Corticotropin-releasing hormone is the main element that determines the body's response to stress. It is also present in diseases that cause inflammation. Too much or too little corticotropin releasing hormone can have a number of negative effects.
Alternative names for corticotropin releasing hormone:
- corticotropin releasing hormone;
- corticotropin releasing factor;
- corticotropin releasing factor;
- corticoliberin;
- CRH;
- CRF.
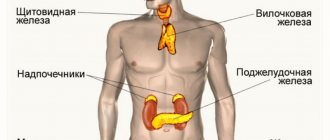
Classification of hormones
Let's look at the most famous releasing hormones:
- Inhibiting the secretory function of the pituitary gland - we are talking about somatostatin, melanostatin, prolactostatin.
- Stimulating - we are talking about melanoliberin, prolactoliberin, folliberin, luliberin, somatoliberin, thyroliberin, gonadoliberin and corticoliberin.
The listed substances, or rather some of them, can be produced by other organs, not only the hypothalamus (for example, the pancreas).
Liberians
Liberins are neurosecretes that stimulate the production of hormones in the anterior pituitary gland. They enter the gland through the capillary system. Liberins promote the release of pituitary secretions.
The hypothalamus produces the following hormones from the liberin group:
- somatoliberin;
- corticoliberin;
- gonadoliberins (lyuliberin and follyliberin);
- Thyroliberin;
- prolactoliberin;
- melanoliberin.
Next, we will consider in detail each of the above neurosecrets.
Characteristics of hormones
The hormone corticoliberin, which is responsible for anxiety, is produced by the hypothalamus. This is another important releasing factor that acts in conjunction with pituitary hormones and affects the functioning of the adrenal glands. People with a deficiency of this hormone often suffer from hypertension and adrenal insufficiency.
Gonadotropin-releasing hormone, a hormone that enhances the production of gonadotropins, is also a product of the hypothalamus. It is also called gonadotropin-releasing hormone.
The normal functioning of the genital organs cannot exist without GnRH. It is this hormone that is responsible for the natural course of the menstrual cycle in women. With its participation, the process of maturation and release of the egg takes place. This hormone is responsible for libido (sex drive). With insufficient production of this hormone by the hypothalamus, women often develop infertility. What other releasing hormones are there?
What is the hypothalamus
The hypothalamus is a part of the diencephalon. It consists of gray matter. This is a small area of the central nervous system. It makes up only 5% of the brain's weight.
The hypothalamus consists of nuclei. These are groups of neurons that perform specific functions. Neurosecretory cells are located in the nuclei. They produce hypothalamic hormones, which are otherwise called releasing factors. Their production is controlled by the central nervous system.
Each neurosecretory cell is equipped with a process (axon) that connects to the vessels. Hormones enter the bloodstream through synapses, then penetrate the pituitary gland and have a systemic effect on the body.
For a long time in medicine it was believed that the main function of this part of the brain is to control the autonomic nervous system. Hypothalamic hormones were discovered only in the 1970s. The study of their properties is still ongoing. Research on neurosecrets helps to understand the causes of many endocrine disorders.
Hormone releasing agonists: drugs
As already noted, these hormones are produced by the hypothalamus. When it is necessary to stimulate the ovaries, for example before an IVF procedure, agonists or analogues of releasing hormones are used. That is, they have the same effect on the body as its own hormone.
But there is a high probability of developing adverse reactions on the part of the female body. This happens due to a decrease in estrogen levels. The most common phenomena include:
- headache;
- excessive sweating;
- tides;
- vaginal dryness;
- mood swings;
- depressive states.
The following drugs are used:
- "Diferelin" is an artificial decapeptide, an analogue of natural releasing hormone.
- "Decapeptyl" contains triptorelin, an artificial analogue of GnRH. The half-life is longer. Often used in artificial insemination.
- "Lukrin-depot" - leuprorelin. It has an antiestrogenic, antiandrogenic effect, treats endometriosis, hormone-dependent tumors - prostate cancer, uterine fibroids. "Lucrin-depot" reduces the concentration of testosterone in men, estradiol in women, and also inhibits the incretion of FSH and LH by the pituitary gland.
- The action of the drug gradually restores the physiological secretion of hormones.
