Before talking about the treatment of mastitis in women, it is necessary to understand what it is. Mastitis occurs both during and without lactation. We will only talk about lactation mastitis and the treatment of mastitis in nursing mothers.
Lactation mastitis is an inflammatory disease of the mammary gland associated with breastfeeding. Postpartum mastitis is distinguished separately, since it occurs most often and develops within 30 days after birth. The cause of its occurrence is clearly a nosocomial infection.
But not all women suffer from this disease after childbirth. It develops against the background of a significant weakening of the immune system due to:
- difficult pregnancy, especially in the last trimester;
- purulent-inflammatory diseases during pregnancy;
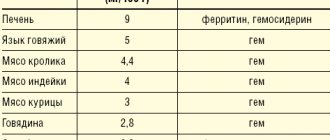
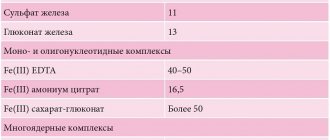
- decrease in hemoglobin level, both before and after childbirth;
- difficult childbirth;
- large blood loss;
- chronic diseases (pyelonephritis, diabetes mellitus);
- taking certain hormonal medications.
Lactation mastitis in the subsequent feeding period occurs due to foci of chronic infection (tonsillitis, frontal sinusitis, caries, etc.), during acute respiratory infections, due to untreated lactostasis. There is an opinion that mastitis is always preceded by lactostasis. This is wrong. Stagnation of milk can become a background for the development of mastitis. But more often the opposite happens: the resulting inflammation leads to swelling of the mammary gland, which compresses the ductal system and forms lactostasis.
Acute and chronic mastitis: causes of pathology
The main cause of the disease is an infectious process. The main culprit is Staphylococcus aureus, less often other types of bacteria (Staphylococcus epidermidis, streptococci, enterococci, E. coli). The infection is activated under the influence of unfavorable factors - both external and internal. Among them:
- Hormonal imbalance in the reproductive system weakens the body's defenses. Reason: prolonged mental and physical stress, treatment with hormonal drugs, steroid use (in particular among athletes), chronic endocrine diseases.
- Decreased immunity - gives the green light to various infections, including opportunistic microorganisms. Reason: hypothermia, poor diet, stress, lack of vitamins, microelements, fresh air.
- Stagnation (lactostasis in lactating women) - a violation of the outflow of milk creates a favorable environment for the development of bacteria. Reason: inept pumping of milk, improper attachment of the baby to the breast, tight bra, tight clothing, severe lack of physical activity.
- Various pathologies of the mammary glands (fibrocystic mastopathy, complications after plastic surgery, etc.).
Common provoking factors include poor ecology, stress, sudden climate change, and failure to comply with hygiene rules. In nulliparous women, the cause of the pathology can be unsuccessful piercing and too active sexual games with injury to the nipples.
What causes it?
According to foreign clinicians, until the 1980s it was generally accepted that mastitis in a nursing mother occurs only due to infection. But further observations showed that even after a course of antibacterial therapy, recurrent incidence was often observed. Scientists believe that pathology is caused by several factors that affect the body simultaneously:
- Reduced body resistance - with weak immunity, the risk of infection increases several times. This condition can be provoked by toxicosis of pregnancy, frequent morbidity during pregnancy, or bleeding during childbirth. A separate group includes patients with chronic autoimmune diseases (rheumatism, lupus erythematosus, etc.) or congenital defects.
- Stagnation occurs due to incomplete feeding with increased milk production, narrow ducts in the gland, when transferring the child to artificial nutrition. Often the feeding process is disrupted if a woman has a flat nipple or external damage to the areola.
- Infection – for the development of mastitis, there must be an entry gate for microbes. The most common route of penetration is through wounds on the nipple; almost half of the cases are associated with cracks or abrasions in this area.
Until recently, it was believed that smoking provokes mastitis, but now this statement is disputed - Western clinicians claim that women with a bad habit simply lose their appetite and eat worse. This leads to a decrease in immunity, which can subsequently lead to the development of mastitis.
