonal changes occurring in the mother's body.
When should you see a doctor?
If the color or consistency of the discharge changes or if there is an unpleasant odor, consult a doctor. You should also consult a doctor if you experience itching or pain when urinating. Watery or bloody discharge may mean your water is breaking or you have a mucus plug. If you are less than 37 weeks pregnant, this may indicate the onset of preterm labor. In this case, you should consult a doctor at the first symptoms. If at any point during your pregnancy you experience vaginal bleeding (more than minor spotting), see your doctor or call an ambulance right away.
Normal or pathological?
Basically, discharge in large quantities occurs:
- before menstruation,
- in the middle of the cycle (when a mature egg is released from the ovary),
- when taking hormonal drugs,
- during pregnancy/gestation
- during lactation (breastfeeding a newborn)
The disease is indicated by a change in the color of the discharge. They may turn greenish, gray, or dark yellow. Often when the color changes, their smell also changes. For example, someone may have discharge that smells like rotten fish. The following symptoms also indicate pathology:
- stomach ache
- itching and other unpleasant sensations in the vagina
- burning sensation when urinating
During pregnancy, from the very first weeks, a woman’s immunity weakens. That's nature. This is necessary so that the mother’s body, which considers the fetus a foreign body, does not reject it. Today, the protective forces of most organisms are already reduced due to unfavorable environmental conditions and many other factors. Therefore, during pregnancy, immunity can be very low.
What other changes in the nature of discharge should you pay attention to?
Immediately before, during and immediately after pregnancy, women sometimes experience the following changes in the nature of their discharge:
- Discharge during ovulation.
The amount of discharge (leukorrhea) depends on the day of the menstrual cycle. The amount of discharge increases immediately before ovulation (the most favorable time for conception), and it usually has a liquid consistency. Immediately after ovulation, the discharge becomes thicker and less noticeable, and its volume decreases. These fluctuations are usually noticed by women who purposefully plan a pregnancy and monitor ovulation periods.
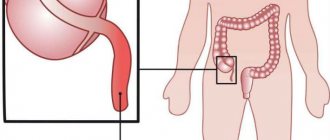
- Mucus plug.
A mucus plug, as the name suggests, is made up of mucus that accumulates in the cervix, blocking the entrance to the uterine cavity. Its purpose is to protect the fetus from infection. Just before contractions begin, the cervix dilates and the plug comes out of the vagina. The color of this mucus is usually clear or slightly pinkish with traces of blood, and its consistency is usually thicker than normal pregnancy discharge.
- Amniotic fluid.
A few hours before the onset of contractions, the amniotic sac breaks and the water breaks. This does not always happen on the same scale as in the movies: for some, the water recedes in a small trickle, for others the volume of water may be more significant, and still others do not notice anything at all.
- Lochia.
Immediately after natural childbirth or cesarean section and separation of the placenta, new discharge appears - lochia. This is mucus with blood that is released for several days after birth. At first it is a thick red discharge, which gradually fades and becomes yellowish or white. After a cesarean section, the volume of lochia is slightly less than after a natural birth. Lochia usually lasts four to six weeks after birth.
During pregnancy, the body undergoes many amazing changes. To find out what's next for you and your baby, download our special pregnancy guide.
Prevention and treatment of yellow leucorrhoea during pregnancy
Yellow vaginal leucorrhoea during gestation may be a reaction of the mother's body to ongoing hormonal changes or a manifestation of inflammation of the genitourinary system. A doctor can determine the cause of pathological leucorrhoea after a laboratory examination of a vaginal smear. If pathogenic microorganisms are identified, bacteriological culture will be carried out, which will determine the sensitivity of the detected virus to antibacterial agents. Based on the diagnostic results, appropriate therapy will be selected.
The choice of the most appropriate drug should be made by a doctor (self-medication is unacceptable), since the list of approved medications during pregnancy is strictly limited. Treatment of the identified pathology is carried out from the second trimester and is developed taking into account the nature of the detected disease, the duration and characteristics of the course of pregnancy, the individual characteristics and health status of the patient.
