- Treatment of dysmenorrhea
- Attending doctors
- Prices for services
Dysmenorrhea (algodysmenorrhea) is a menstrual disorder characterized by pain during menstruation. According to statistics, more than half of women of reproductive age complain of painful menstruation. In order to avoid dangerous complications, it is very important to diagnose the pathology in a timely manner and undergo a course of treatment.
We are talking about dysmenorrhea only if the pain syndrome is severe enough. According to various sources, approximately every tenth woman experiences significant pain that is cyclical in nature and associated with menstruation. Moreover, in many cases, patients note not only pain, but also a noticeable deterioration in their general condition, decreased performance, changes in psycho-emotional state, and forced abandonment of the usual rhythm of life.
Causes of dysmenorrhea
The main causes of dysmenorrhea:
- congenital defects that appear as a result of exposure to negative factors during the period of intrauterine development of the fetus - a closed accessory vagina, a closed uterine horn. During menstruation, blood accumulates in the accessory structures, causing intense pain. Sometimes such formations reach quite large sizes, the pain becomes very severe and is even accompanied by a short-term loss of consciousness. The intensity of the pain increases with each menstrual cycle, forcing the patient to see a doctor;
- spasm of the smooth muscles of the uterine body, caused by deviations in the synthesis and metabolism of prostaglandins and thromboxanes. These are biologically active substances that are produced in almost all organs and structures. Some of them are the main mediators of pain and inflammation, others regulate the tone of smooth muscles, and others are responsible for the condition of the microvasculature. By acting on the myometrium, prostaglandins provoke intense contraction of myocytes, which is externally manifested by severe pain. It should be noted that pathological abnormalities can be either congenital or acquired;
- hormonal imbalance, especially excess estrogen in combination with progesterone deficiency. Estrogen is produced by the ovaries; the corpus luteum, which appears after ovulation at the site of the burst follicle, is responsible for the production of progesterone. An increased amount of estrogen increases myometrial spasm, which leads to pain;
- endometriosis is a gynecological nosology of a chronic nature, which is manifested by the appearance of pathological foci of endometrioid tissue. These lesions, like the normal inner lining of the uterus, are susceptible to cyclic changes - in the first half they grow, in the second they are rejected. The process is accompanied by the accumulation of blood, the development of inflammation and the formation of adhesions in the affected area;
- ovarian tumors, especially those producing hormonal substances;
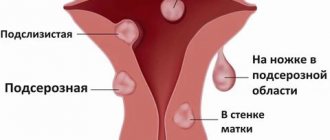
- fibroids are benign neoplasms of the uterus that develop from the myometrium. This is one of the most common gynecological diseases. According to statistics, fibroids are diagnosed in every fourth woman. The main symptom of fibroids is heavy and prolonged periods, often with the release of blood clots. The pain is cramping in nature, reminiscent of a feeling of heaviness. If the fibroid is located close to the peritoneum, dyspepsia and severe pain in the entire abdomen often occur;
- an incorrectly installed or misaligned spiral is a structure made of a polymer material with the addition of metal. This is a reliable means for preventing unwanted pregnancy, which is installed in the uterine cavity. If for some reason the IUD has moved, or was initially installed incorrectly, it can cause severe menstrual pain and intense bleeding;
- varicose veins of the small pelvis, accompanied by inflammation;
- diseases of the reproductive system of an infectious nature - endometritis (inflammation of the endometrium), salpingitis (inflammation of the fallopian tubes), adnexitis (inflammation of the fallopian tubes and ovaries). Most often, these processes are provoked by pathogenic microflora, infection of which occurs through unprotected sexual contact. When the ovaries are involved, in addition to direct inflammation, there is a disruption in the production of hormones;
- formation of adhesions in the pelvis. Adhesions are rather dense formations, peculiar cords, consisting mainly of collagen fibers. By preventing the normal contraction and relaxation of the uterus during menstruation, adhesions cause quite intense pain (read more here);
- incorrect position of the uterus, as a result of which expulsion of the functional layer of the endometrium and bleeding is difficult;
- delayed sexual development, genital infantilism;
- suffered injuries to the genital organs.
Depending on the cause, dysmenorrhea is of two types - primary and secondary.
Premenstrual syndrome
Premenstrual syndrome is a collection of symptoms that occur during the second half of the menstrual cycle and include weight gain, acne, hot flashes, swelling, diarrhea or constipation, mood swings, breast tenderness and hardness, and depressive symptoms. About 90% of women may have symptoms of premenstrual syndrome (PMS), 5% of them lose their ability to work during the corresponding days of the menstrual cycle.
