- Diagnosis of cervicitis
- Treatment of cervicitis
- Cervicitis and infertility
- Cervicitis and pregnancy
Cervicitis is an inflammatory process that occurs in the cervix. Both the vaginal part of the cervix (exocervix) and the mucous membrane of the cervical canal (endocervix) may be affected. Depending on this, exocervicitis or endocervicitis is diagnosed.
Causes of cervicitis
Cervicitis is a common disease that affects approximately every third woman. This pathology can cause infertility and the development of a number of serious complications during pregnancy.
- Sexually transmitted infectious diseases (chlamydia, gonorrhea, trichomoniasis, mycoplasmosis). Pathogenic microorganisms, penetrating the genital tract, rise up through the vagina and, in the absence of timely treatment, affect the cervix. Further infection of the fallopian tubes (salpingitis) and ovaries (oophoritis) is also possible;
- Infectious diseases caused by opportunistic microorganisms (staphylococcus, streptococcus, E. coli);
- Fungal diseases (candidiasis). Active reproduction of fungi of the genus Candida causes an alkaline environment, which provokes a decrease in local immunity. Damage to the mucous membranes is the cause of the development of vaginitis and cervicitis;
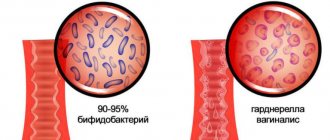
- Bacterial vaginosis (dysbacteriosis) is an inflammatory process of the vaginal mucosa caused by changes in microflora. There is a sharp decrease in the number of lactobacilli and the identification of a large number of polymicrobial anaerobic flora (Klebsiella, Gardnerella, Bacteroides, etc.);
- Damage and trauma to the cervix (surgery, childbirth, artificial termination of pregnancy);
- Diseases of the genitourinary system (pyelonephritis, cystitis);
- Decreased immunity.
Types of disease
What is chronic cervicitis, and what other forms of this disease exist, interests many women. The disease has a rather complex classification, but the main subtypes can be distinguished:
- Papillary - this form of chronic cervicitis manifests itself in that a huge number of papillomas appear. They have a benign form.
- Cervical ectopia is a form of cervicitis in which epithelial cells of the cervical canal grow and spread to the cervix. This type of disease can even lead to infertility.
- Inactive cervicitis is a form in which the cervix thickens, pseudo-erosions and cysts appear inside the cervix. It also has scarring changes.
- Chronic active cervicitis is a form in which there is redness of the cervical mucosa, swelling, as well as discharge and erosion.
Cervicitis is also divided into other types:
- Exocervicitis - when the vaginal segment of the cervix becomes inflamed.
- Endocervicitis is an inflammatory process that affects the inner lining of the cervical canal.
Symptoms of cervicitis
There are a number of signs to suspect cervicitis. These include:
- Discharge from the genital tract that is mucous or purulent in nature. The characteristics of the discharge are determined by the cause of cervicitis. So, if the disease is caused by gonococci, the discharge becomes yellowish, if trichomonas, it becomes foamy.
- Periodic pain in the lower abdomen, which can be either dull, pulling or sharp, cutting in nature
- Painful sensations and bloody discharge after sexual intercourse
- Pain when urinating
- Burning and cutting in the external genital area
However, in some cases the clinical picture is blurred, and the woman, as a rule, does not see a doctor. This is very dangerous, because... if left untreated, the inflammatory process begins to spread to surrounding tissues.
During the examination, pathological changes in the cervix are revealed, which also vary depending on the causative agent of the infection. Thus, trichomonas cervicitis is characterized by the presence of small hemorrhages, gonorrheal cervicitis is characterized by looseness and hyperemia of the cervix with areas of ulceration, candidal cervicitis is characterized by alternating areas with a rough and very smooth (varnished) surface.
Why is cervical inflammation dangerous?