- Zoladex is a synthetic analogue of natural releasing hormone (LH). Often used in IVF. Reduces the concentration of estradiol in the blood, this is due to the suppression of LH secretion from the anterior pituitary gland.
PsyAndNeuro.ru
A positive dexamethasone test in patients with melancholic depression, indicating hyperactivation of the hypothalamic-pituitary-adrenal axis (HPA axis), has been known since my student days. Moreover, hyperactivation of the HPA axis is a powerful biological correlate of depression along with dysfunction of monoamine neurotransmitter systems and is considered one of the main links in its pathogenesis. However, over the past few decades, scientists' knowledge of how the HPA axis functions has expanded significantly. It has now become clear that in addition to the functioning of the hypothalamus, pituitary gland and adrenal glands, which occupy one of the central places in the pathogenesis of depression, a much larger number of areas of the brain and its neurotransmitter and neuropeptide systems are involved in the pathological process. This “expansion” of the theory of HPA axis hyperactivation in depression allows us to take a fresh look at the mechanisms of development of this disorder, as well as find new specific targets for drug therapy. It is also worth noting that hyperactivation of the HPA axis occurs only in 70% of patients with this disorder, and is not typical for such types of depression as menopausal, atypical or seasonal, which, on the contrary, are characterized by a decrease in the activity of the HPA axis.
Rice. 1 Functioning of the HPA axis is normal
The stimulus that caused the stressor reaches the HPA axis from the amygdala. In response to this, vasopressin and corticotropin-releasing hormone (CRH), the main regulator of the HPA axis, are released in the paraventricular nucleus of the hypothalamus. It consists of 41 amino acid residues, and its synthesis is regulated by the CRF gene. Together with vasopressin, CRH travels through the portal vein system to the anterior pituitary gland and stimulates the production of the prohormone proopiomelanocortin (POMC), which is then processed into adenocorticotropic hormone (ACTH), opioids and melanocortin. ACTH, in turn, stimulates the release of glucocorticoids (cortisol in humans and corticosterone in mice) in the zona fasciculata of the adrenal cortex, which subsequently exert negative feedback on the pituitary gland and hypothalamus through effects on mineralcorticoid (MR) and glucocorticoid receptors (GR), due to which the degree of activation of the HPA axis decreases (Marni N. Silverman, 2012).
Despite the widespread belief that the main manifestations of hyperactivation of the HPA axis are associated only with hypercortisolemia, there is increasing evidence that increased levels of corticotropin-releasing hormone (CRH), which is the main regulator of the HPA axis, have a much greater negative effect on functional systems brain.
The effects exhibited by CRH depend on the zones of its synthesis and the places of greatest concentration of its receptors. So, in addition to the hypothalamus, it is also secreted in the neurons of the amygdala, hippocampus and locus coeruleus. This neuropeptide has a local neuromodulatory effect on neurons within a few seconds after release, acting through two specific CRH receptors types 1 and 2 (CRHR1, CRHR2), which are widely distributed in various parts of the brain. It is also worth noting that the family of CRH neuropeptides, in addition to CRH itself, also includes urocortins (UCN 1, 2 3), which, like wozopressin, orexin and dynorphin, affect brain homeostasis.
Depending on the dose and time of exposure of CRH to targets, its effects also differ. For example, the release of CRH in optimal doses during acute stress in the central nucleus of the amygdala promotes memory consolidation, and in the hippocampus it increases synaptic plasticity. However, when exposed to high doses of CRH over a long period of time, hippocampal function deteriorates, manifested by neuronal damage and a decrease in the number of synapses.
Thus, during the entire episode of melancholic depression, patients exhibit elevated levels of CRH in plasma and cerebrospinal fluid. Postmortem studies of deceased people with depression have found evidence of CRH hyperactivity in the paraventricular nuclei of the hypothalamus, cortical areas, pontine nuclei, and locus coeruleus. At the same time, elevated CRH levels in depressed individuals decreased after a course of electroconvulsive or antidepressant therapy.