To prevent the appearance of pathological vaginal discharge during gestation, pregnant women should do the following:
- Adhere to a healthy lifestyle before and during pregnancy (engage in moderate physical activity, give up bad habits, etc.).
- Eat a balanced and rational diet, including foods rich in vitamins and micronutrients in your daily diet. This will help increase the body's protective properties and strengthen the immune system.
- Maintain a sleep and rest schedule, avoid nervous stress and psycho-emotional stress.
- Adhere to hygiene rules.
- Use barrier contraceptives to prevent sexually transmitted infections.
Usually, yellow, odorless and itchy discharge is normal during pregnancy. If the consistency, shade or amount of vaginal leucorrhoea changes or other pathological symptoms appear, you should consult a doctor who will select the safest and most appropriate therapeutic tactics.
Attention!
This article is posted for informational purposes only and under no circumstances constitutes scientific material or medical advice and should not serve as a substitute for an in-person consultation with a professional physician.
For diagnostics, diagnosis and treatment, contact qualified doctors! Number of reads: 7002 Date of publication: 03/30/2018
Gynecologists - search service and appointment with gynecologists in Moscow
Prevention measures
Who may experience white discharge? Any woman. Why? Because she doesn't lead a healthy lifestyle. A pregnant woman should exercise, adhere to the principles of proper nutrition, etc. This is necessary to minimize the risk of developing various diseases. The components of a healthy lifestyle can be presented as follows:
- Balanced nutrition in terms of quality and quantity. The diet should be rich in vitamins, minerals, valuable proteins, all micro- and macroelements. A woman should eat as many fruits and vegetables as possible.
- Moderate constant physical training. The purpose of the exercises is to maintain the body in tone, prevent complications from the fetus and increase the overall resistance of the body.
- Only protected sexual intercourse. Any contact can lead to infection. The infection can develop not only in the vaginal area and external genitalia, but also penetrate through the softened, dilated cervical canal, easily overcoming the mucus plug. In such a situation, infection of the fetus and many other complications are possible.
- Careful hygiene. Daily toileting of the genitals twice a day provides complete protection of the vaginal microflora from pathogenic and conditionally pathogenic microorganisms.
- Careful selection of underwear. A woman's clothing should be made exclusively from natural materials. It is not recommended to wear synthetic items or clothes purchased for the first time to prevent allergic reactions.
If it was not possible to avoid the appearance of negative symptoms and yellowish discharge is detected, you should consult a doctor. He will prescribe a full course of examination and select further treatment. It is strictly forbidden to engage in healing on your own.
Causes
There are many reasons why this problem occurs, so it is almost impossible to prevent its occurrence. Among the most common reasons for its formation are the following:
- mechanical impact on the lower abdomen (for example, injuries, bruises);
- hormonal deficiency (progesterone deficiency);
- genetic abnormalities of the embryo (developmental defects);
- stress;
- heavy physical activity;
- diseases of the uterus (chronic endometritis, endometriosis, fibroids, uterine malformations (septum, duplication, additional horn, etc.);
- disorders of the blood coagulation system;
- autoimmune aggression (eg, antiphospholipid syndrome);
- sexually transmitted infections, etc.;
- vascular pathology.
Also, noise and vibration (occupational factor) and even the environment can contribute to the formation of a hematoma.
Retrochorial hematoma can be suspected when spotting bloody discharge from the genital tract appears, but it is often an incidental finding during ultrasound, not accompanied by any symptoms. The presence or absence of symptoms is largely due to the location of the hematoma: if it is located high, in the area of the fundus of the uterus, it does not manifest itself in any way, only slight aching pain in the lower abdomen is possible. If the hematoma is located low, at the edge of the ovum, it often empties and “scares” the woman with bloody discharge from the genital tract. Sometimes these discharges can be quite copious, especially if a vessel in the uterine wall is damaged during the formation of a hematoma. And the blood is released liquid and scarlet.
Brown discharge from the genital tract in the presence of a hematoma is considered, as strange as it may sound, a good prognostic sign, since in this way the hematoma empties and disappears. If the discharge from the genital tract is abundant and scarlet, this is already a serious situation - this may indicate an increase in the area of detachment, and, accordingly, an increased risk of threatened miscarriage.