Author: Sozinova A.V., obstetrician-gynecologist, has been in continuous practice since 2001.
Scanty menstruation, or hypomenorrhea, is a reduced amount of bleeding during menstruation (50 ml or less). Hypomenorrhea refers to menstrual irregularities and can be a symptom of many diseases.
Normally, menstrual blood loss is 50-150 ml, duration is from 3 to 5 days, the menstrual cycle lasts 21-35 days, and there is no severe pain.
Scanty periods are often combined with oligomenorrhea (shortened menstruation - less than 3 days), opsomenorrhea (rare menstruation, once every 2-3 months) and spaneomenorrhea (2-3 times a year).
Types of hypomenorrhea
There are primary and secondary hypomenorrhea. They talk about primary hypomenorrhea when a young girl’s periods are scanty from the very first arrival and remain so even after a year.
Secondary hypomenorrhea is indicated by a decrease in menstrual blood loss in mature women after a period of normal menstruation.
Causes
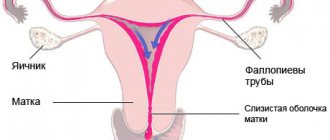
A multifunctional system is involved in the regulation of the menstrual cycle: cerebral cortex – hypothalamus – pituitary gland – ovaries – uterus. Any failure at any level will lead to a disorder of the menstrual cycle, including scanty menstruation. Hypomenorrhea can be caused by both physiological and pathological reasons.
Physiological causes of scanty periods:
- the formation of menstruation in adolescents throughout the year;
- premenopausal period;
- lactation.
All of these factors are associated with a physiological imbalance of sex hormones in the body, that is, in adolescence, the optimal production of estrogen and progesterone has not yet been established, and in premenopausal age there is a natural depletion of ovarian function. During the period when menstruation has resumed after childbirth, but the woman is still breastfeeding, hypomenorrhea can be observed in her due to the increased content of prolactin in the blood (the hormone prolactin is increased during lactation).
Pathological causes of scanty periods:
1) affecting the uterus and the functional (menstruating) layer of the endometrium:
- abortions and curettage of the uterine cavity;
- inflammatory diseases of the uterus and appendages;
- tuberculosis of the genital organs;
- operations on the uterus (removal of myomatous nodes, partial removal of the uterus, cesarean section);
- sexually transmitted diseases;
2) disrupting the production of sex hormones in the ovaries:
- injuries and surgeries on the pelvic organs (for example, removal of part of an ovary with a cyst);
- endocrine diseases, including PCOS and obesity;
- autoimmune diseases;
- genital infantilism and developmental defects;
- occupational hazards (radiation, chemicals);
3) leading to an imbalance of sex hormones released in the pituitary-hypothalamic system (brain):
- intoxication and poisoning;
- sudden and significant weight loss (anorexia, dieting, excessive exercise);
- lack of vitamins, anemia;
- mental trauma, constant stress, depression;
- brain tumors and injuries;
- autoimmune diseases;
- influence of hormonal contraception;
- major bleeding during traumatic childbirth;
- improper functioning of other endocrine organs.
Normal or disease?
Some women do not attach any importance to the peculiarities of their cycle. And in vain. If you want to have children and maintain health for many years, you need to be attentive to the features of your critical days. The gynecologist records menstrual dysfunction if a woman’s cycle deviates from the following norms:
- no pain or slight pain during menstruation
- Duration of critical days is at least 3 days
- the interval between menstruation is from 21 to 35 days
- During menstruation, 50 to 150 ml of blood is released
It is advisable to create a special table to enter the start date of critical days, the duration of the monthly cycle and other factors that were mentioned above. You can also take your basal temperature to know if your ovarian function is normal. Basal temperature is usually measured by those who suspect infertility or those who want to become pregnant in the near future.
Hypomenorrhea is a period during which an unusually small amount of blood is released. These may be traces or drops of blood. They can be light brown or dark brown in color. And this is not the norm. Hypomenorrhea indicates the presence of a certain pathology that needs to be detected.
Scanty periods are not a pathology only during the formation and waning of the cycle. These are two periods in the life of a woman/girl. At menarche, menstruation is scanty. The cycle is established in about a year. Its unevenness cannot be considered a deviation during puberty.
