How does phimosis manifest in boys: symptoms and treatment methods
Many parents notice phimosis in young boys, but not all adults know that it is important to constantly monitor the condition of the genitals. The head of the penis is covered by the foreskin; attempts to open it cause pain. Sometimes the skin duplication is so dense that serious urological problems appear and inflammatory processes develop.
Parents of a newborn boy should know what to do if the baby's head of the penis is not exposed. Panic and confusion are bad helpers after identifying a sensitive problem. According to statistics, physiological phimosis in children occurs in more than 90% of boys under 1 year of age. The article describes the causes, types, and methods of treating phimosis in boys of different ages.
Classification
It should be understood that phimosis is not a disease, but a special condition that is associated with the physiological characteristics of the body (age), heredity and damage to the tissue of the foreskin. In this regard, the following forms of phimosis are distinguished:
- Physiological – occurs in most boys before the onset of puberty, and is associated with the functional maturation of the preputial cavity. It is not a pathology and resolves on its own after 7 years.
- Pathological – occurs as a result of inflammation, injury, metabolic disorders and requires treatment;
- Hypertrophic (proboscis);
- Atrophic;
- Scar.
The incidence of one form or another of phimosis directly depends on age. In children, in the overwhelming majority of cases, it is physiological in nature, and in men it is caused by cicatricial changes.
Reasons for the development of pathological phimosis
If infant natural phimosis goes away on its own, then there is phimosis, which has the form of a disease. It is provoked by several reasons:
- genetic disorders in the development of skin tissue of the penis;
- infectious diseases (especially of the genitourinary system);
- inflammation or injury to the penis (most often occurs when the child is carelessly washed or examined);
- failure to comply with hygiene rules.
All these reasons are provocateurs for the development of the disease, which is fraught with serious complications (for example, acute urinary retention).
Treatment
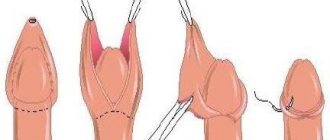
The main treatment method is circumcision. The indication for surgical treatment is the presence of cicatricial phimosis.
However, there are contraindications to circumcision, or circumcision, namely: hypospadias, hidden penis. Also, the operation cannot be performed in the presence of local infections or coagulopathies: in such cases, surgical treatment is carried out after correction of concomitant diseases to eliminate the increased risk of infectious and other complications after surgical treatment.
There are also non-operative treatment methods for mild forms of the disease. In this case, hormonal ointments are used locally, on the area of the foreskin, and mechanical stretching of the foreskin is performed. These treatments are aimed at eliminating the inflammatory process and preventing the possibility of new scars forming. However, conservative treatment is not always appropriate and effective, so the choice of treatment method can only be determined during a face-to-face consultation with a specialist.
Symptoms
The basic symptom of phimosis in boys or adult men is the partial or complete inability to expose the head of the penis.
In addition, the patient may experience:
- Decreased potency.
- Pain during urination.
- If inflammation is activated, purulent discharge may be observed, the temperature may rise significantly and the lymph nodes on the body will significantly enlarge.
- Disorders of urination - fluid flows slowly, in drops or in a thin stream, the preputial area is swollen due to the accumulation of urine there and the impossibility of its rapid removal.
- With paraphimosis, a sharp pain develops in the head and penis, the pinched foreskin turns blue, the genital organ itself increases in size and becomes inflamed - this requires urgent surgery.
A doctor's help is necessary for the following symptoms of phimosis:
- increased body temperature;
- insufficient stream when urinating;
- swelling of the head of the penis;
- inflammation of the head of the penis;
- blue discoloration of the head of the penis;
- inability to fully open the head of the penis in children over seven years of age;
- enlarged lymph nodes located in the groin;
- the appearance of pus even with light pressure on the head of the penis;
- severe pain when urinating (small children cry for a long time after this process);
- drip urine output (in very severe forms).
The appearance of at least one of these symptoms indicates that phimosis has gone from safe, self-limiting with age, to pathological, requiring urgent treatment. In this case, leaving the child without treatment and waiting for the exacerbation of phimosis to go away on its own is not worth it. This can significantly worsen the child's condition and lead to much more complex treatment. For those mothers who do not want or do not have the opportunity to see a doctor to solve the problem, traditional medicine will come to the rescue, which is easy to use at home.