Moreover, in healthy individuals with a high genetic risk of developing depression in their families, the results of the combined DEX/CRH test (DEX/CRH: dexamethasone-suppression/corticotropin-releasinghormone-stimulationtest), which combines dexamethasone suppression with CRH stimulation, are between results of patients with depression and a control group of healthy volunteers. These results indicate that even small changes in HPA axis functioning have a genetic background that increases the risk of developing depression or other stress-related illnesses with age. Another study showed that individuals with depression had a significantly increased frequency of the G allele polymorphism (rs242939) of the CRHR1 gene compared to the control group. Taken together, these observations support the concept that HPA axis dysregulation, including elevated CRH levels, may be associated with genetic predisposition and represent a risk factor for the development of depression.
In depression, a decrease in the activity of neurotrophic factors is also observed. This leads to decreased synaptic connections in the hippocampus and prefrontal cortex, which correlates with depressive symptoms. A close relationship has been found between neurotrophic factors, in particular brain-derived neurotrophic factor (BDNF), and CRH, which modulates their production, production and activity.
It is also interesting that changes in the CRH receptor apparatus also affect the formation of certain symptom complexes. Thus, repeated exposure to stress leads to a change in the ratio of CRHR1 and CRHR2 towards an increase in CRHR1 in areas associated with depression. CRHR1 is able to modulate anxious behavior independently of the HPA axis, and its deficiency protects a person from the formation of negative consequences of stress, regardless of age. This is due to the fact that CRHR1 controls glutamatergic, noradrenergic and dopaminergic neural circuits, making a significant contribution to the manifestations of stress-related disorders.
This is supported by extensive evidence showing that the three major neurotransmitter systems (serotonin, norepinephrine and dopamine) closely interact and influence CRH levels. Thus, in the locus coeruleus (the most important nucleus of the noradrenalinergic system in the brain), the dorsal raphe nuclei (the most important nucleus of the serotonergic system) and in the ventral tegmental area (the most important nucleus of the mesocorticolimbic dopaminergic system) a high level of expression of CRHR1 and CRHR2 is found, and the overall level of expression of these receptors and their ratio is an important indicator of individual stress tolerance and the risk of developing depression.
For example, in the dorsal raphe nucleus, CRH has opposing effects on the serotonergic system depending on which receptor (CRHR1 or CRHR2) it acts on. Thus, activation of CRHR1 in this area leads to increased GABAergic inhibitory effects on the serotonin system, and activation of CRHR2, on the contrary, has a potentiating effect.
The influence of CRH on the formation of anhedonia, which is characterized by a decrease in activity in mesolimbic dopamine projections from the ventral tegmental area to the nucleus accumbens (ventral striatum) and further to the cerebral cortex, has also been proven. During periods of acute stress, CRH stimulates the release of dopamine in the nucleus accumbens, which is an important part of the “reward” system. However, after severe acute stress or with prolonged exposure, CRH does not stimulate the release of dopamine, which can be considered as one of the mechanisms for the formation of anhedonia.
An imbalance in the neurotransmitter systems also affects the HPA axis itself, since acetylcholine, dopamine and norepinephrine promote the secretion of CRH in the hypothalamus, and serotonin, in turn, inhibits the secretion of CRH in the hypothalamus and ACTH in the pituitary gland, which also contributes to HPA axis dysfunction. axes.
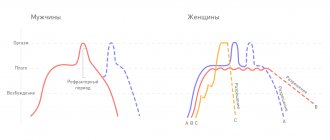
Another important feature of the physiology of depression is the disinhibition of the REM sleep phase (REM, Rapid Eye Movement), which is specifically associated with the central activity of CRH and a decrease in the level of somatotropin-releasing hormone (SRH), which regulates slow-wave sleep. dream. Thus, in one clinical study assessing the safety and tolerability of CRHR1 antagonists (R121919), EEG recordings were performed during sleep before and after 28 days of treatment. The results showed that the majority of patients with significant REM sleep stage disturbances showed improvement in depressive symptoms between 50 and 90% on the Hamilton Depression Rating Scale, while improvement in patients with normal sleep stages was consistently below 50%.
Rice. 2 Sleep disturbances in depression
Sleep disturbance in depression is characterized by disruption of slow wave sleep and increased REM sleep as a result of an imbalance between CRH and SRH (Steiger, 2003).
The generalized results suggest that disinhibition of the REM sleep phase can probably be considered as a specific indicator reflecting the central activity of CRH, with the help of which it is possible to identify patients with depression in whom it is advisable to undergo therapy with CRHR1 antagonists, which are widely used for the treatment of endocrinological diseases.
