Detection of melatonin
In 1958, the team of Aaron Lerner, a professor of dermatology from Yale University in the USA, managed to isolate a new compound from the epiphyses of cows, which, when introduced into the skin of a tadpole, lightened it.
The substance blocked the production of melanocyte-stimulating hormone, which is why it was called “melatonin”. Later they discovered that the open compound is synthesized in the body mainly at night.
This was associated with daily periods of rest and wakefulness, and for two decades melatonin was considered only a sleep hormone that regulates human circadian rhythms.
Cellular Clock - Nobel Prize 2021
Chronobiology, the science that studies biological rhythms, distinguishes diurnal, tidal, weekly, seasonal and annual rhythms. In this article we will touch upon issues related to circadian (from Latin circa - “around, around” + dies - “day”) rhythms. Circadian rhythms arose as a result of daily changes in light caused by the Earth's rotation. Cyanobacteria, fungi, plants and animals have circadian rhythms. In humans, daily changes in physiological parameters can be observed: body temperature, synthesis of hormones (for example, cortisol) and enzymes, sleep-wake cycles [1], [2].
By the mid-twentieth century, much data had already been accumulated on circadian rhythms, and therefore the theme of the annual symposium on quantitative biology at Cold Spring Harbor in 1960 was “Biological Clocks.” The following decades saw major developments in the study of the molecular basis of circadian rhythms, for which Geoffrey Hall, Michael Rosbash and Michael Young were awarded the Nobel Prize in Physiology or Medicine in 2017 [3].
Using a fruit fly model, scientists have shown that there are genes, that is, physical carriers of information, that influence not just a trait (such as the color of human eyes or the color of bean flowers), but the behavior of the whole organism - when to go to bed; how many seconds to sing the marriage song. They isolated these genes (per, tim, dbt) and learned to make changes to them, thereby influencing behavior. They were able to unravel the full cycle of reactions that occur around the nucleus and allow the cell to maintain its own internal clock through the autoregulation of the protein machine.
Thus, it is now known that the body’s circadian rhythms are supported by the work of the internal cellular clock. What about environmental factors?
Melatonin production
80% of melatonin is produced by the pineal gland, a 100-125 mg pineal gland located in the brain. The remaining 20% of melatonin is produced by special cells:
- digestive tract;
- bronchi and lungs;
- kidney;
- pancreas;
- prostate and ovaries;
- retina, other organs and tissues.
Melatonin is produced even by blood cells: eosinophils and lymphocytes.
This discovery was made in 1974 by Soviet scientists Nathan Tanfelevich Raikhlin and Igor Moiseevich Kvetnoy. This “peripheral” melatonin does not affect circadian rhythms, working exclusively at the local level.
When should you contact Altimed MC?
You should seek help from the Altimed Medical Center if obvious signs of melatonin deficiency appear:
- Sleep problems - if you suffer from insomnia, wake up easily in the middle of the night or have trouble falling asleep, if you don't dream often during sleep, have shallow or restless sleep and anxious thinking at night - these are the main signs of low melatonin, although cortisol levels are also may be to blame. In fact, cortisol and melatonin levels have an inverse relationship with each other in the body.
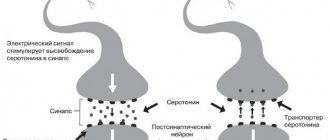
- Mood changes . If you lack inner peace, are always anxious, suffer from seasonal affective disorder or depression, or are always on edge and always irritable, you may have low melatonin levels. Melatonin is converted to serotonin, a neurotransmitter whose levels increase with some antidepressants.
- Menopause symptoms - hot flashes, increased heart rate, morning depression and irregular cycles - are believed to improve with melatonin supplements.
- Symptoms of Low Thyroid Hormone Levels . Melatonin helps convert thyroxine (T4) into active triiodothyronine (T3), which gives you energy and generates heat. In fact, melatonin and thyroid-stimulating hormone come from the pineal gland. Thus, symptoms of hypothyroidism may indicate low melatonin levels.