Physiological, pathological…
Phimosis is a narrowing of the foreskin of the penis, manifested in pain or the inability to expose its head. Depending on the severity of the narrowing, it is customary to distinguish between physiological and pathological phimosis. As a rule, physiological phimosis occurs in most children under 2-3 years of age. Until now, doctors have not come to a common opinion as to what age phimosis should be considered physiological, when it is necessary to operate on a child, etc. It should also be taken into account that physiological phimosis has all the same complications as pathological phimosis. The question of the advisability of the operation and its timing for “childhood phimosis” is decided individually, in each specific case. Most often, phimosis in children goes away on its own, the head opens and problems with the foreskin do not arise. But until the head is opened, you need to pay special attention to its hygiene and treat the head at least once a day with antiseptic drugs. Now most experts believe that by the age of 6-7 years the head of the penis should open freely, and if this does not happen, then surgery is necessary. As for phimosis in adult men, it can persist since childhood, or it can develop over time, during puberty. This period is characterized by rapid growth and development of the genital organs. Sometimes, a discrepancy may appear between the development of the penis and the foreskin, when the flesh is smaller than the head, its opening is narrower, and it is difficult or impossible to open the head. Most often, this is phimosis of 1-2 degrees, but phimosis preserved from childhood can be at least 3 degrees.
Paraphimosis
A common condition that develops in boys with phimosis. It is important to always remember: under no circumstances should you use great force when trying to expose the head of the penis. The fact is that it gradually expands in the direction from the opening of the urethra, and the shaft of the penis itself is much narrower. As a result of the forced opening of the head, the foreskin stretches somewhat (this can cause a short-term feeling of pain), and then tightly wraps the ring around the penis behind the head.
Manifestations of paraphimosis:
- the head is enlarged and swollen;
- the boy experiences a feeling of severe pain (babies cry and do not allow him to touch the penis).
The compressed blood vessels no longer perform their function, and the tissues of the head begin to lack oxygen and nutrients. If measures are not taken in a timely manner, necrosis or gangrene of the penis may develop, which forces doctors to remove the affected area - the patient becomes disabled.
Surgery
There are many surgical techniques. In young children, in some cases, surgery is used to separate synechiae in the area of the glans penis using surgical instruments.
The most optimal treatment method is complete removal of the foreskin - circumcision, or circumcision. Only with this method of treatment is the substrate for the development of the disease completely eliminated and the possibility of relapse of the disease is prevented. In children, surgery is performed under general anesthesia; in adults, surgery can be performed under local anesthesia. The operation takes from 20 to 30 minutes, depending on the choice of technique.
There are a very large number of surgical treatment methods. The most common is circular excision.
In some cases, after the operation, an elastic bandage is applied for 1 day.
Stages of development
According to the severity of the process, 4 degrees of phimosis are distinguished:
- In a calm state, the head is completely released; during an erection, its removal is difficult and painful;
- At rest, the head of the penis is difficult to remove; during erection, it is completely covered by the foreskin and cannot be released;
- The head can be partially withdrawn only at rest;
- The head is constantly hidden by the foreskin and is not visible. During urination, urine first fills the preputial sac and only then is released drop by drop.
Phimosis keeps pace with age
In adolescents, young men and adult men, phimosis steadily progresses, this is due to the appearance of erections, masturbation and sexual activity. During an erection, the head of the penis enlarges and the foreskin stretches tightly. In this case, small cracks and microcracks appear on the foreskin; they do not bleed and do not cause any concern. But as they heal, a scar or microscar forms in their place. Scar tissue is less elastic than normal foreskin tissue, therefore, with the appearance of each new scar, the foreskin narrows more and more, and the disease progresses. This process is especially pronounced during sexual intercourse; ruptures of the foreskin can be significant and accompanied by heavy bleeding.
How to treat phimosis in boys?