Types of scanty periods:
- opsomenorea (cycle duration from 1.5 to 2 months)
- hypomenorrhea (blood discharge less than 50 ml)
- oligomenorrhea (duration of critical days is up to 3 days)
- spanimenorrhea (menstruation comes only 2-4 times a year)
The decline of reproductive function is called premenopause in medicine. As noted above, scanty periods during this period are the norm. The ratio of hormone levels in the body changes. A woman enters premenopause at age 45 or older. But in recent years, increasingly “younger” cases of premenopause have been recorded.
Hypomenorrhea occurs:
- primary
- secondary
Primary is registered when the girl has never had her usual period. Secondary means that menstruation was normal, and one day it became scanty. Primary hypomenorrhea can occur in the presence of congenital pathology of the genital organs. But these are extremely rare cases. The reason for the first meager critical days may be the abnormal development or underdevelopment of the girl’s genital organs. Or this is a variant of the norm, and after a few months the cycle will already be stable, and the discharge will be in sufficient quantities.
Manifestations of scanty periods
The main symptom of hypomenorrhea is small, spotting or drop-shaped bloody discharge of a dark brown color.
Scanty periods may also be accompanied by a shortening of the duration, that is, their duration may be no more than 2 days. Collectively, this is called hypomenstrual syndrome.
In some cases, scanty periods occur against the background of pain. Women complain of pain in the lower abdomen, lower back, “shooting” in the rectum area, and sacrum. This is especially typical for adhesions in the uterine cavity and fusion of the cervical canal.
Low-grade fever (long-lasting slightly elevated body temperature up to 37-37.5 degrees) may indicate a connection between scanty menstruation and the current infectious process in a woman.
If the cause of scanty or rare menstruation is associated with disturbances in the secretion of hormones by the ovaries or pituitary gland, hypothalamus, or thyroid gland, then a woman may observe signs of premature skin aging, dryness and itching in the vagina, decreased sexual desire, irritability, tearfulness, and a tendency to depression.
Signs of improper functioning of the thyroid gland and hypothalamus (in the brain) can be weight gain in a woman simultaneously with the appearance of scanty periods, the appearance of milky discharge from the nipples, dull complexion, puffiness, drowsiness, and apathy.
general characteristics
With scanty periods, small spotting appears.
Less commonly, they appear as dark brown bloody drops. Regular daily and even ultra-thin pads work well to protect underwear during such menstruation. Often, the duration of the menstrual period is reduced to 1-2 days (oligomenorrhea), and the cycles are extended to 2-3 months (opsomenorrhea) and even longer (spaniomenorrhea). Typically, such menstruation occurs without pain and deterioration in well-being. You should consult an obstetrician-gynecologist if an adult woman, instead of the usual menstruation, experiences scanty discharge for 3 cycles or longer. A cause for concern should also be the combination of prolonged spotting (up to 2 weeks or more) with pain in the lower back and lower abdomen, which “shoots” in the sacrum, tailbone, and rectum. What is alarming is a decrease in discharge against the background of a constant or periodic increase in temperature, drowsiness, apathy, and weight gain.
Diseases that accompany hypomenorrhea
Synechiae (fusions, adhesions) in the uterine cavity
This condition is called “Asherman's syndrome” in gynecology. Numerous abortions and uterine curettages lead to the formation of intrauterine adhesions, during which the walls of the uterus were injured. Sometimes this may be just one abortion or a single curettage (for example, for the remnants of placental tissue after childbirth), but under conditions of infection. Trauma and inflammation lead to the formation of adhesions in the uterine cavity and cervix.
Women complain that before abortion or curettage they had a regular menstrual cycle, but now menstruation is scanty, usually sharply painful. In some cases, menstruation may stop altogether, and the adhesive process will progress in the uterine cavity and cervical canal.
Sex hormones in this case are produced by intact ovaries, and when examining the level of sex hormones in the blood, their compliance with the norm will be determined.
Ultrasound in the uterine cavity describes adhesions and adhesions between the walls, the uterine cavity is narrow, the mucous layer of the endometrium is insufficient in height. In conditions of adhesive and inflammatory process, the endometrium is not able to menstruate and accept a fertilized egg. Therefore, in addition to hypomenorrhea, a woman is diagnosed with infertility or recurrent miscarriage.
Fusion (atresia) of the cervical canal of the cervix
This condition is observed after operations on the cervix, during which the wall of the cervical canal is injured. For example, after removal of the vaginal part of the cervix due to the initial stage of cancer (cervical amputation according to Sturmdorff), after diathermoexcision of the cervix due to dysplasia.