- Intestinal symptoms such as pain, hyperactivity and intestinal cramps may also indicate low melatonin levels.
Action of melatonin
The “sleep hormone”
begins to be produced between 20 and 22 hours (earlier for early risers, later for night owls). The concentration of melatonin peaks from midnight to two o'clock in the morning, and by six to seven o'clock in the morning it drops to its minimum level.
How does melatonin work?
- Absorbs free radicals - unstable molecules that damage organs and tissues, lead to decreased immunity, the development of tumors and cardiovascular diseases.
- It is the strongest natural immunomodulator, restores damaged cells, prevents diseases, including cancer.
- It has a pronounced chronobiotic effect: it regulates daily and seasonal biorhythms.
- Promotes sleep, is responsible for calm restorative sleep, bringing natural rest.
- Regulates the functioning of the endocrine system, normalizes body temperature.
- Acts as an antidepressant and prevents the occurrence of certain mental disorders.
- Slows down the rate of aging, increases life expectancy.
What lowers melatonin levels?
- Age. After 45-50 years, the production of natural melatonin decreases.
- Light. The pineal gland can only produce melatonin in the dark. If the lights are turned on at night, the production of the hormone slows down until it stops completely. The glow of the screens of a mobile phone, tablet, laptop, computer or TV reduces the synthesis of melatonin.
- Smoking.
- Drinking alcoholic or caffeinated drinks.
- Taking nonsteroidal anti-inflammatory drugs (NSAIDs), vitamin B12, and some other medications.
What increases melatonin production?
- Lack of light at bedtime
- Calcium
- Magnesium
- Vitamin B6
- A nicotinic acid.
Why is a lack of melatonin dangerous?
A lack of melatonin is dangerous for the body. The hormone performs a number of functions and also affects a person’s general well-being. Experts recommend carefully monitoring your health and melatonin levels. Its lack is:
- problems falling asleep;
- general hormonal imbalance;
- constant fatigue;
- tendency to depression;
- weak immunity;
- endocrine system disorder;
- disruption of brain function;
- weakening of bone tissue;
- blood pressure surges;
- the likelihood of developing mental illness.
Melatonin levels also affect overall body weight. Its deficiency is a direct path to excess weight gain.
The use of synthetic melatonin analogues in medicine
Most often, melatonin preparations are used to treat various sleep disorders.
Conducted studies prove the effectiveness of melatonin for acute insomnia: the time to fall asleep decreases, the quality of night sleep and its duration improve. Taking melatonin is justified in case of chronobiological disorders, when a person often changes time zones or works on a shift schedule alternating night and day shifts.
“Sleep hormone” drugs cannot be used as a usual sleeping pill. They help only with failures caused by a decrease in melatonin production. In other cases there will be no effect.
Melatonin is not prescribed for:
- chronic insomnia;
- maintaining the daily secretion of your own melatonin;
- normal biological rhythms.
Medications containing melatonin
Medications will help quickly restore hormone levels. Melatonin tablets are a common form of medication. But, the use of medications is carried out only according to indications, after determining the level of the hormone in the body. For this purpose, comprehensive diagnostics are carried out.
Sleep pills with melatonin are publicly available, but it is unacceptable to use them without consulting a specialist. There are a number of more natural processes that allow you to normalize the level of the hormone in the body. Including impulse impact on active points. Altimed Medical Center specializes in eliminating hormone deficiencies using modern equipment operating at various frequencies.
Dietary supplement or medicine?
There is still no consensus among doctors whether to consider melatonin a medicine or a biologically active supplement (dietary supplement).
IN THE USA
The Food and Drug Administration (FDA) has not approved it for medical use, so melatonin is sold over-the-counter as a dietary supplement.
In the European Union and Australia,
melatonin is considered a medicine, sold by prescription and used to treat insomnia in children, adolescents and people over 55 years of age.
In Russia
Dosage forms of the drug and dietary supplements have been registered and can be purchased in pharmacies and sports nutrition stores without a prescription.
Melatonin is used as an adjuvant therapy for:
- peptic ulcer of the stomach and duodenum;
- hypertension;
- Alzheimer's disease and other memory disorders;
- depression and other diseases.