Treatment of phimosis in children depends on its degree, as well as the age of the patient. Depending on the extent of the process, the recommended approaches are listed in the table below.
| Phimosis degree | How to treat? |
| IV | Conservative treatment is ineffective; surgical intervention is necessary. |
| III | If possible, conservative methods are used at home; if conservative treatment does not help, phimosis in boys is eliminated with surgery. |
| II | At home, ointments are used and methods of gradually stretching the tissues of the foreskin are used. Any manipulations are carried out only in accordance with the recommendations of the urologist. |
| I | In boys under 13 years of age, no special treatment is required. |
The following methods can be used:
- Drug treatment. It is the use of hormonal ointments, such as Clobetasol, Bepantel, Betameson, Solcoseryl. They are needed to increase tissue elasticity, relieve inflammation, and heal microcracks.
- Non-medicinal. This treatment for phimosis in boys at home consists of mechanical regular retraction of the foreskin. You should move the baby's foreskin by one millimeter twice a week. First you need to take a warm bath for 15 minutes with any antiseptic (decoction of chamomile, calendula or a weak solution of potassium permanganate). It is advisable to lubricate the problem area with baby cream. The maximum movement can be up to 2 mm; sudden jerks are unacceptable. These manipulations should be carried out only after instructions from a urologist.
FIMOSIS physiological, hypertrophic, cicatricial. Pathology of the foreskin.
Assessment of the condition of the foreskin (PF) in pediatric practice remains a subject of discussion among pediatricians, pediatric surgeons, and urologists. When examining children, due attention is often not paid to age-related characteristics. There is no common point of view in defining the concept of phimosis in pediatric practice, there are no clearly defined boundaries between normality and pathology, treatment tactics and preventive measures for diseases of the foreskin have not been worked out. There is no unity among doctors regarding synechiae (fusions of the head with the inner layer of the foreskin). Many surgeons do not know how to deal with the accumulation of smegma in the preputial sac, and how dangerous its presence is for the occurrence of balanitis. The tactics of managing patients with purulent-inflammatory diseases of the foreskin are discussed. Is it necessary to circle and remove the head in acute inflammatory processes? Practical recommendations on methods of general hygiene and methods of caring for a boy in infancy and early childhood are often written by non-specialists and by people far from practical experience. Such advice may create more problems for the child than it is worth. Our study was devoted to solving all these issues.
Material and methods.
During the period from 1996 to 2004, in the Tushino Children's Hospital, St. Vladimir Hospital, children's clinic No. 140 of the North-Western Administrative District, in the Semashko children's clinic in Moscow, in the department of planned surgery and in the clinic in Taganrog, 3235 boys with pathology of the foreskin were examined. The condition of the foreskin was assessed in children with other diseases during hospitalization in the departments of the listed clinics and at outpatient consultations with a pediatric surgeon and a pediatric urologist-andrologist. The children's ages ranged from 8 days to 17 years.
Based on the analysis of large clinical material, it was possible to more clearly formulate the definition of “physiological” phimosis and, taking into account the structural features of the foreskin, identify other options for narrowing of the preputial sac.
The term phimosis
- is of Greek origin, means “muzzle” (muzzle, muzzle, muzzle, snout), this is a pathological condition in which it is impossible to remove the head (6).
The main cause of phimosis in adult patients is the presence of a dense, scarring ring of the foreskin. Treatment is only surgical, by excision of scar tissue. A generalized definition of phimosis, used by adult surgeons, is unacceptable in pediatric practice; treatment tactics should also be different. According to our observations, in the majority of boys (87%) under 3 years of age it is not possible to open the glans penis, and in 43% it is impossible to even see part of the glans without injury to the preputial sac. However, this does not mean that all of them require surgery. The main reason for this “physiological” narrowing of the foreskin
is the congenital narrow opening of the preputial sac at the junction of the outer layer of the foreskin into the inner one.
The concept of physiological phimosis has no age limits and can occur at any age (in a newborn and a 16-year-old teenager). Upon examination, the following characteristic features of physiological phimosis can be noted. The skin of the foreskin has no scar changes, is soft, and stretches well (Fig. 1).