Pathogenesis . The exact mechanism of development of PMS is unknown, but its numerous physiological and psychological causes have been established. The most common hypotheses for the pathogenesis of PMS include estrogen-progesterone imbalance (progesterone deficiency), hyperprolactinemia, fluctuations in steroid hormone levels, disorders of the renin-angiotensin-aldosterone system and electrolyte balance, vasopressin; excessive production of prostaglandins; impaired synthesis of neurotransmitters (monoamines, acetylcholine), other hormones (androgens, glucocorticoids, melatonin and insulin), decreased endogenous synthesis of endorphins or impaired sensitivity of receptors to endogenous opiates. Modern theories of the pathogenesis of PMS prefer a violation of serotonin secretion as a primary or secondary cause of the development of this syndrome.
Assuming normal metabolism, serotonin levels rise and fall throughout the day. An increase in serotonin levels is accompanied by a need for protein intake; the drop in serotonin levels then begins a new cycle. With PMS, serotonin levels do not reach the trigger level for protein consumption, even after eating carbohydrates. So, patients with PMS tend to increase their consumption of sweets.
The administration of progesterone, the deficiency of which was previously considered responsible for the development of PMS, helps only a small proportion of patients, and in many cases can worsen the condition of patients. Progesterone helps increase plasma levels of MAO (MAO) during the menstrual cycle. According to one theory, an increase in MAO levels correlates with the development of depression due to catecholamine deficiency. Symptoms of fluid retention (weight gain, swelling, breast hardening) with PMS, as well as some emotional symptoms, may be associated with increased levels of renin, angiotensin and aldosterone. A direct aldosterone antagonist, spironolactone (veroshpiron), usually reduces the symptoms of PMS.
Treatment of premenstrual syndrome is often carried out by exclusion - if one group of drugs is ineffective, other treatment options are prescribed. In 1/3 of patients with premenstrual syndrome, significant improvement is achieved through the use of an adequate diet. The diet consists of reducing the consumption of simple carbohydrates (sugar) in favor of complex ones (fruits, vegetables), reducing salt, fat, but sufficiently consuming proteins. In order to increase the production of endogenous opiates, dosed physical exercise is recommended. In some cases, homeopathic medicines (Dysmenorm, Menalgin, Remens, etc.) can be effective.
Nonsteroidal anti-inflammatory drugs reduce the production and effects of prostaglandins and may also be effective. For pain and hardening of the mammary glands, it is recommended to prescribe bromocriptine at a dose of 5 mg/day. Oral contraceptives usually reduce the manifestations of premenstrual syndrome by blocking ovulation and suppressing the endometrium (reducing the synthesis of prostaglandins), as well as normalizing the estrogen-progestin ratio.
The theory of the development of premenstrual syndrome due to fluctuations in the level of steroid hormones has been confirmed in a number of studies on the effectiveness of GnRH agonists (zoladex, diferelin, decapeptyl, lupron) in reducing the manifestations of PMS.
When significant edema develops, diuretics are used (veroshpiron, Lasix, furosemide). Patients with depressive disorders, loss of appetite, sleep disorders, autistic reactions, and withdrawal from social life may require the prescription of psychotropic drugs - alprazolam (Xanax) and fluoxetine hydrochloride (Prozac).
Primary dysmenorrhea
This is a functional disease, manifested by a typical clinical picture without pathologies of the reproductive system. It usually appears at a young age, several years after the start of the first menstruation. As a rule, the pain is minor at first, but the condition worsens every year. The lower abdomen begins to hurt on the first day of menstruation, or a few hours before it begins. The duration of discomfort varies from 1 to 3–4 days. The reasons for this condition are not exactly known, however, there are suggestions that primary dysmenorrhea
occurs due to the action of biologically active substances produced in dead endometrial cells - prostaglandins E2 and E2-α.