Self-medication risks complications, so only a doctor should decide how to treat a woman. If the patient does not seek help in a timely manner, acute cervicitis becomes chronic. A woman faces consequences such as erosion, miscarriage, and spread of the inflammatory process to the appendages. The risk of developing cancer increases. Chronic cervicitis leads to the formation of adhesions and infertility. Patients often experience chronic pelvic pain, menstrual irregularities and other manifestations that reduce quality of life.
Atrophic cervicitis
In addition to infection by various types of microorganisms and injury to the cervix, atrophic cervicitis can be caused by prolapse of the vagina and cervix, a decrease in estrogen levels during menopause, and the use of certain contraceptives, which, for example, include chemical spermicides. As a rule, atrophic cervicitis develops as a result of a long (chronic) course of the pathological process. The mucous membrane of the cervix becomes thinner and ulcers form on it.
Characteristics of chronic exocervicitis
To identify this form of inflammation, it is enough to undergo a routine gynecological examination; to confirm the diagnosis, the doctor may prescribe additional tests.
In chronic exocervicitis, the vaginal part of the cervix is affected by staphylococci, streptococci or Candida fungi - nonspecific inflammation, and in case of specific inflammation, the causative agents are ureaplasma, herpes and chlamydia.
This form of the disease lasts for at least two months, with periodic exacerbations and remissions.
Diagnosis of cervicitis
Diagnosis of cervicitis involves:
- examination of the patient by an obstetrician-gynecologist in the speculum, which allows identifying pathological changes in the visible part of the cervix
- conducting an extended colposcopy - examination of the cervix under significant magnification, allowing a detailed examination of the affected areas, determining the nature of the changes, including through special tests
- Ultrasound of the pelvic organs
- obtaining laboratory test results that allow identifying the type of pathogen, selecting the most effective drug for treatment, and identifying changes at the cellular level.
Description of moderate exocervicitis
In gynecology there is such a concept as “moderate exocervicitis”. What is it really? This is a mild inflammatory process of the surface or intermediate layer of the cervical epithelium. The symptoms are the same as for an acute illness, but less pronounced. The general manifestations include imbalance in behavior, constant anxiety, and excessive psychosis.
To identify a moderate form of the disease, a special analysis is performed - a cytogram. With the help of such a study, the disease can be recognized at an early stage.
A cytogram is a reliable way to identify and monitor a number of abnormalities in the body
This analysis allows:
- determine the presence of oncological tumors;
- detect leukoplakia;
- see changes in tissues;
- consider polyp enlargement;
- determine the number of eosinophils, leukocytes and other blood cells.
Treatment of cervicitis
Treatment of cervicitis depends on the reasons that caused it and on the duration of the inflammatory process. Taking antibacterial, antiviral, and antifungal drugs may be indicated. In addition, immunostimulants and vitamin complexes can be prescribed. Vaginal dysbiosis requires restoration of normal microflora. If the basis of cervicitis is a hormonal imbalance, the doctor may recommend replacement therapy. Chronic cervicitis is much less treatable. In some cases, surgical treatment (laser therapy, diathermocoagulation, etc.) may be used.
Conservative therapy
The basis is anti-inflammatory oral and local agents. These are vaginal suppositories, tablets, ointments. When bacteria are detected, antibiotics are required. If tests detect HPV or herpes virus, then therapy includes antiviral agents.
The following may also be prescribed:
- Antiseptics.
- Immunomodulators.
- Vitamin and mineral complexes.
- Physiotherapy.
- Hormonal agents for the atrophic form of the disease.
When an STI is detected, it is advisable to consult a doctor not only for the woman, but also for the sexual partner. During treatment, sexual rest is recommended.
The first stage is always aimed at combating the underlying cause of cervicitis. Only then is the consequences eliminated. The chronic form requires long-term medication and an integrated approach. Subsequent tests are required to assess the effectiveness of therapy and a repeat colposcopy is required.