However, when trying to quickly or roughly remove the head, radial cracks occur in the area of the junction of the inner and outer leaves of the preputial sac. The deepest tears in the foreskin can be observed during the simultaneous removal of the head in boys with physiological phimosis.
| Fig. 1 View of the foreskin of a 2.5 year old child with physiological phimosis. |
These manipulations are accompanied by episodes of bleeding, severe swelling of the foreskin, pain and difficulty urinating, up to acute urinary retention. Significant tears in the foreskin often heal with the formation of rough scars. That is why we consider all attempts to simultaneously remove the head
. In order to assess the degree of narrowing of the foreskin and the condition of the skin of the preputial sac, it is absolutely not necessary to completely remove the head (retract the foreskin beyond the coronal groove). Moreover, this manipulation is meaningless (has no medical indications), is sharply painful and very harmful. Even more dangerous are recommendations for parents to carry out a one-step removal of the head on their own, at home. The tendency of the preputial sac to edema in childhood, the traumatic and painful nature of manipulation predispose to the development of paraphimosis. We observed pinching of the head extended beyond the coronary groove by the foreskin in 29 boys. The periods of infringement ranged from 2 hours to 15 hours. Conservative reduction of the head was performed in 25 children, but 4 boys were operated on and required incision of the foreskin to immerse the head in the preputial sac.
Over the past 15 years, we have abandoned any attempts to simultaneously remove the head of the penis, but have used a technique of gradual gentle stretching of the foreskin
developed in the clinic (St. Vladimir Hospital). The method is based on two principles. The first is a slow impact on the narrowed area of the preputial sac; treatment continues for months; there is no reason to rush. The glans penis should be open by puberty (12-15 years). These dates are determined by hormonal changes in the boy’s body. It is important to remember that free removal of the head is necessary only for painless sexual intercourse. The second principle is that the foreskin should be stretched as gently as possible; even minimal trauma (tear, cracks) of the narrowed area is not allowed. After each procedure, which was carried out 2 times a week, it is necessary to achieve stretching (displacement) of the preputial sac by 1-2 mm, from the original, no more. To improve the stretching of the foreskin, before manipulation, it is recommended to take a hygienic bath with decoctions of medicinal herbs (chamomile, string, celandine), lasting 10-15 minutes. Skin steamed in warm water stretches more easily and is less damaged. After the procedure, it is advisable to treat the foreskin with baby cream or solcoseryl for better epithelization of occasionally occurring micro tears.
The procedures described were performed initially by a physician. Then, after a detailed explanation of the goals and objectives of this technique, gradual gentle stretching of the foreskin was carried out by the parents at home. The doctor’s task was to monitor the dynamics of the process of displacement of the foreskin. In the vast majority of cases (91%), it was possible to open the head of the penis halfway within 2-3 months. We consider this effect of treatment to be a good result (Fig. 2 A-B).
| Fig.2. A. View of the foreskin of a 2.5 year old child with physiological phimosis. |
B, C – results of conservative treatment of physiological phimosis using the technique of gradual gentle stretching of the foreskin after 1 month. and 2 months..
Similar procedures were subsequently recommended to be carried out once every 2–3 weeks to maintain skin elasticity. We did not strive to achieve mandatory complete removal of the head in young children, since its further opening may be difficult due to the presence of dense fusions of the head with the foreskin ( synechiae)
).
Modern ideas about the nature of synechiae and accumulations of smegma in the preputial sac differ from those previously existing in the domestic literature. Currently, there is no consensus on the surgeon's tactics in relation to these conditions.
The classic description of normal embryonic development of the foreskin has existed since 1949 (Gairdner D). The development of the preputial sac in the fetus begins between 3 and 5 months. gestation. And by the time of birth, the foreskin covers the head of the penis to the meatus (4.8). The glans penis and foreskin develop from the same tissues of the distal part of the penis during the 3rd month of pregnancy. The foreskin arises as a fold of skin at the base of the glans penis and grows by extending above this base. Its growth on the dorsal side occurs more intensively than on the ventral side. Since in the early stages of pregnancy the urethra is not closed, but represents a urethral groove, the foreskin on the ventral side develops from two paired outgrowths. (Fig. 3 A, B).