After injury and inflammation, an adhesive process also develops in the wall of the cervix, making the outflow of menstrual blood difficult.
Women complain of painful cramping and nagging pain in the lower abdomen, scanty discharge, sometimes with a stagnant odor. In this case, menstruation can last for a long time - “smear” for up to 2-3 weeks, until the uterus empties through a narrow opening. If the adhesive process has led to complete overgrowth of the uterus, then hematometra occurs - a sharply painful condition in which a large number of menstrual clots accumulate in the uterus. With a hematometer, there may be a rise in temperature up to 38 degrees.
PCOS: polycystic ovary syndrome
Oligomenorrhea and opsomenorrhea are very common in patients with PCOS. Sometimes women complain of infrequent (up to once every 2-6 months) menstruation.
With scleropolycystic disease, the membrane of the ovary and follicles (sclera) thickens. At the same time, many follicles with eggs mature in the ovaries. Due to the dense membrane, the follicle cannot rupture, which should release the egg (ovulation does not occur). The ovaries increase in size, the capsule is dense, white; ultrasound describes many enlarged follicles in the ovary, like small cysts (polycystic). Many ripening and overripe follicles secrete sex hormones chaotically. Against the background of excess androgens and an imbalance of sex hormones in a woman’s body, carbohydrate metabolism is also disrupted - insulin resistance increases. Many women gain weight; blood tests reveal periodic increases in glucose levels, a condition called “prediabetes” type 2. Fluctuations in blood pressure (increase) are common.
During an external examination, you can sometimes notice signs of excess androgens: acne on the skin, increased growth of coarse hair on the face and body, sebaceous glands, fat deposition on the abdomen and shoulder girdle (male type). Such symptoms are not observed in all patients, but only in those whose blood testosterone levels are significantly elevated.
Due to the lack of ovulation and normal development of the endometrium, such women have difficulty becoming pregnant. If pregnancy occurs, hyperandrogenism (excess male hormones) can cause early loss.
Hyperandrogenism can also occur with pathology of the adrenal cortex. You can find out the cause of hyperandrogenism (ovarian or adrenal) by analyzing the hormonal levels of the blood.
Hyperprolactinemia
When the hormone prolactin increases in the blood, an imbalance occurs between the amounts of estrogens and androgens, inhibition of the production of sex hormones, impaired insulin sensitivity, and impaired lipid metabolism.
In addition to scanty or cessation of menstruation, a woman notices a general apathetic sluggish state, drowsiness, fatigue, puffiness of the face, milky discharge from the breasts, hair loss, dull skin and face color, weight gain. Blood tests show increased prolactin levels. Hyperprolactinemia often accompanies thyroid dysfunction. Such patients also have problems conceiving and bearing a child.
Inflammatory diseases of the pelvic organs: chronic endometritis, adnexitis, tuberculosis of the genital organs and other genital tract infections
Inflammatory processes of the reproductive system can occur with severe symptoms, or they can pass with virtually no symptoms. For example, with genital herpes, a woman may only remember an episode of herpetic rash in the vulva area, but in fact, in the small pelvis, adhesions in the fallopian tubes and chronic endometritis in the functional layer of the endometrium may develop asymptomatically.
In any case, after suffering an infectious process, normal organ tissue may become inoperative. In the ovaries, after inflammation, tissue with follicles that secrete hormones and eggs is replaced by connective tissue. The mucous layer of the endometrium in the uterus becomes “bald”, scanty, so it cannot be shed normally and painlessly during menstruation and replaced with a fresh layer. Such patients subsequently have problems not only with menstrual irregularities, but also with the onset of pregnancy and gestation.
Tuberculosis of the genital organs
Tuberculosis of the genitourinary tract is very difficult to suspect and establish. Characteristic signs of tuberculosis infection:
- constant low-grade fever - up to 38°C - temperature,
- mental disorders (irritability, nervousness, tearfulness),
- decreased appetite,
- chronic adnexitis or endometritis that cannot be treated.
Chronic endometritis
Constant or periodic pain in the lower abdomen, increased temperature during an exacerbation, menstrual flow with an unpleasant odor.
Chronic adnexitis
Periodic aching pain in the groin areas, increased temperature during exacerbation, heaviness and adhesions in the appendage area, which are determined during a gynecological examination, infertility.