A course of drug therapy can only cope with the initial form of the disease. When there is no positive dynamics, the doctor recommends surgical methods.
Surgery
Modern medicine offers gentle and low-traumatic ways to get rid of the consequences of cervicitis - ectopia, condylomas, adhesions. These methods do not require long recovery or preliminary preparation.
- Cryodestruction
Involves exposure to low temperatures (liquid nitrogen) on the pathological focus.
- Diathermocoagulation.
Prescribed only to women who have given birth. Cauterization occurs using an electric current of the required strength. At the moment, the method is considered obsolete.
- Using laser or radio waves
Advanced painless methods. Can be used by young girls planning pregnancy.
Sometimes chemical cauterization using special solutions is prescribed for young girls.
During the rehabilitation period, it is recommended to refrain from sexual contact and maintain careful intimate hygiene. It is safer to take a shower rather than a bath. It is not recommended to lift weights or perform active physical exercises. If there is discharge, use pads without fragrances or fragrances.
The optimal result when using surgical treatment methods can be obtained if antiviral and antibacterial therapy has been previously carried out. If a pathogenic pathogen remains in the body, then a relapse will not be long in coming.
Cervicitis and pregnancy
Of course, it is best to undergo a course of treatment for cervicitis at the stage of preparation for pregnancy. The fact is that cervicitis, diagnosed already in the gestational period, poses a danger to the health and life of the unborn child. The pathogen can ascend into the amniotic fluid and cause infection of the fetus. In the early stages, when the formation of organs and body systems occurs, infection can cause developmental defects. If the fetus is infected at a later stage, developmental delays may occur.
Cervicitis can cause isthmic-cervical insufficiency (ICI), which threatens termination of pregnancy in the 2nd and 3rd trimester. Also, with cervicitis, the risk of premature birth and the birth of a child with low body weight is increased.
Women diagnosed with cervicitis are more likely to develop complications in the postpartum period. Treatment of cervicitis during pregnancy is prescribed by an obstetrician-gynecologist based on the results of the examination, taking into account concomitant pathologies. Monitoring the condition of the expectant mother and baby should be carried out by a qualified obstetrician-gynecologist with extensive experience in managing complicated pregnancies.
If you have any questions related to cervicitis, you can ask them to the doctors at Nova Clinic. You can make an appointment with a gynecologist-reproductologist or obstetrician-gynecologist by calling the phone number listed on the website or using the booking button.
Disease prevention
Cervicitis is treatable. You can completely get rid of it if you use the right tactics and follow your doctor’s advice. If you do not start the disease in an acute form, but immediately take specific therapeutic measures, the disease can be defeated at the initial stage.
Prevention of the disease involves following the rules of personal hygiene, having one partner who is healthy and regularly undergoes examination. It is also important to remember to use a condom in case of casual sex, eat right, have a healthy lifestyle and regularly see a doctor. It is also important to remember that a woman must have healthy intestinal microflora and good immunity, which must be strengthened. It’s also a good idea to get tested for serious diseases (syphilis, hepatitis) at least once a year. All these measures will help avoid this unpleasant disease.
Why do they trust us?
For patients who choose the Private Practice clinic, we guarantee:
- high professional qualifications, attention, friendliness of the staff;
- sterility, comfortable conditions;
- effective result of therapy;
- anonymity;
- relevance of licenses and certificates;
- compliance with the standards of the Ministry of Health and the norms of medical legislation of the Russian Federation.
We have a flexible system of discounts and promotional offers. The clinic is conveniently located a 5-minute walk from the Varshavskaya metro station. Leading Moscow doctors with 10 years of successful experience are waiting for you at Private Practice every day, seven days a week.
Regina Rubenovna Petrosyan, a gynecologist and mammologist at the Private Practice clinic, talks about ureaplasmosis in women.
Doctor of the Private Practice clinic, gynecologist, mammologist Svetlana Vitalievna Nagovitsina talks about cervicitis.