Types and forms of mastitis
There are acute and chronic forms of the disease. The first includes lactation or postpartum mastitis with pronounced symptoms. An example of the second is a non-lactation type of pathology, which is not associated with the period of breastfeeding and is not clearly linked to gender and age.
On a note! According to statistics, lactation mastitis occurs on average in 5% of lactating women. In unfavorable regions, this figure can rise to 15%. Moreover, 85% of all cases of the disease occur in first-time mothers. Non-lactation mastitis is less common (no more than 10% of the total number of all manifestations of mastitis) and can affect women of different ages, men, and children.
There are 3 clinical forms of the disease:
- Acute postpartum – develops against the background of congestion in nursing women.
- Plasma cell - more typical for multiparous women in the period after the end of lactation, as well as during hormonal changes during menopause. The disease occurs in a moderately acute form, with mild symptoms, which makes it similar to tumor pathologies of the mammary gland
- Neonatal mastitis – observed in infants of both sexes as a result of residual effects of maternal hormones (is a complication of physiological mastopathy in newborns).
On a note! Separately, it is worth mentioning cases of mastitis in men, which are considered a direct consequence of chronic endocrine diseases and hormone imbalance. The pathology manifests itself in the presence of diabetes mellitus, gynecomastia, tumors of the genital organs, as well as with long-term use of steroids in bodybuilders.
Depending on the nature of the inflammation, there are several types of mastitis:
- serous;
- infiltration;
- purulent.
Together they form 3 successive stages of development of the inflammatory process - from the appearance of the first symptoms in the form of serous exudate to active suppuration of the area of inflammation with the discharge of pus. Based on the type of localization of purulent structures, two more forms can be distinguished:
- phlegmonous - with the spread of pus throughout the entire volume of the affected tissue;
- abscess - with clear localization and delimitation of purulent contents from adjacent tissues.
In advanced cases, a gangrenous form may develop with tissue necrosis and septic complications, which poses a high risk to the patient’s life. The only way out in this situation is complete removal of the mammary gland and adjacent lymph nodes.
Mastitis: symptoms
The composition of the symptom complex depends on the stage of the disease:
- Stage 1 – serous: slight hyperemia and swelling of the glandular tissue, pain on palpation (may radiate to the area of the axillary lymph nodes).
- Stage 2 - infiltration: swelling and soreness increase, a compaction is clearly palpable in the glandular tissue, the temperature rises sharply, regional lymph nodes enlarge, signs of intoxication appear, and general well-being worsens.
- Stage 3 – purulent: the severity of symptoms reaches its peak, purulent exudate appears. In the lactation form, purulent-bloody discharge can be seen in the milk (in this case, breastfeeding must be stopped).
In severe cases of mastitis, the symptoms may become more complicated - a general increase in temperature, fever, intoxication, and enlarged axillary lymph nodes are possible. In the absence of treatment, a gangrenous form develops with septic damage to the body.
Diagnosis of the disease
Acute mastitis is diagnosed during a medical examination and tissue palpation. The procedure allows you to find out the localization of the inflammatory process, check for symptoms, and collect information on your medical history. The chronic form requires differential diagnosis with a tumor process, mastopathy and other diseases of the mammary glands. Based on the results of the preliminary diagnosis, the doctor will refer you for additional examination using instrumental and laboratory methods.
Basic techniques:
- Ultrasound of the mammary glands - reveals characteristic thickening of the subcutaneous tissue, expansion of the milk ducts, shows the location of infiltration zones, abscesses and necrotic areas;
- aspiration biopsy of the breast with histological examination of the inflammatory infiltrate;
- collecting milk for bacteriological testing (for lactation mastitis);
- mammography (rarely prescribed, only in controversial cases of chronic disease).
Recommendations
Breast mastitis requires immediate action and adequate treatment. To achieve a speedy recovery and not harm your health, you need to adhere to the following recommendations:
- Treatment of mastitis should be trusted only to qualified specialists. Independent actions can lead to negative consequences and the transition of the disease to a more complex stage.