Sexually transmitted diseases
STDs include:
- chlamydia,
- ureaplasmosis,
- cytomegalovirus infection, etc.
More often they are asymptomatic or with minor complaints (discharge from the genital tract with an unpleasant odor, itching and burning in the perineum, pain during sexual intercourse, signs of chronic endometritis and/or adnexitis).
In inflammatory diseases of the pelvic organs, it is usually always possible to identify a connection with a provocative factor: with a change of sexual partner, with the occurrence of active inflammation after an abortion or other manipulation of the uterus, with hypothermia.
Ovarian wasting syndrome and resistant ovarian syndrome
In this case, the uterus and endometrium remain healthy, but there are not enough sex hormones for a normal menstrual reaction. Disturbance in the production of sex hormones occurs at the ovarian level. In the body of a woman with these diseases, premature menopause occurs at a young age (at 35-40 and less than 35 years).
With ovarian wasting syndrome (OVS), the hormone-producing tissue in them is replaced by connective tissue. This sometimes occurs due to hereditary factors, sometimes after inflammation in the ovaries, after a toxic effect on the body. A woman who has previously menstruated and may even have given birth notices that her periods become more and more scanty, and then gradually stop altogether. When examined by a gynecologist, the uterus and ovaries are reduced in size. Follicles in the ovaries are not visualized at all on ultrasound. An analysis of anti-Mullerian hormone in the patient's blood may show that there is no supply of follicles and eggs left in the ovaries.
The content of sex hormones in the blood is at the level of menopause, a woman notices aging skin, hot flashes, fluctuations in blood pressure, anxiety, irritability, sweating, discomfort in the vagina - symptoms characteristic of menopause.
With resistant ovarian syndrome (ROS), a young woman’s menstruation also gradually becomes scanty and stops due to the lack of sufficient amounts of sex hormones in the blood. With this disease, the ovarian tissue retains the required number of follicles and eggs and is not replaced by connective tissue.
Here the cause of the disease is a failure of regulation in the brain. The ovary becomes insensitive to stimulation by hormones from above (from the pituitary gland-hypothalamus). The body signals that there is a deficiency of estrogen in the blood, but the ovaries remain insensitive to FSH (follicle-stimulating hormone) and LH (luteinizing hormone).
The clinic also observes scanty periods with their gradual complete absence and the inability to conceive. The difference between SOC and SUS: when the ovaries are resistant, follicles remain in them, and the symptoms of menopause are less clinically pronounced.
Psycho-emotional stress, excessive sports or study (“excellent student syndrome”), sudden weight loss, difficult working conditions can disrupt the release of hormones that control the ovaries by the pituitary gland and hypothalamus. Here, menstruation becomes scanty or disappears completely with a healthy uterus and ovaries. Control of the production of sex hormones is also disrupted by tumors, injuries to the pituitary gland and hypothalamus, brain infections and after hemorrhages in the brain.
How do menstruation progress during menopause?
As you already know from this article, menstruation is typical for the perimenopausal period. At this stage, there is a sharp change in the cyclicity and nature of the discharge. Let's begin our acquaintance with female characteristics from the beginning. Menstruation occurs during the following stages:
- The egg matures and is ready to be fertilized.
- It comes out of the follicle. This process is otherwise called ovulation.
- The endometrium grows inside the uterus.
- If fertilization does not occur, the egg dies.
- The endometrium is rejected and brought out. The usual menstruation comes.
When perimenopause occurs, ovulation occurs less frequently. This is due to the fact that there is not enough estrogen . Therefore, the process continues only after their level rises. During menopause, the gaps between menstruation are from 40 to 120 days. Once estrogen production stops, menstruation says goodbye forever.
Diagnostics
In order to find out the reason for scanty periods, the patient goes to see a gynecologist. What a gynecologist can see and assume at the first appointment:
- When examined on a chair, reduced size of the uterus and ovaries, dry and reddened mucosa with contact bleeding may indicate a lack of sex hormones in the body.
- When questioned, the woman herself may say that her sex drive has decreased, describe the signs of premature menopause, and complain about skin aging.
- Enlarged, dense ovaries may be a sign of PCOS.
- Increased growth of coarse hair on the face, linea alba, inguinal folds, legs and skin condition suggests an excess of male sex hormones in the blood.