Research into the pharmacological activity and effectiveness of melatonin is ongoing. To date, more than 26 thousand scientific papers have been published, each of which opens up new pages in the use of this amazing substance.
Risks of Taking Melatonin
Melatonin is considered safe for short-term use - for example, to restore sleep patterns. Even taking single extreme doses is unlikely to cause harm. There is not yet enough data on long-term use to consider it completely safe, but there are few risks. Here are the ones worth keeping in mind.
- Melatonin has side effects.
Headache, dizziness, daytime sleepiness and nausea are rare but do occur. They may be an individual reaction or a consequence of too high a dosage (above 3 mg). Melatonin also inevitably causes drowsiness immediately after taking it, so it is best to avoid driving or operating machinery for five hours after taking the supplement.
- Melatonin may interfere with the way medications work.
The list of drugs that are best not taken with the supplement is quite long. Anticoagulants, antiplatelet drugs, and any supplements that reduce blood clotting when combined with melatonin increase the risk of bleeding. Antidepressants and hormonal contraceptives - cause excessive drowsiness and may worsen side effects. Diabetes medications may not work as well because melatonin reduces insulin sensitivity and production. Anticonvulsants and immunosuppressants also work worse. So if you take medications, you should consult your doctor before purchasing melatonin.
- The composition of the supplement does not always correspond to the label.
The production of dietary supplements is not as strictly regulated as drugs. As a result, they may not contain melatonin at all or may not contain the amount indicated on the package. In 2017, researchers tested 31 melatonin supplements and found that melatonin content was within 10% of label claims in more than 71% of the supplements. 26% of the supplements also contained serotonin, which, if exceeded, can lead to serotonin syndrome, a rare but dangerous toxic reaction.
- It is not so easy to choose the dosage.
The brain produces less than 0.1 g of melatonin per night. Melatonin supplements usually contain much more: 2–12 mg. This number seems excessive. Especially in the context of studies in which melatonin reduced insulin sensitivity and production.
Melatonin and COVID-19
The COVID-19 pandemic, caused by the SARS-CoV-2 virus, has forced scientists to actively study the effect of melatonin on the course of this disease. As a result, the usual “sleep regulator” began to be used in a complex of means of auxiliary therapy for COVID-19. In the fall of 2020, it was even used to treat US President Donald Trump. US
Melatonin Reviews In October 2021, the electronic scientific library medRxiv published a report on a research work in which 800 cases of severe COVID-19 were studied. It turned out that patients who initially had high levels of their own melatonin, and those who received the hormone in the form of a drug, were significantly more likely to survive in intensive care. Melatonin increased the chances of recovery, both from coronavirus and any other infection that affects the lungs.
Canada and Argentina.
The work was published in the journal Diseases in November 2021. A joint study from the University of Toronto and the Pontifical Catholic University found that the disease may be more severe in older people due to decreased levels of melatonin. Melatonin in adequate doses prevents the development of an aggressive form of COVID-19, and also supports the effect of the anti-coronavirus vaccine.
Brazil.
Data published by Melatonin Research in early 2021. Scientists from the University of Sao Paulo have proven that melatonin, which is produced by the cells of the alveoli of the lungs, becomes a barrier to coronavirus. This may be why people with high levels of melatonin do not become infected with Covid or experience the disease easily. Regina Pekelman, the author of the study, is confident that using nasal drops or a spray with melatonin is an effective means of combating COVID-19.
To enter the human body, SARS-CoV-2 viruses must bind to angiotensin-converting enzyme 2 (ACE2) receptors located on the surface of lung cells. Only by combining with ACE2 do coronaviruses enter the cell and begin to multiply, leading to disease.
Melatonin reduces the number of free ACE2 receptors, as a result, the number of connections between the virus and the enzyme is reduced, which leads to damage to a minimum number of cells, which means the coronavirus infection will occur in a mild form.