Following the fusion of the urethral platform into a tube, sections of the foreskin move along the lateral surfaces of the head, covering the urethra from above, and merge with each other, forming a frenulum.
| Rice. 3. The head of the human fetal penis. A. at the 16th week of gestation, the urethral folds extend along the ventral surface along the shaft of the penis. Later they connect along the midline. The rudiments of the foreskin are located mainly on the dorsal surface and gradually creep on both sides of the head. B. After the 20th week of gestation, the urethra on the glans is completely closed, the lateral masses of the foreskin have merged together in the area of the frenulum of the penis. |
The epithelial lining of the inner layer of the foreskin and the head of the newborn is made up of flat keratinizing epithelium, “fused” together. Thus, the surface of the head and inner leaf of the PC are in a state of “epithelial adhesion,” which is considered a physiological state (1). Smegma formation, according to various sources, begins at birth or at 3-4 months. life. Epithelial cells become keratinized, desquamated and form “infantile smegma.” In addition to the keratinized epithelium, most of the smegma is the secretion of the sebaceous glands of the skin (3). The resulting infantile smegma is sealed in the preputial space between the epithelium of the head and the skin of the foreskin, so the likelihood of infection of the infantile smegma is negligible. The latter gradually migrates to the top of the glans, that is, natural cleansing of the prepuce cavity and separation of the fusion of the glans penis with the foreskin occurs (8). This process continues from birth to prepuberty. And at 11-15 years old, in 62.9% -73.7% of boys, the head of the penis is open. (8,9).
Based on the above, it becomes obvious that fusion of the head and preputial sac up to 11-15 years of age can be considered the norm, therefore the separation of adhesions (adhesions) and removal of “infantile smegma” does not have direct medical indications. Assessing the results of such manipulations (circling the head) at follow-up after 4-6 months, we observed re-formation of adhesions and accumulation of smegma in 32% of children. The only reason for dividing synechiae may be the inflammatory process of the foreskin, caused by the presence of infected smegma. However, it is incorrect to associate smegma formation with the causes of balanitis, since smegma is present in 99% of boys, and balanopastitis was detected in only 6% of examined patients.
It was noted that in the puberty period of 11-15 years, under the influence of hormonal changes, synechiae become looser and the process of their separation occurs much easier, less painful, without the appearance of extensive erosive surfaces on the head. On the contrary, according to our research, the separation of fusions of the glans with the foreskin in children 3-5 years old, very often (up to 85%) ends with a recurrence of synechia with an even more severe scarring process, in cases where the parents stopped regularly opening the head of the penis. Two boys, 14 and 15 years old, with rough cicatricial fusions of the foreskin with the head after repeated circling in early childhood required surgery to cut off the foreskin fused with the head for 2-3 cm.
Variants of phimosis in pediatric practice.
Physiological phimosis -
3096 (87%)
Hypertrophic phimosis
(proboscis foreskin)
- 168 (2.7%)
Cicatricial phimosis (classic)
All patients with pathology of the preputial sac who were included in this study 3235 (examined in clinics and hospitals) were conditionally divided into four groups. First
, the most significant
group (3096) 87%
consisted of children with
physiological phimosis
or normal, unstretched foreskin with a congenitally narrowed opening of the preputial sac without signs of skin scarring. The children did not require medication or surgical treatment; gentle, gradual stretching of the foreskin was carried out. The boys did not require strict outpatient monitoring of the condition of the preputial sac and were considered practically healthy.
Second group
(168) 2.7% were children diagnosed with
hypertrophic phimosis
or
proboscis foreskin.
It is important to note that the majority (142) of the boys (82.5%) from this group were malnourished and had varying degrees of obesity.
The foreskin of these children had excess length and resembled a proboscis, which is explained by the accumulation of subcutaneous fatty tissue in the pubic area and, as a consequence, displacement of the skin of the shaft of the penis towards the foreskin. When trying to remove the head, a section of the skin of the foreskin was clearly visible in the form of a dense ring ( Fig. 4 A, B),
| Fig. 4 A. A 4-year-old child with hypertrophic phimosis. |
Excess of foreskin resembling a proboscis. B.
When trying to remove the head, a section of the skin of the foreskin was clearly visible in the form of a dense ring, which was very poorly stretched, easily injured, radial skin cracks and capillary bleeding occurred, so it was not possible to visualize the external opening of the urethra.