Sources
- Parmigiani G., Mandarelli G., Tarsitani L., Roselli V., Gaviano I., Buscajoni A., Biondi M., Girardi P., Ferracuti S. Perceived Stress and Life Events in Patients Affected by Schizophrenia and Schizoaffective and Bipolar Disorder : Is There a Role for Self-Reported Basic Symptoms? // Psychopathology - 2021 - Vol - NNULL - p.1-8; PMID:33910198
- Kim S.Y., Kim S.I., Lim W.J. Association between change in sleep duration and posttraumatic stress symptoms in natural disaster victims: the mediating role of resilience. // Sleep Med - 2021 - Vol82 - NNULL - p.110-116; PMID:33910160
- Ahmed F., Maclean RH., Nihtyanova SI., Ong VH., Murray CD., Denton CP. Autoantibody Predictors of Gastrointestinal Symptoms in Systemic Sclerosis. // Rheumatology (Oxford) - 2021 - Vol - NNULL - p.; PMID:33909895
- Maia CS., Araújo PSR., Schindler HC., Soares JP., Cruz AS., Queiroz Júnior JRA., Tenorio FDCAM., Medeiros JP., Tenorio BM., Maciel GES., Amorim RVDS., Hinrichsen SL. Treatment of mycobacteriosis in a patient with compatible symptoms after a cesarean delivery. // Rev Inst Med Trop Sao Paulo - 2021 - Vol63 - NNULL - p.e37; PMID:33909851
- van der Valk JPM., Heijboer FWJ., van Middendorp H., Evers AWM., In 't Veen JCCM. Case-control study of patient characteristics, knowledge of the COVID-19 disease, risk behavior and mental state in patients visiting an emergency room with COVID-19 symptoms in the Netherlands. // PLoS One - 2021 - Vol16 - N4 - p.e0249847; PMID:33909639
- Lin RSY., Yu DSF., Pui Hing Chau P., Li PWC. An empowerment-psycho-behavioral program on neuropsychiatric symptoms in persons with mild cognitive impairment: Study protocol of a randomized controlled trial. // J Adv Nurs - 2021 - Vol - NNULL - p.; PMID:33909293
- Amendola S., Hengartner MP., Spensieri V., Grillo L., Cerutti R. Patterns of internalizing symptoms and disability functioning in children and adolescents. // Eur Child Adolesc Psychiatry - 2021 - Vol - NNULL - p.; PMID:33909142
- Smith LC., Tieu L., Suhandynata RT., Boomhower B., Hoffman M., Sepulveda Y., Carrette LLG., Momper JD., Fitzgerald RL., Hanham K., Dowling J., Kallupi M., George O Cannabidiol reduces withdrawal symptoms in nicotine-dependent rats. // Psychopharmacology (Berl) - 2021 - Vol - NNULL - p.; PMID:33909102
- Phelps R., Van Scoyoc A., Marquardt M. Parental Misattribution of Environmental Stress Reaction Symptoms to Autism. // J Dev Behav Pediatr - 2021 - Vol42 - N4 - p.264-271; PMID:33908901
- Lima MP., Moret-Tatay C., Irigaray TQ. Locus of control, personality, and depression symptoms in cancer: testing a moderated mediation model. // Clin Psychol Psychother - 2021 - Vol - NNULL - p.; PMID:33908672
Secondary dysmenorrhea
It is caused by pathological changes in the pelvic organs, such as developmental anomalies, inflammatory processes, etc. The presence of an intrauterine device may also be a cause. Most often, clinical manifestations of the secondary process appear after 30–35 years. Pain and other symptoms of dysmenorrhea usually begin 2-4 days before the start of menstruation and may continue even after it ends. The causes are disturbances in blood flow to the pelvic organs, as well as stretching of the walls of the uterus, myometrial spasms and pathological changes in tissue. Secondary dysmenorrhea
can be distinguished from the primary one by the presence of concomitant symptoms of the main pathology, as well as during examination by a gynecologist.
Prevention
Gynecologists advise that if you have any problems during menstruation, contact competent specialists. It is easier to treat any disease in the initial stages of development. You should not wait until dysmenorrhea enters the decompensated stage; its therapy will take a long time.
Since in most cases a woman experiences secondary algodismenorrhea due to inflammatory processes, endometriosis or benign neoplasms, for prevention it is worth being examined by a gynecologist twice a year.
You also need to follow simple doctor’s recommendations:
- Lead a healthy lifestyle.
- Establish a regular intimate life.
- Eat right, including in your diet foods that are healthy for the female body: grains, vegetables, fruits.
- Maintain a sleep-wake schedule.
- Do not self-medicate any illness.
Dysmenorrhea can lead to prolonged depression and other mental disorders (bulimia), and advanced pathologies, which result in menstrual irregularities, will lead to infertility. Therefore, it is important to contact a gynecologist on time and monitor your own health.
The information is provided for informational purposes only! If you have questions, we recommend making an appointment with a gynecologist.