Additionally, melatonin reduces the inflammatory response at the site of virus entry and controls the immune response, preventing the development of a “cytokine storm.” And since it is the violent cytokine reaction that leads to a fatal result, its suppression increases the patient’s chances of surviving and avoiding serious complications.
In our country
sufficient scientific experience has not yet been accumulated to confirm the fact that melatonin prevents severe COVID-19, and the mechanism of action of melatonin on the human body has not yet been sufficiently studied. However, empirical evidence provides encouraging results and supports the positive effect of melatonin on the outcome of COVID-19.
Melatonin preparations are available in Russia without a prescription, but you should not take them without an in-person consultation with a doctor, either to correct sleep disorders or to prevent or treat COVID-19.
Melatonin secretion
Melatonin (N-acetyl-5-methoxytryptamine) is a substance discovered by the American dermatologist A. Lerner. In the body of vertebrates, small amounts of melatonin are secreted by the retina of the eyes and significant amounts by some cells of the intestinal mucosa, but the main source of systemic melatonin is the pineal gland. Melatonin is synthesized from the essential amino acid tryptophan. The rhythm of its secretion by the pineal gland has a clearly defined circadian character. The level of this hormone in the blood begins to increase in the evening, coinciding with a decrease in light levels, reaches a maximum in the middle of the night (at 2:00-3:00), then progressively decreases towards the morning. During the daytime, melatonin secretion remains at a very low level. The circadian rhythm of melatonin production by the pineal gland is set by the suprachiasmatic nucleus of the thalamus (SCN) depending on the level of illumination [1-2].
Melatonin functions as a chemical carrier of information from the circadian pacemaker. The central melatonin receptors MT1 and MT2 are concentrated mainly in the SCN, in which melatonin acts according to the principle of negative feedback. In addition, the presence of MT1 and MT2 receptors in blood vessels, adipocytes, liver, and pancreas determines the functions of melatonin in regulating the sleep-wake cycle and synchronizing the onset of sleep with changes in metabolic processes and the functioning of internal organs. Disruption of the circadian rhythm of melatonin synthesis leads to the development of desynchronosis, which manifests itself in a mismatch of circadian rhythms in the work of different functional systems and the development of a number of diseases.
Laboratory diagnostics
On average, the adult body synthesizes about 30 mg of melatonin per day. In human blood, more than 80% of circulating melatonin is of epiphyseal origin. The half-life of melatonin in the human body is, according to various sources, from 30 to 50 minutes. Inactivation of melatonin occurs mainly in the liver, where, under the influence of a system of microsomal oxidative enzymes, it is converted into 6-hydroxymelatonin (6-hydroxyMT). Most 6-hydroxyMT is excreted in urine and feces as the sulfate conjugate of 6-sulfatoxymelatonin (6-SOMT).
Currently, in clinical laboratory diagnostics, there are methods with analytical characteristics that make it possible to determine both the content of melatonin in plasma and saliva and its derivative 6-COMT in urine. Due to pronounced hourly fluctuations in the level of melatonin in the blood and the rapid breakdown of melatonin (half-life of no more than 50 minutes), an objective assessment of its content is possible only by placing a catheter and repeated blood sampling during the day, which cannot be recommended for widespread use in clinical practice. In this regard, the assessment of the content of the main melatonin metabolite 6-COMT in urine is currently most widely used. Given the pronounced dependence of melatonin synthesis on the time of day, it is customary to evaluate the concentration or excretion of 6-COMT separately in night and daytime urine.
Standardization of the preanalytical stage for determining melatonin metabolites in urine should become a mandatory procedure when using this test for diagnostic purposes. Data on the excretion of 6-COMT may become the basis for determining additional indications for the use of melatonin in the treatment of insomnia and other diseases. In assessing the metabolism of melatonin in clinical practice, in addition to the level of nocturnal excretion of its metabolites, the level of daytime, nighttime and evening excretion and the ratio of these parameters may be important.