- To achieve effective results, you cannot ignore the recommendations of your doctor.
- When identifying the first signs of mastitis, you need to refrain from thermal procedures and regularly express milk.
Only professional treatment of mastitis will help get rid of the inflammatory process and avoid its reappearance.
Elimination of symptoms and treatment of mastitis
Mastitis is treated by a gynecologist and mammologist. In some cases, the help of an endocrinologist and surgeon will be required. A timely visit to a doctor is of great importance, since when mastitis passes into a purulent abscess form, surgical intervention becomes inevitable. In this case, an opening of the purulent focus is prescribed, followed by tissue drainage. Serous and infiltration mastitis can be cured using conservative techniques.
Attention! During treatment for lactation mastitis, you should stop breastfeeding. Reason: Breast milk contains bacterial toxins and antibiotics, which can harm the baby.
The main groups of drugs for drug treatment:
- antibiotics – to suppress and/or completely eliminate the infectious pathogen;
- painkillers and antipyretics as symptomatic treatment;
- drugs that suppress lactation (when the pathology becomes purulent);
- immunostimulants and vitamins - to maintain the body and improve resistance to infections;
- detoxification agents.
Ultrasound, magnetic therapy, phonophoresis, and darsonval are used as physical procedures. At home, cool compresses, including those based on herbs with an anti-inflammatory effect, are actively used to relieve pain and reduce inflammation.
Attention! Self-medication of mastitis is unacceptable - any miscalculation can lead to serious complications, including sepsis and necrosis. Advanced forms may require complete removal of the gland and adjacent lymph nodes. Home therapy methods can only be used after consultation with a doctor as an accompanying treatment.
Operation process
Before the operation, the patient receives general anesthesia, which eliminates pain. To remove the abscess, a radial incision is made in the area where the compaction has formed.
After a careful dissection, the surgeon removes the abscess and examines the internal cavity. After this, the wound is treated with a special antiseptic solution and drainage is performed. Sutures are most often not applied to avoid repeated leakage of purulent discharge.
The postoperative period is always accompanied by the use of antibacterial drugs. This promotes rapid healing and destruction of pathogenic microorganisms.
After completing the course of treatment, the patient undergoes tests again to rule out the presence of infection.
Surgical intervention in some cases can affect the lactation function of the mammary gland. Therefore, nursing mothers need to take care of their health and visit a doctor at the first suspicion of mastitis.
Prevention
Measures to prevent lactation mastitis in women:
- Prevent stagnation of breast milk. Get advice about breastfeeding and, if necessary, pumping using special breast pumps.
- Attach your baby to the breast correctly. Make sure it completely covers the nipple and areola. Do not allow breastfeeding to be done “in vain”, without milk being sucked out.
- Maintain breast hygiene. Carefully prepare your nipples for feeding - this will prevent the appearance of microcracks and their subsequent infection.
- Try to visit a mammologist regularly - an experienced doctor will be able to determine the onset of the disease before the first unpleasant symptoms appear. This will greatly simplify treatment.
To prevent non-lactation mastitis, you should carefully monitor the general condition of the body. The trigger for pathology can be constant stress, hypothermia, poor environment, and too little physical activity. An important part of the prevention of inflammation of the mammary glands (including for men and children) is timely diagnosis and timely elimination of hormone imbalance.
How to diagnose?
Breast cancer can mimic the symptoms of mastitis. To exclude oncology and confirm the disease, an examination is required.
It includes:
- Ultrasound – allows you to detect a lesion in the mammary gland, determine its size and shape;
- microscopy of milk - with mastitis, a microbial pathogen, remains of pus and leukocytes will be detected;
- A blood test will show an increase in ESR and a shift of the formula to the left, which indicates inflammation.
A biopsy will show the final point in diagnosis - but it is not always prescribed when previous methods do not allow a differential diagnosis.