Answered by Alexandra Andreevna Metelina, pediatrician and gastroenterologist at CTA.
Very young children (up to one year old) suffer from appendicitis extremely rarely; other diseases accompanied by abdominal pain and general malaise are more common in this group. For example, intussusception, acute pyelonephritis, or an intestinal infection (viral or bacterial) may present with similar symptoms.
It is believed that children 3-4 years old are not prone to appendicitis. But I have more than once seen appendicitis in a four-year-old child while on duty in a hospital, and inflammation of the appendix develops rapidly, sometimes with lightning speed. Therefore, let's talk about the symptoms in detail so that you notice them in time and call a doctor immediately.
How to recognize appendicitis at 2-3 years old
You should be alerted by drowsiness, lethargy, refusal of your favorite food, cartoons, unusual silence and indifference to your signals and suggestions. Characteristic symptoms also include a sharp increase in temperature to (38-40) C and complaints of abdominal pain. At the same time, don’t expect that the answer to the question “Where does it hurt?” the baby will show you the right half of the abdomen, its lowest square, the right iliac region, where (as most adults know) the appendix is located. He will most likely move his hand all over your belly and most likely point at your belly button. In this age group, it is difficult for doctors to suspect appendicitis. A clue is often given by the baby’s forced position (on his left side with his legs pulled up). When you try to lift the child or pull the right leg towards the stomach, the child will resist your actions, scream or cry. If, when pressing on the left side of the abdomen or tapping, the child grabs the right side, it is likely appendicitis and it is time to seek professional help.
Sources
- Gilligan LA., Trout AT., Davenport MS., Zhang B., O'Hara SM., Dillman JR. Variation in imaging outcomes associated with individual sonographers and radiologists in pediatric acute appendicitis: a retrospective cohort of 9271 examinations. // Eur Radiol - 2021 - Vol - NNULL - p.; PMID:33880622
- Reimer RP., Heneweer C., Juchems M., Persigehl TT. . // Radiologe - 2021 - Vol61 - N5 - p.497-510; PMID:33860818
- Raoudha K., Amel T., Nesrine J., Najla S., Samia B., Sana M., Jihene B., Abdellatif N., Samia T., Lamia B. Bilateral pheochromocytoma revealed by acute abdominal pain in a child. A case report. // Pediatr Endocrinol Diabetes Metab - 2021 - Vol - NNULL - p.; PMID:33853288
- Valitutti F., Verde A., Pepe A., Sorrentino E., Veneruso D., Ranucci G., Orlando F., Mastrominico A., Grella MG., Mandato C. Multisystem inflammatory syndrome in children. An emerging clinical challenge for pediatric surgeons in the COVID 19 era. // J Pediatr Surg Case Rep - 2021 - Vol69 - NNULL - p.101838; PMID:33846690
- Belgacem A., Miane H., Fillali W., Hangard P., Ponthier L., Ballouhey Q. Hemolytic uremic syndrome following complicated appendicitis in a child: what is the missing link? // J Int Med Res - 2021 - Vol49 - N4 - p.3000605211006952; PMID:33840247
- Choi S.Y. Comparison of Clinical Characteristics According to the Existence of Secondary Appendicitis in Pediatric Acute Enterocolitis: A Single Center Study. // Pediatr Gastroenterol Hepatol Nutr - 2021 - Vol24 - N2 - p.127-134; PMID:33833968
- Fadgyas B., Garai GI., Ringwald Z. How does COVID-19 pandemic influence paediatric acute appendicitis cases? // Orv Hetil - 2021 - Vol162 - N16 - p.608-610; PMID:33830938
- Sharma K., Tomar S., Sharma S., Bajpai M. Floating appendix: post-traumatic amputation of the appendix as sequela or complication?: a case report. // J Med Case Rep - 2021 - Vol15 - N1 - p.192; PMID:33827681
- Moratilla Lapeña L., Delgado-Miguel C., Sarmiento Caldas MC., Estefanía K., Velayos M., Muñoz-Serrano A., De Ceano-Vivas M., López-Santamaría M., Martínez L. Impact of SARS- CoV-2 pandemic on emergency department activity at the pediatric surgery unit of a third-level hospital. // Cir Pediatr - 2021 - Vol34 - N2 - p.85-89; PMID:33826261
- Vaziri M., Nafissi N., Jahangiri F., Nasiri M. Comparison of the appendicitis inflammatory response and Alvarado scoring systems in the diagnosis of acute appendicitis in children. // J Med Life - 2021 - Vol14 - N1 - p.75-80; PMID:33767789
How to recognize appendicitis at 4-7 years of age and older
At this age, children can usually clearly show where it hurts. If the child has a typical location of the appendix - in the right iliac region - he will clearly show you the place where it hurts. It will be much more difficult for a child whose appendix is hidden in the left half of the abdomen, under the liver and closer to the kidneys - behind the peritoneum; in this case, the child will point to other areas of the abdomen. But if these pains are accompanied by vomiting and/or stool disturbances, and the temperature rises to 38.5-39, the likelihood of appendicitis is high. At this age, when the appendix is inflamed, children also remain in a lying position on their left side with their legs tucked in, lose their appetite and do not want entertainment. Approach the child every half hour and stroke the belly, lightly pressing it in the lower half on the left and right. If the pain intensifies over time, you must call an ambulance.