However, we did not observe cicatricial changes in the skin in this group of patients. Children with hypertrophic phimosis required strict outpatient monitoring of the condition of the foreskin. These patients received conservative treatment in the form of gradual, gentle stretching of the foreskin after warm hygienic baths with herbal decoctions. To achieve the therapeutic effect of stretching the elongated narrowed part of the preputial sac in hypertrophic phimosis, it took significantly more time than in the case of physiological phimosis. On average, conservative therapy lasted up to 3-5 months. A positive result was achieved in 156 patients (92.2%). However, 12 boys required surgical treatment. Indications for circumcision in hypertrophic phimosis should be seriously limited, since the usual circumcisio operation has a number of complicating aspects. Economical resection of the foreskin can lead to recurrence of phimosis. Significant excision of the skin of the preputial sac is often accompanied by the appearance of a hidden penis. Outside of erection, the penis disappears into the surface of the body and hides in the surrounding tissues of the subcutaneous fatty tissue of the pubic region and scrotum (Fig. 5).
| Fig.5. An 8-year-old child after circumcision of the foreskin due to hypertrophic phimosis. Outside of erection, the penis is hidden in the surrounding tissues of the subcutaneous fatty tissue of the pubic region. |
We observed similar complications of the treatment of hypertrophic phimosis in 4 patients operated on in other medical institutions. All children with a hidden penis underwent surgery to isolate the penis from the surrounding tissues, form the contour of the penis, and fix the skin in the peno-abdominal and scrotal angles. If there is cicatricial phimosis in combination with a hypertrophic foreskin and surgical treatment is necessary, the operation of choice may be economical resection of the foreskin with the formation of a contour of the penis.
Third group
Of patients (342), 9.6% were boys with
cicatricial phimosis.
Based on anamnestic data, we tried to find out the causes of scar changes on the foreskin. However, in the majority of patients 134 (39.1%), cicatricial narrowing of the preputial sac occurred against the background of complete health. Signs of balanopastitis shortly before the onset of scarring of the foreskin were observed in 122 (35.6%) patients. Traumatic simultaneous removal of the head preceded cicatricial phimosis in 76 patients (22.2%).
Depending on the clinical manifestations, we conditionally divided all patients with cicatricial phimosis into two subgroups. The first subgroup consisted of 189 boys (52.2%) with uncomplicated
cicatricial phimosis (Fig. 6) .
| Fig.6 A. A 5-year-old child with signs of uncomplicated cicatricial phimosis. There is a dense scar ring of the foreskin wider than the external opening of the urethra. There are no signs of inflammation. |
B.V
. Complicated cicatricial phimosis. The skin of the foreskin shows signs of inflammation, the opening of the foreskin is point-shaped, sharply narrowed (urination is difficult).
Visually, the foreskin was changed slightly, there were no signs of inflammation (swelling, hyperemia, infiltration of the tissues of the preputial sac), urination was not impaired. All children urinated freely, painlessly, in a wide stream.
When trying to remove the head, a dense scar ring was identified, which did not allow examining the head. The diameter of the cicatricial ring of the foreskin was significantly greater than the external opening of the urethra, so there were no signs of urination problems. The second subgroup consisted of boys with complicated cicatricial phimosis
153 (44.7%)
(Fig. 6 B, C).
The foreskin of these children was swollen and somewhat hyperemic. The opening of the foreskin is point-shaped, sharply narrowed, in a dense cicatricial conglomerate. Urination is impaired, in a thin sluggish stream, painful, with a significant expansion in the form of a ball of the preputial sac. In fact, the child initially accumulated urine in the preputial sac, and then evacuated the urine out through the opening of the foreskin narrowed by the scar.
Patients with cicatricial phimosis required surgical treatment. With uncomplicated phimosis, the timing of the operation can be arbitrary and surgical intervention can be postponed for some time. Complicated phimosis, accompanied by signs of bladder outlet obstruction, requires urgent planned surgery in the near future. As a short-term preoperative preparation, it is possible to recommend treating the external opening of the foreskin with anti-scar ointments (contractubex).