- When examining the mammary glands, you can notice galactorrhea (discharge of milk secretion from the nipples) with hyperprolactinemia.
- At the appointment, the patient takes a smear to determine the degree of purity from the vagina, which may show an “senile” type of smear (as during menopause), signs of chronic inflammation.
- During the conversation, a woman can talk about previous weight gain, an abortion with an infectious complication, surgery, traumatic childbirth, chronic infections, meningitis, the fact that she was recently diagnosed with an autoimmune disease - a lot of information about the provoking factor.
Important! It is advisable to come to the appointment with a “menstrual calendar”, that is, mark in advance in red on the calendar your recent periods (so as not to painfully remember at the appointment!).
After a conversation and examination of the patient, the doctor can already roughly assume that the cause of scanty periods is in the uterus, or in the ovaries, or dysfunction of other organs must be excluded.
What examinations can a gynecologist prescribe:
- Ultrasound of the pelvic organs: you can see a picture of scleropolycystic ovaries or, conversely, reduced ovaries with the absence of follicles, a decrease in the size of the uterus, identify a hematometra in case of obstruction of the cervical canal, a picture of the adhesive process (synechias) in the uterine cavity, “bald” insufficient for the second phase of the cycle endometrium in the uterus.
- Blood tests to determine hormonal status: estrogens, progesterone, testosterone, prolactin, adrenal and thyroid hormones, FSH and LH, and others.
- Tests for the presence of ovulation in the cycle. This may be the old method of measuring basal temperature: the body temperature in the rectum is measured every morning, the values are entered into a chart; When ovulation occurs, the basal temperature rises, which is reflected in the graph. The method requires time and self-control, but there is no monetary cost. When monitoring the presence of ovulation in the ovary using ultrasound performed several times in a row (we observe the growing and bursting follicle) and urine tests for ovulation, the woman will not experience the difficulties of daily measuring the basal temperature in the rectum, but will spend money on tests and ultrasound.
- Anti-Mullerian hormone - indicates the supply of follicles and eggs in the ovaries and the patient’s prospects for childbearing and the resumption of menstruation. With premature menopause, it is practically zero.
- Blood sugar and glucose tolerance test with 100 g of glucose (for impaired insulin sensitivity).
- Visit to a phthisiatrician (if indicated, if there is a suspicion of genital tuberculosis).
- Smear tests and PCR diagnostics for sexually transmitted diseases.
- Cervical smear for oncocytology.
- X-ray of the sella turcica and examination by an ophthalmologist (to exclude a pituitary tumor);
- Consultation with an endocrinologist, ultrasound of the thyroid gland and ultrasound of the adrenal glands to exclude hormone-producing tumors in these organs.
- Tests with the introduction of estrogens, progesterone, FSH and LH from the outside (the doctor prescribes a certain drug to the patient according to the regimen and observes whether a menstrual-like reaction appears in response to its introduction or withdrawal). With their help, the doctor determines which hormone is missing and whether the uterus is healthy (can menstruate at all).
- Hysteroscopy and endometrial biopsy. These are already invasive examination methods (mini-surgery). During hysteroscopy, the uterine cavity and cervix are examined from the inside with a video camera. You can see and dissect intrauterine adhesions, diagnose obstruction of the fallopian tubes in the initial sections, scrape the endometrium for analysis (based on the results of the scraping, morphologists can describe hormone deficiency, chronic endometritis), etc.
- Laparoscopy with examination and biopsy of the ovaries is sometimes prescribed to women who are being evaluated for scanty or absent periods and infertility before undergoing IVF. During laparoscopy for infertility, signs of tuberculosis and other infectious lesions of the pelvis can be detected.
Pathologies to watch out for
Alas, one cannot always explain the vagaries of the cycle by menopause. Sometimes they are a signal that the body is being consumed by a serious disease. If you notice pathologies during the primary menopause , contact your gynecologist:
- menstruation has changed in character: the discharge has become thick, the blood is bright brown in color and smells bad;
- Uterine bleeding is normal, but blood clots of a different color are found in it. Pathology indicates a disruption of the endocrine system;
- The bleeding is short but heavy. You change the pad every 30-50 minutes, your stomach hurts a lot, you feel weak and faint.
This is not a complete list, but a basic one. If you don’t find out the cause of the changes in time, you can end up under the surgeon’s knife. And then there is curettage of the uterus, removal of benign or malignant tumors.