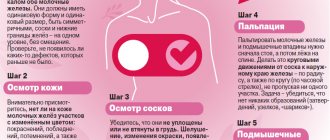
Symptoms of dysmenorrhea
The main symptom is pain in the abdominal area, mainly lower. This condition is called algomenorrhea. The pain can be aching, pulling or cramping. Often there are changes in the general condition, manifested in the form of weakness, dizziness, nausea, bloating, increased body temperature and loss of appetite. Such symptoms of dysmenorrhea can be severe, which significantly impairs the physical and mental state of a woman. Approximately 15% of women are forced to take sick leave in the first 1–3 days of menstruation.
With secondary dysmenorrhea, the above symptoms are accompanied by signs of the underlying pathology that caused the cycle disruption.
Diagnosis of dysmenorrhea
Typically, diagnosing dysmenorrhea is not difficult, since women independently describe all clinical manifestations. The presence of secondary dysmenorrhea can be detected by undergoing an examination by a gynecologist and a series of laboratory and instrumental tests.
The most informative in terms of diagnosing dysmenorrhea are:
- laboratory determination of hormone levels in the blood in different phases of the cycle;
- ultrasonography;
- endoscopic examination - colposcopy, hysteroscopy;
- computed tomography or magnetic resonance imaging.
Laboratory determination of hormones in different phases gives the doctor an idea of the regularity of the cycle, the functioning of the ovaries, hypothalamus and pituitary gland, and thyroid gland.
Expert opinion of a doctor
Barakhoeva Zarema Bekhanovna
Reproductologist, obstetrician-gynecologist, Ph.D.
During an ultrasound examination, you can see an incorrectly located uterus, tumors, adhesions, and a displaced helix. Hysteroscopy helps diagnose endometriosis, endometrial polyps and other disorders of the lining of the uterus. CT and MRI are prescribed in doubtful cases, mainly for differential diagnosis.
If a tumor is suspected, a biopsy and pathomorphological examination of the obtained material is indicated. Such a diagnosis of dysmenorrhea will make it possible to make a correct final diagnosis, practically eliminating the possibility of error.
Treatment of dysmenorrhea
Regardless of the reasons and the age at which the diagnosis was made, dysmenorrhea requires treatment, first of all, to alleviate the woman’s general condition, as well as to prevent disability. Treatment of primary dysmenorrhea involves taking medications aimed at blocking the action of prostaglandins. These include non-steroidal anti-inflammatory drugs such as Ibuprofen, Naproxen, Diclovit and Nimesulide. These medications also have an analgesic effect. Combined oral contraceptives have a good effect. In case of significant pain, it is possible to take analgesics or antispasmodics (Analgin, Sedalgin and No-shpa)
Sometimes a preventative course is prescribed - taking anti-inflammatory drugs 3-5 days before the onset of menstruation.
The duration of such treatment is 3 menstrual cycles. Treatment of dysmenorrhea as a secondary phenomenon is aimed at treating the underlying gynecological pathology that caused this manifestation. Analgesics are prescribed to eliminate pain and alleviate the general condition. The choice of drug, dosage and methods of use are determined by the doctor after interviewing and examining the patient.
Particular attention is paid to physiotherapeutic procedures. Relaxing baths with extracts of pine needles, mint and lemon balm normalize the functioning of the central nervous system. A course of 10–15 baths is enough to stabilize the central nervous system. Electrosleep has a similar effect. Ultratonotherapy improves blood supply to internal organs, normalizes the tone of blood and lymphatic vessels, and improves metabolism. Sunbathing also has a noticeable effect. Sun rays improve the functioning of the immune system, activate regenerative processes, and normalize metabolism. The procedures are recommended to be taken in the morning and evening hours. Electrical stimulation of the cervix allows you to regulate the functioning of the hypothalamic-pituitary system by activating peripheral receptors and triggering reflex reactions. If necessary, the patient is recommended psychotherapy sessions. These can be both group and individual sessions, the type of which is selected by the psychotherapist.
About pain during the menstrual cycle
Dysmenorrhea (painful menstruation) is a menstrual disorder characterized by pain during menstruation. According to statistics, more than half of women of reproductive age complain of painful menstruation. In order to avoid dangerous complications, it is very important to diagnose the pathology in a timely manner and undergo a course of treatment.
We are talking about dysmenorrhea only if the pain syndrome is severe enough. According to various sources, approximately every tenth woman experiences significant pain that is cyclical in nature and associated with menstruation. Moreover, in many cases, patients note not only pain, but also a noticeable deterioration in their general condition, decreased performance, changes in psycho-emotional state, and forced abandonment of the usual rhythm of life.