Purulent-inflammatory diseases of the foreskin (PF)
were identified in 214 boys, which is 6% of all examined patients. Signs of acute balanopastitis were observed in 96 of them (44.8%). The diagnosis of fungal infection of the foreskin was established in 118 boys (55.1%). Acute balanopastitis and fungal inflammation have similar clinical manifestations, however, the treatment of these diseases is fundamentally different. The correct differential diagnosis allows you to clarify the nature of the lesion.
In case of acute balanopastitis
children complained of pain in the glans penis, itching, burning sensation when urinating, and in rare cases there was acute urinary retention (in 2 patients). The foreskin was swollen and hyperemic, and in 55 cases (57%) there was discharge of pus from the preputial sac. An important diagnostic sign in patients with acute balanopastitis was the presence of synechiae and accumulation of infected smegma (causes of inflammation). Physiological phimosis was detected in 83 boys (86%) with acute inflammation of the preputial sac.
Treatment of acute balanopastitis has undergone some changes in recent years. Fundamentally, we consider it important to refuse to remove the head; this is not necessary, and this procedure against the background of inflammation is extremely traumatic and is accompanied by severe scarring of the preputial sac in the future. Experience in treating patients with balanopastitis has shown that complete circular division of the synechia of the foreskin with a button probe is not necessary. These procedures are extremely painful for the child and are accompanied by significant mental trauma. The surgeon is obliged to drain the purulent focus. For this, palpation of the foreskin or local revision of the foreskin at the site of greatest swelling and hyperemia is quite sufficient. After draining the pus, it is advisable to complete the procedure by introducing antibacterial ointments into the preputial sac (levomykol, syntomycin emulsion, dioxykol, etc.). At home, the child was prescribed sitz baths with herbal infusions of chamomile, string, celandine, calendula or a weak solution of potassium permanganate KMn04 3-4 times per day for 6-8 days. After each bath, it was recommended to treat the glans penis (external opening of the foreskin) with antibacterial ointment. Relief of the inflammatory process was noted on days 3-4. Indications for complete circumference of the head were rare cases (2 children, 2%) of persistent inflammation.
A distinctive feature of fungal inflammation
or the so-called chronic balanitis was the complete absence of synechiae, accumulations of smegma in the preputial sac. There were no patients with physiological or cicatricial phimosis in this group of children. The head opened completely easily. The inner layer of the foreskin looked hyperemic, swollen, the mucous membrane was dull, wrinkled, fibrin deposits and an unpleasant odor were noted. From the anamnesis it turned out that most children used manganese baths and treated the foreskin with soap for an excessively long period. Fungal spores were identified in flora cultures from the surface of the foreskin. Treatment of fungal balanitis included antifungal drugs (nystatin, Diflucan) by mouth. Local nystatin, diflucan, mycoseptin - ointments. It is recommended to exclude antibacterial drugs and antiseptic solutions (topically). Reduce the number of different baths and exercise more drying effects on the skin of the foreskin.
We have offered the following recommendations for hygienic care of a boy’s genitals:
— there is no need for daily opening of the head and treatment with water, soap or disinfectants;
- in the absence of inflammatory phenomena, it is sufficient to perform hygienic baths with herbal decoctions (chamomile, string, celandine, sage, calendula) 2 times a week, without removing the head;
- use of KMnO4, furacillin, antibacterial ointments only as indicated.
Conclusion.
Thus, based on the work performed, the following conclusions were made.
- Synechiae of the foreskin is a normal physiological condition caused by different stages of the formation of the preputial sac. Does not require special treatment. Complete separation of synechiae is indicated at prepubertal age (11-12 years); before this period, fusion of the preputial sac with the head is considered acceptable.
- Smegma and “infantile smegma” - a product of desquamation of the keratinizing epithelium, the secretion of the sebaceous glands of the preputial sac and head is observed in all children, independently migrates and is evacuated. “Infantile smegma” is difficult to consider as a direct cause of balanopastitis and its surgical evacuation is not justified.
- The procedure for one-step complete removal of the head has no medical indications, is pointless, very painful, traumatic and harmful. Even more dangerous are recommendations to parents to carry out one-step complete removal of the head on their own, at home (paraphimosis).