Individual fluctuations
The difficulty in interpreting the data obtained on melatonin excretion in patients is associated with the large scatter of individual values. Pronounced individual fluctuations in melatonin levels among healthy subjects are associated with variability in the size of the pineal gland. Autopsy data revealed significant variability in the size of the pineal gland, reaching 20-fold differences between patients [3]. The same significant fluctuations in the level of melatonin secretion were noted by many researchers [4-5] in healthy subjects. A study [6] of the relationship between the size of the pineal gland and the amount of 6-OHMT in the morning urine in 122 men aged 75±2.2 years using magnetic resonance imaging (MRI) revealed a strong correlation between the volume of the parenchyma and the level of 6-OHMT, with a significant variability of both parenchyma volume (from 65 to 503 mm3) and melatonin concentration in the morning urine (21±16 ng/ml). There was no relationship between melatonin secretion and the presence of cysts or calcifications in the pineal gland. The only significant factor for melatonin synthesis was the volume of parenchyma consisting of active pinealocytes. Another study showed [7] a significant relationship between parenchymal volume and the amount of 6-COMT in daily urine. An important finding of these studies was evidence that the level of melatonin secretion is related to the volume of the parenchyma, and not the volume of the entire pineal gland, which may include both cysts and calcifications. This relationship remained significant after excluding the influence of age, insomnia, and body mass index.
Factors determining the decrease in melatonin synthesis by the pineal gland
Age.
Melatonin synthesis by the pineal gland rapidly increases in the newborn, reaching a maximum by 2-4 years. A sharp decrease in melatonin synthesis occurs during puberty and then there is a slow progressive decrease throughout life (see figure).
Decrease in melatonin synthesis with age (according to [43]).
The x-axis is the age of the patients (years); the y-axis is the melatonin level (ng/ml). A progressive decrease in melatonin synthesis during normal aging is associated with a decrease in the volume of the functionally active pineal gland due to its calcification, degeneration of the SCN, and hormonal changes in the body. There is a predominant decrease in the synthesis of nighttime melatonin with fairly large individual fluctuations. Bad habits.
A decrease in melatonin levels was found in active smokers [8]. Alcohol consumption also reduces melatonin synthesis and causes sleep disturbances [9].
Medicines.
Many drugs widely used in modern medicine significantly reduce the synthesis of endogenous melatonin. This list includes beta blockers [10, 11], benzodiazepines [12], and nonsteroidal anti-inflammatory drugs [13, 14]. The most significant for melatonin secretion is the use of beta blockers, which cause a decrease in melatonin secretion by up to 50%. It is the decrease in melatonin synthesis that is one of the most important reasons for the development of insomnia when taking these medications.
Illumination.
Another important factor determining the decrease in melatonin synthesis by the pineal gland is light exposure. If even slight external lighting is maintained in the evening and at night (computer on, outdoor advertising lights, night light), melatonin secretion will be disrupted. Evaluation of melatonin concentration in the blood during sleep in healthy people showed a decrease in melatonin synthesis by more than 50% during sleep with preserved light compared to sleep in darkness. A significant difference in melatonin synthesis was also revealed depending on the intensity of room illumination before bedtime [15].
Artificial illumination at night, characteristic of modern life, inhibits the synthesis of endogenous melatonin. According to numerous studies, the progressive increase in illumination at night poses a serious threat to the health of the inhabitants of the Earth. Disruption of the circadian dynamics of melatonin synthesis associated with illumination and work at night is manifested by desynchronoses, which increase the risk of developing various somatic, neurodegenerative and oncological diseases [1, 16].
Sleep-wake cycle disorders.
Sleep-wake cycle disorders include: delayed sleep phase syndrome, advanced sleep phase syndrome, shift work disorder and jet lag. Melatonin plays a leading role in the treatment of these sleep disorders.
Delayed sleep phase syndrome is a disorder in which the usual sleep time is delayed in relation to the desired and accepted in the social environment by at least 2 hours, which is determined by the patient’s complaints of the inability to fall asleep and difficulties in waking up at the desired or appointed time of day. Late falling asleep is accompanied by painful morning awakening and drowsiness in the first half of the day. The prevalence of the syndrome is highest among adolescents and ranges from 7 to 16%. The role of genetic factors in the development of this syndrome is shown. A characteristic shift in the synthesis of endogenous melatonin is later than normal. Treatment includes taking melatonin 1 hour before desired sleep and using phototherapy upon awakening.