Source: Kasyanov E.D., Mazo G.E. Functioning of the hypothalamic-pituitary-adrenal axis in depression: current state of the problem. // Journal of Mental Health. – 2017. – No. 8. – P. 27 – 34.
Antagonists
Because estradiol is extremely elevated when taking hormone-releasing hormone agonists, a surge in luteinizing hormone may occur. This leads to premature ovulation and egg death. To prevent this from happening, hormone releasing hormone antagonists are used. As a result of their action, the pituitary gland can be stimulated again. Ovarian hyperstimulation syndrome does not manifest itself, but this often happened due to long-term use of GnRH agonists. Administered five days after the start of follicle-stimulating hormone use.
For therapy to be successful, all drug prescriptions must be carried out only by a specialist.
Somatoliberin
Somatoliberin stimulates the production of growth hormone by the pituitary gland. The hypothalamus produces increased amounts of this neurosecretion as a person grows. Increased formation of somatoliberin is observed in children and adolescents. With age, hormone production decreases.
Active production of somatoliberin occurs during sleep. Related to this is the widespread belief that a child grows while he sleeps. Hormone synthesis also increases during stress and exercise.
Somatoliberin is necessary for the human body not only for the growth of bones and tissues in childhood. This neurohormone is also produced in small quantities in adults. It affects sleep, appetite and cognitive function.
A deficiency of this neurohormone in childhood can lead to severe growth retardation, including the development of dwarfism. If the production of somatoliberin is reduced in an adult, then this has little effect on his well-being. There may be only slight weakness, deterioration in working capacity and poor muscle development.
Excess somatoliberin in children can lead to excessively high growth (gigantism). If this hormone is produced in increased quantities in adults, then acromegaly develops. This is a disease that is accompanied by disproportionate growth of bones and tissues of the face, feet and hands.
Nowadays, pharmacological preparations based on somatoliberin have been developed. They are mainly used for growth deficiency in children. But often people involved in bodybuilding take such drugs to build muscle mass. If the drug is used for sports purposes, you should consult an endocrinologist before using it.
Useful video
Watch the video about the hypothalamic-pituitary system:
Similar articles
- Hypothalamic statins, neurosecrets, hormones
In total, there are 7 hypothalamic statins, of which 3 have been comparatively studied. These hormones affect the genitals and can have an antitumor effect. The neurosecrets of the hypothalamus are being actively studied by scientists. Read more - Hypothalamus: structure, features, functions in humans...
The hypothalamus plays a very important role in the body, the structure of which is quite complex and not fully understood. The main functions and biological role in the human body are the production of mostly hormones. What are its features? Read more
- Diabetic polyneuropathy, its types: sensory…
Diabetic polyneuropathy often manifests itself as pain. Additional symptoms depend on its type. It can be sensory, sensorimotor, peripheral, diabetic, autonomic. Pathogenesis also depends on which species of the classification has evolved. Read more
- Hormones of the pituitary lobes: anterior, middle, posterior, their...
Hormones of the pituitary gland influence almost all vital functions of the body. The structural features of the organ include three lobes - anterior, middle and posterior. What are their functions? What is the histological and physiological significance? Read more
- Pituitary gland dysfunction: signs, symptoms...
Many factors can provoke disruption of the pituitary gland. The signs are not always obvious, and the symptoms are more similar to endocrinological problems in men and women. The treatment is complex. What disorders are associated with the functioning of the pituitary gland? Read more
Statins
Statins are hypothalamic hormones that inhibit the production of pituitary secretions. We can say that their function is opposite to the action of liberins. Statins include the following neurosecrets of the hypothalamus:
- Somatostatin. Suppresses the synthesis of growth hormone.
- Prolactostatin. Blocks the formation of prolactin.
- Melanostatin. Inhibits the production of melanotropic hormone.
Currently, the hormonal function of the hypothalamus is still being studied. Therefore, it is not yet known whether there are neurosecrets that inhibit the production of gonadotropic and thyroid-stimulating hormones, as well as ACTH. Medical science suggests that not all hypothalamic neurohormones from the statin group have yet been discovered.