- The technique of gradual gentle stretching of the foreskin makes it possible to achieve opening of the head in children with physiological phimosis within 1-2 months. In children with hypertrophic phimosis - within 2-4 months.
- Physiological phimosis is a congenital narrow opening of the preputial sac at the junction of the outer layer of the foreskin into the inner one. The skin of the foreskin has no scarring, is soft and stretches well. The concept of physiological phimosis has no age limits and can occur at any age in a newborn and in a 15-year-old teenager.
- Pathology of the foreskin has age-related characteristics. Phimosis is not only cicatricial, but also physiological and hypertrophic. Treatment tactics for pathology of the preputial sac depend on the severity of scar changes on the skin of the foreskin.
- Circumcision with hypertrophic phimosis is dangerous due to the occurrence of relapse and hidden penis. Recurrence of phimosis often occurs when attempting to preserve the foreskin (plastic surgery – up to 2.4%)
- Surgical treatment is indicated for children with cicatricial phimosis; conservative measures are not effective. The method of choice is circumcision of the foreskin with mandatory complete excision of scar tissue.
- For patients with chronic inflammation of the foreskin, it is first necessary to exclude fungal infection.
- When treating acute balanopastitis in children, removal of the head is contraindicated (trauma to the preputial sac); there is no need to circumcise the head. It is quite enough to ensure drainage of infected smegma and hygienic baths with the introduction of antibacterial ointments 3-4 times a day.
Video material on this topic can be viewed at the link www.youtube.com/watch?v=y2JkcJMQkPI /
When is surgery needed?
In many children, physiological phimosis gradually decreases and goes away on its own, without requiring any treatment, much less surgery. Therefore, if nothing bothers the child, it is quite possible to do without surgical intervention. But there are cases when surgery for phimosis in boys is necessary:
- inflammation is regular, and treatment of phimosis does not produce results;
- urination becomes painful;
- adhesions form between the head and foreskin;
- severe swelling with paraphimosis;
- phimosis does not go away until puberty.
If one of the reasons suits you, do not panic too much; in fact, the operation for phimosis is simple, done under local anesthesia and takes only a few minutes. And literally in one or two days you will be able to return home.
In case of developed balanoposthitis, conservative therapy includes the following measures:
- warm baths with a solution of potassium permanganate - 5 times a day for 4 days; treatment with furacillin - according to the same scheme;
- introduction of antiseptic ointments into the preputial sac - 3 times a day for 6 days;
- lubricating the affected area with petroleum jelly - 2 times a day, 7 days.
External antibacterial therapy can be different and is determined in each specific case individually. Antibiotic-based emulsions and powders may be prescribed. When performing the procedure, the foreskin must be moved from the head.
Prevention
Parents need to keep their child's genitals clean. It is recommended to wash the boy with clean warm water every evening. The rest of the time you can use wet wipes. The use of foam for bathing is not recommended. These products contain chemicals that irritate the delicate skin of the penis.
With physiological phimosis, there is no need to expose the head of the penis while swimming. If a child develops inflammation due to dirt accumulated under the foreskin, then it must be removed from there as follows:
- Draw 10 ml into a syringe without a needle. clean warm water or ectericide solution (furatsilin can be used instead).
- Pull the foreskin upward so that the head of the penis is hidden rather than exposed.
- Insert the syringe into the gap that has formed between the foreskin of the penis and its head (this procedure is more convenient to carry out together).
- Release the liquid, thus washing away accumulated dirt.
- Repeat this procedure 1 or 2 more times.
- Drop 2-3 drops of olive or Vaseline oil into the gap between the foreskin of the penis and its head (you can use oil solutions of vitamin A, E).
It is imperative to change diapers for a small child more often. Thanks to this, there will be no prolonged contact of the head of the penis with feces and urine. The inflammatory process will not occur.
BALANOPOSTHITIS
A purulent inflammatory disease that develops due to poor hygiene of the penis. This develops infrequently in children, because in very young boys, the discharge from the penis and mucous membranes contains almost no harmful bacteria. With age, smegma (the secretion produced by the mucous membrane of the foreskin) begins to have an increasingly complex composition, so hygiene must be more careful. And this is difficult, if the foreskin remains impossible to retract, balanoposthitis may develop.