Advanced sleep phase syndrome is a disorder in which the usual sleep time occurs earlier than desired or accepted in the social environment by at least 2 hours, which is determined by the patient’s complaints of a strong craving for sleep in the evening and early final awakening. The prevalence of this syndrome does not exceed 1% among middle-aged people. The treatment uses a chronotherapeutic approach.
Shift work sleep-wake cycle disorder is a condition characterized by symptoms of insomnia and daytime sleepiness that occurs in connection with a shift work schedule. The manifestation of the disorder depends on the work schedule. It is necessary to follow recommendations for sleep hygiene and organize the maximum possible duration of sleep in shift work conditions. Drug therapy includes the use of melatonin when it is necessary to sleep during the day, phototherapy and psychostimulants to reduce drowsiness when it is necessary to work at night.
Jet lag is a condition characterized by symptoms of insomnia, excessive daytime sleepiness, and impaired daytime functioning that occur when rapidly traveling across 2 or more time zones. The reason for the development of the disorder is the discrepancy between the activity of the internal pacemaker and local time. The severity of discomfort that a person feels after a flight depends on the direction of travel, age, and chronotype. When flying in an eastern direction, you experience difficulty falling asleep; when flying in a western direction, you have to go to bed later, which is easier to bear. Typically, symptoms last no more than 2-3 days while adaptation to the new time zone occurs. If adaptation to new conditions is insufficient, the use of Z-hypnotics is recommended. Another drug that facilitates phase shift is melatonin.
Diseases for which melatonin treatment has been proven effective
Diabetes mellitus and metabolic syndrome.
The progressive increase in the prevalence of obesity, metabolic syndrome and type 2 diabetes mellitus over the past 50 years is often associated with a decrease in physical activity and unhealthy, excess nutrition.
However, increasing evidence suggests a critical role for sleep deficiency and desynchronosis in the development of these conditions. It has been shown [17] that metabolic syndrome and diabetes mellitus are associated with oxidative stress, activation of proinflammatory cytokines, prothrombotic mediators and a decrease in nocturnal melatonin secretion. Evaluation of the concentration of 6-OHMT in the first morning urine in patients without diabetes and further 12-year follow-up showed a significantly lower initial level of 6-OHMT in patients with subsequent development of type 2 diabetes mellitus (1910 [340; 7980]) mg/dL compared with the group without developing diabetes (2410 [430; 9922] mg/dL, p
= 0.02). Exclusion of the influence of other factors made it possible to prove the existence of an independent association between reduced melatonin secretion and the development of type 2 diabetes mellitus.
The addition of melatonin to standard therapy for metabolic syndrome and diabetes mellitus has shown its effectiveness in lowering blood pressure, normalizing lipid metabolism, and carbohydrate metabolism [18, 19].
Oncological diseases
. Epidemiological studies have shown that desynchronosis caused by night work increases the risk of developing breast and prostate, rectal, and lung cancer. Non-small cell lung cancer is the leading cause of cancer death worldwide. Lung cancer accounts for about 13% of all diagnosed malignancies. More than 85% of lung cancers are classified as non-small cell, with a 5-year survival rate of only 15.9%. Surgical treatment and chemotherapy show low effectiveness. Data on the anticarcinogenic properties of melatonin [20] and a decrease in its level in patients with lung cancer [21] served as a rationale for the prescription of melatonin. A number of clinical studies [22, 23] provide convincing evidence that the addition of melatonin to standard chemotherapy significantly increases the effectiveness of treatment, reduces the side effects of chemotherapy, improves quality of life and increases 5-year survival. All studies used high doses of melatonin—20 mg/day.