Very often, such problems can be avoided by non-hormonal therapy. Phytohormones replace estrogens and maintain women's health at an acceptable level. One of the remedies recommended by doctors is Lignarius. So far, there is simply no analogue to the drug. You can store estrogen for a long time, getting it from food, or take a course of pills to get rid of hot flashes, problems with abnormal discharge and fatigue.
Don't waste your health! Even if you are reassured by another article from the Internet, be vigilant and play it safe. Have a nice day!
Treatment of scanty periods
Treatment of hypomenorrhea depends on the cause that caused it.
If gynecological diseases are the causative factors in the occurrence of scanty periods, then therapy is carried out by a gynecologist. In case of tuberculosis infection, treatment is carried out by a TB doctor. In case of endocrine pathologies, treatment is carried out by an endocrinologist; in cases of mental disorders, joint supervision of the patient by a gynecologist and a psychologist is recommended, and, if indicated, by a psychiatrist.
Treatment of hypomenorrhea lasts for more than one month.
Dissection of intrauterine synechiae, fusion of the cervical canal and emptying of hematometers is carried out by hysteroscopy or hysteroresectoscopy under anesthesia. After the surgical stage of dissection of adhesions, the stage of hormonal therapy necessarily follows. A combination of estrogens and gestagens (not COCs) is usually prescribed. Against the background of hormone replacement therapy, it is necessary to achieve the growth of normal endometrium.
For PCOS, the treatment regimen includes weight loss, taking medications that improve insulin sensitivity, correction of hyperandrogenism, and surgery (incisions on the ovaries, making it possible to release and ovulate eggs). Surgical treatment is performed for infertility and the patient’s desire to conceive.
In case of hyperprolactinemia, its correction is carried out (drug “bromocriptine”, “Dostinex”). If there is a lack of thyroid hormones, they are introduced into the body for replacement purposes.
Replacement therapy with sex hormones is also carried out for the syndrome of exhausted ovaries and resistant ovaries. Without the introduction of hormonal drugs from the outside, a woman’s body will develop premature menopause.
For chronic adnexitis and endometritis, antibiotics and anti-inflammatory drugs, resorption therapy and physiotherapy are prescribed. In chronic endometritis, endometrial insufficiency is usually always present. In order for a woman to be able to menstruate and bear a child in the future, rehabilitation is prescribed after anti-inflammatory therapy. Its goal is to improve blood flow in the pelvis, restore the functional layer of the uterus, and prevent sclerotic changes in the ovaries after inflammation. The woman is recommended to undergo laser blood purification, ozone therapy, and stimulation of endometrial growth through the use of hormonal drugs and stem cell preparations.
If you are overweight or underweight, it is corrected and vitamins are prescribed according to the phases of the menstrual cycle.
Signs of hypomenorrhea
There are certain signs that characterize the development of hypomenorrhea, the appearance of which is a signal to seek advice from a specialist. Only an experienced gynecologist is able to identify the true causes of scanty periods and prescribe effective treatment. You should immediately look at the amount and color of the discharge: blood discharge that lasts longer than usual, with a volume of less than 50 ml, that has a light or dark brown color - such phenomena will signal the development of hypomenorrhea.
Additional symptoms of hypomenorrhea also include:
- headache during menstruation;
- nagging pain in the lower back;
- increased breast sensitivity;
- nausea;
- dyspeptic disorders.
More often, scanty menstrual flow is accompanied by several symptoms, but exceptions are possible when menstruation passes without accompanying symptoms. In such cases, a medical examination will be required to confirm or refute dangerous pathological factors and disease.
Hypomenorrhea can be an undesirable symptom during pregnancy. Scanty bleeding can threaten termination of pregnancy and provoke miscarriage. Light and prolonged menstruation in the postpartum period may indicate normal physiological cleaning of the uterine cavity or the presence of pathological inflammation in it.
Doctors' opinion
To maintain a normal menstrual cycle, every woman is recommended to monitor the duration, regularity and amount of discharge. To exclude or promptly identify pathologies of the female genital organs, it is necessary to regularly undergo a complete gynecological examination. Scanty, long periods are often not recognized as normal, and a woman in this condition may not even have any suspicion that she has serious pathologies and diseases of the genital organs. Prolonged periods can be observed in gynecological oncology of the ovaries and uterus, and require urgent treatment.