STG[edit | edit code]
The gene encoding GH is located on the long arm of chromosome 17. There are also four genes homologous to it: three genes encoding different forms of placental lactogen, and a gene encoding placental growth hormone, which is secreted by syncytiotrophoblast cells. GH is secreted as a mixture of peptides with different molecular weights and charges. The main form of GH has a molecular weight of about 22,000 and is a single non-glycosylated polypeptide chain of 191 amino acid residues with two disulfide bonds. By alternative splicing, a form with a molecular weight of about 20,000 is formed, which lacks the region from the 32nd to 46th amino acid residue; it has approximately the same activity and accounts for 5-10% of circulating GH. Other forms of GH are present in serum, but their significance is unclear. About 45% of GH with a molecular weight of 22,000 and 25% of GH with a molecular weight of 20,000 form a complex with the serum GH-binding protein, which contains the extracellular domain of the GH receptor. The GH-binding protein serves as a GH reservoir, since in combination with this protein, GH breaks down 10 times slower than free GH. On the other hand, GH-binding protein reduces the activity of GH because it prevents its interaction with receptors in tissues.
Melanoliberin
Melanoliberin releases melanotropin in the pituitary gland. This is a substance that promotes the formation of melanin in epidermal cells.
Melanin is a pigment that is formed in special cells - melanocytes. Its excess causes darkening of the epidermis. Melanoliberin is responsible for skin color. An increased amount of neurosecretion is formed when exposed to sunlight, which becomes the cause of tanning.
Prolactoliberin
Prolactoliberin is a neurohormone that stimulates the production of prolactin by pituitary cells. It is necessary for the formation of milk during lactation. A sufficient amount of this hormone is very important for nursing mothers.
However, prolactoliberin and prolactin are formed in non-lactating women, and even in men. What are these hormones used for outside of lactation? There is an assumption that prolactoliberin is involved in immune reactions and stimulates the growth of new blood vessels. Some studies show that this neurosecretion has analgesic properties.
However, excess prolactoliberin is harmful. It can cause galactorrhea. This is an endocrine disorder that results in the release of milk from the mammary glands in non-breastfeeding women. In men, this disease leads to abnormal enlargement of the mammary glands - gynecomastia.
Structure of the thyroid gland
The thyroid gland is located on the front of the neck, just below the Adam's apple. The ancient Roman physician Galen first described the gland as a separate organ, and it received its name much later in the 17th century. The name of the gland comes from the Greek words “thyreos” - shield and “idos” - view, i.e. an organ that looks like a shield. The international name for this internal secretion organ is the thyroid gland. The shape of the thyroid gland resembles a butterfly or a horseshoe; it has three main parts - two lateral lobes and an isthmus. Every third person has another non-permanent lobule - pyramidal.
The size of the gland can vary significantly even in the same person, depending on the activity of its functioning. Gender, age, climate, medication use and, of course, diet largely influence the size and amount of gland hormones. Due to the tight connection with the larynx, its position can change, it rises and falls when swallowing, moves to the side when turning the head in different directions, which is visible to the naked eye
The structure of the thyroid gland is quite complex. Under a microscope, it is noticeable that it consists of many vesicles - follicles. Along the edges of the follicles there are cells - thyrocytes, and inside the follicle there is a thick watery liquid - colloid. Thyrocytes synthesize hormones, and they accumulate in a colloid for immediate release into the blood when needed.
In the walls of the follicles between the cells, as well as between the follicles themselves, there are larger, lighter parafollicular cells (C-cells), which produce the hormone calcitonin, which is involved in the regulation of calcium and phosphorus metabolism. It inhibits the removal of calcium from bones and reduces calcium levels in the blood.
Thyroliberin
Thyroliberin activates the production of thyroid-stimulating hormone by the pituitary gland. It stimulates the production of thyroid hormones by the thyroid gland. An increase in the concentration of thyroliberin most often indicates a lack of iodine in the body. This neurosecretion also affects the formation of growth hormone and prolactin.
Thyroliberin is synthesized not only in the hypothalamus, but also in the pineal gland, pancreas, and also in the gastrointestinal tract. This hormone affects human behavior. It increases performance and has a tonic effect on the central nervous system.
Currently, medications based on thyrotropin-releasing hormone have been created. They are used to diagnose thyroid dysfunction and acromegaly.