Neurodegeneration and melatonin
. Numerous neurodegenerative diseases, among which Parkinson's disease and Alzheimer's disease have received the most attention, are accompanied by various sleep disorders. Moreover, sleep deficiency is essential for the progression of dementia, since drainage function and removal of waste products from the brain, including amyloid, occur predominantly during sleep [24]. The progression of neurodegenerative diseases is also associated with oxidative stress and mitochondrial dysfunction. The presence of melatonin with pronounced antioxidant properties, as well as the ability to selectively accumulate in mitochondrial membranes, normalizing their work, is considered as the leading mechanism of the neuroprotective effect of melatonin in Alzheimer's disease [25]. Studies examining melatonin secretion in Alzheimer's disease are scarce and indicate that there is no correlation between Alzheimer's disease, sleep disturbance and the level of 6-hydroxyMT secretion [26]. At the same time, it has been shown that long-term (1–4 months) administration of melatonin in doses of 3 to 9 mg helps normalize sleep and has a potential positive effect on cognitive function in Alzheimer’s disease [27, 28].
A sleep disorder in the form of REM sleep behavior disorder (RBD) deserves special mention. RPPS is manifested by various motor and speech activity. Motor activity varies from isolated shudders to complex aggressive forms with pushing and grabbing objects, which can lead to injury to both the patient and the bed partner. Motor activity is often accompanied by speech production. Unlike sleepwalking, patients do not leave the bed, their eyes are closed. Episodes occur predominantly in the second half of the night, during REM sleep, and the nature of motor and speech production reflects the nature of dreams.
The prevalence of RPHD in the population is 1-2% and occurs mainly over the age of 50 years. There are idiopathic and secondary RPPS, which develop in patients with synucleinopathies (Parkinson's disease, dementia with Lewy bodies, multiple system atrophy), autoimmune diseases (narcolepsy, limbic encephalitis), with focal lesions of the brain stem (stroke, multiple sclerosis), during abstinence and withdrawal of a series of psychotropic drugs (anticholinergic and serotonergic). Since almost all patients with idiopathic RPPS subsequently develop a neurodegenerative disease, this category of disease can also be classified as secondary.
The drug of choice for the treatment of RPPS is clonazepam at a dose of 0.5-2.0 mg, taken 30 minutes before bedtime (level A). Clonazepam significantly reduces motor activity and injuries associated with RPPS. Limitations for use include the presence of dementia, gait disturbances and obstructive sleep apnea, as clonazepam may exacerbate these manifestations.
Melatonin in a dose of 3-12 mg is used to treat RPPS (level B). Its effectiveness in controlling both primary and synucleinopathies-associated RPPS is less than that of clonazepam, but greater than that of other drugs used. Melatonin may be the drug of choice for the treatment of RP in patients with cognitive impairment, gait disturbances, and obstructive sleep apnea [29]. It can be prescribed either alone or in combination with clonazepam.
Insomnia and melatonin.
Insomnias are repeated disturbances in the initiation, duration, consolidation or quality of sleep that occur despite the availability of sufficient time and conditions for sleep and are manifested by disruption of various types of daytime activities. Sleep disturbances, along with headaches and dorsalgia, are the most common complaints when visiting a neurologist. According to epidemiological data, insomnia occurs in 28-45% of the world's population and in 50% of cases it is an important problem requiring treatment. At the same time, 1.5-3% of the population constantly and 25-29% occasionally take sleeping pills.
The onset of sleep and its individual stages is associated with the activity of a complex network of nervous structures, functioning with the help of various neurotransmitter systems, among which melatonin plays an important role. These ideas suggest a possible deficiency of endogenous melatonin in patients with insomnia and justify the administration of exogenous melatonin.
There is now a large body of research demonstrating the effectiveness of using melatonin to improve sleep quality and efficiency. The effectiveness of melatonin preparations for insomnia has been confirmed in both foreign [30-32] and domestic [33] studies. It has been shown [34] that long-term use is not accompanied by a decrease in effectiveness or the development of serious adverse events. A meta-analysis of clinical trials of the use of exogenous melatonin [35] proved its effectiveness in the treatment of insomnia. Data were obtained on a significant reduction in sleep onset time in patients with primary sleep disorders who received exogenous melatonin compared with the placebo group.
It should be noted that in the vast majority of studies, the inclusion criterion was the presence of insomnia, regardless of the level of endogenous melatonin. Studies of 6-COMT excretion in patients with insomnia are few and the results are contradictory. A number of studies have shown a decrease in 6-COMT excretion in nighttime urine in patients with insomnia compared to controls [36–38], but other studies have not found such a relationship [39–40]. The most significant decrease in 6-COMT excretion in the night portion was found in patients with insomnia over the age of 55 years. G. Hajak et al. [41, 42] in their studies found low melatonin levels in patients with long-term insomnia (more than 5 years) compared to patients with short-term insomnia (less than 5 years). It was concluded that melatonin levels may be associated with the duration of sleep disturbances. It was shown [31] that there was a more significant decrease in 6-COMT excretion in patients with insomnia and cardiovascular diseases.
In patients with a combination of cardiovascular pathology and insomnia, the diagnosis of 6-COMT excretion takes on additional importance, since it is known that a decrease in melatonin synthesis is associated not only with the development of insomnia, but is also associated with the risk of developing diabetes mellitus and arterial hypertension. Detecting a decrease in 6-hydroxyMT in these patients and prescribing melatonin in this case will have implications for both the treatment of insomnia and cardiovascular disease.
Conclusion
Melatonin has broad therapeutic potential, normalizing circadian rhythms and exhibiting its antioxidant, anti-inflammatory, analgesic and anticarcinogenic properties. The absence of significant side effects of melatonin, in contrast to sleeping pills, determines the wide possibilities of its use.
Until recently, there were only two melatonin preparations from foreign manufacturers on the Russian pharmaceutical market (melaxen and circadin). In 2021, the Russian drug Sonnovan, containing 3 mg of melatonin, was introduced to the market. Sonnovan is recommended to be taken as a sleeping pill 3 mg 30-40 minutes before bedtime, as an adaptogen when changing time zones 1 day before a flight and in the next 2-5 days 3 mg 30-40 minutes before bedtime. It is important to emphasize that melatonin is a regulator of circadian rhythms and therefore the recommendation of taking it 30 minutes before bedtime should be supplemented by the recommendation of taking it at the same time.
The greatest effectiveness of melatonin in the treatment of chronic insomnia was observed in patients over 55 years of age, individuals taking beta blockers, in patients with insomnia duration of more than 5 years and in patients with decreased nocturnal melatonin synthesis.
Insomnia is often observed in patients with cardiovascular diseases, metabolic syndrome, neurodegenerative diseases and cancer. Melatonin should be the drug of choice in these cases, as it has a normalizing effect not only on sleep, but also on the underlying disease.
The publication was supported by Canonpharma Production CJSC (Russia).
*e-mail Zybina N.N. https://orcid.org/0000-0002-5422-2878br />Tikhomirova O.V. https://orcid.org/0000-0003-4722-0900
Publications on the topic of the month “How to overcome post-Covid syndrome”
- Lung recovery after coronavirus
- Restoring the sense of smell after coronavirus
- Restoring memory after suffering from coronavirus
- Overcoming mental disorders during post-Covid syndrome
- We are experiencing COVID. How the coronavirus pandemic affects mental functioning
- Post-Covid screening - examination after a new coronavirus infection
- How to return digestion to normal after coronavirus?
- Loss of smell due to COVID-19 - advice from an otolaryngologist
- Recommendations from a cardiologist after suffering from COVID-19
- Coronavirus turned out to be “vindictive” - what is important to know
- Post-Covid syndrome: program for diagnosis and regression of post-Covid symptoms. How to Manage Long-Term Long COVID Symptoms
How to check if melatonin tablets are right for you?
The medicine chosen by your doctor helps you if you:
- fall asleep quickly and sleep soundly;
- became calmer, stopped getting irritated over trifles;
- feel active and cheerful;
- We learned that the tumors had stopped actively growing.
To get visual evidence, take a photo before you start taking melatonin and after you stop taking it. If in the second photo you look fresher and even younger, the course has clearly benefited you. Get enough sleep and be healthy!