Possible symptoms
When appendicitis develops, a child may experience:
Nature of pain in appendicitis
- Nausea ending in vomiting. Inflammation of the appendix is characterized by a wave-like appearance of attacks of nausea: it can disappear completely and then return with greater force. The appearance of vomiting indicates severe intoxication of the body. As a rule, with appendicitis it will be single.
- The appearance of plaque on the tongue. This is one of the most likely signs of inflammation of the appendix. A dense layer of gray, beige or milky color is located in the center of the tongue. Difficult to remove with a spoon. The child’s breath remains clean, which eliminates the exacerbation of pathologies of the digestive system.
- Temperature. The initial stage proceeds with a slight increase in its indicators. A rise in temperature above 38 degrees indicates the involvement of all layers of the appendix in the inflammatory process.
- Changes in the consistency of stool. In approximately 15% of children, an attack of appendicitis is accompanied by the development of diarrhea. Feces are abundant, liquid in composition, without an unpleasant odor, and may contain particles of undigested food.
Important! With appendicitis, a child may complain of pain both when urinating and when bowel movements.
What do the tests say?
If appendicitis is suspected, a complete clinical blood test (CBC) and a general clinical urinalysis (UCA) are taken; it is advisable to do this within the first hours after the onset of the disease. In a general blood test for appendicitis, there should be high leukocytes and a large number of band neutrophils, and the ESR may also increase. But if a child has appendicitis, a urine test is usually normal. And if the urine is not sterile, with bacteria, white blood cells and red blood cells - together, both of these tests indicate a urinary tract infection or renal colic, and you will certainly be referred for an ultrasound and to a pediatrician for antibacterial therapy.
If you have taken tests in the laboratory without calling a doctor, and you see that all urine indicators are normal, and leukocytes, neutrophils and ESR are above normal, do not offer the child any more water or drink, pack a bag with things (passport , policy, birth certificate, SNILS, slippers, pajamas, hygiene products), call an ambulance or go to the hospital yourself.
Attention! Do not give your child any painkillers until examined by a doctor; do not place a heating pad or ice on his stomach so that the picture of appendicitis is not blurred. Your actions can complicate the diagnosis and waste time.
Recovery after appendectomy
With uncomplicated appendicitis, recovery occurs quickly; complications require longer hospitalization and a longer period of postoperative rehabilitation.
Factors contributing to early recovery: early diagnosis and timely surgery, absence of concomitant diseases, young age, absence of complications.
Risk factors: late hospitalization, obesity, elderly and senile age, peritonitis, sepsis, multiple concomitant diseases.
Within a month after removal of appendicitis you should:
- limit physical activity, especially stress on the abdominal muscles;
- follow a diet that excludes vegetables, fruits, essential oils, smoked meats, animal fats, fried, spicy foods, foods rich in purines and cholesterol (red meat, lard, jelly, strong broths, packaged soups, smoked meats, fatty fish, legumes, canned food) , raspberries, figs, grapes, eggs, cottage cheese, butter, margarine, fatty dairy products.
With the modern level of development of medicine, appendicitis is treatable, but much depends on timely access to a doctor and correct behavior after surgery.
What will happen in the hospital.
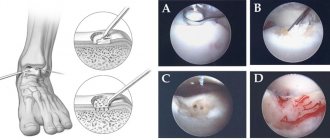
In the emergency room, the child will have an ultrasound and will be examined by a surgeon. If the appendix is inflamed, and tests confirm this, if you have not fed or watered the child for at least 3.5 hours, he will be immediately taken to the operating room. There, using laparoscopy (these are 3 small punctures), the inflamed appendix will be removed through a small hole and a healthy baby will be returned to you, completely free of appendicitis. After 4 hours he will be able to get up and drink water, but all this is only if you have time before the complications begin. If for some reason laparoscopic surgery is not possible, abdominal surgery will be performed and the recovery period will take longer.
Indications for appendectomy
Surgery to remove the appendix is used for chronic or acute forms of appendicitis. In addition, appendectomy is performed if there is an appendiceal infiltrate, as well as if neoplasms are detected in the appendix.
Emergency appendectomy is usually performed no later than one hour after diagnosis. In case of chronic appendicitis or appendicular infiltrate, surgery to remove appendicitis is performed as planned.
What to do to prevent appendicitis, and can it be cured without surgery?
Currently, the only method of treating appendicitis - from the point of view of evidence-based medicine - is surgical treatment, but research is also being conducted on conservative therapy (“Is conservative therapy for acute appendicitis possible?” Prof. S.A. Sovtsov, Prof. A.G. Krieger, Candidate of Medical Sciences O.V. Pribytkova, A.V. Smirnov, Federal State Budgetary Educational Institution of Higher Education "South Ural State Medical University" of the Ministry of Health of Russia, Federal State Budgetary Institution "Institute of Surgery named after A.V. Vishnevsky" of the Ministry of Health of Russia, 2021 .; Early appendectomy vs. conservative management in complicated acute appendicitis in children: A meta-analysis. Fugazzola P, Coccolini F, Tomasoni M, Stella M, Ansaloni L., General and Emergency Surgery dept, Bufalini Hospital, Cesena, Italy. Pediatrics dept. and Neonatal and Pediatric Intensive Care Unit, Bufalini Hospital, Cesena, Italy. 2019, etc.). Yes, of course, people who lead a healthy lifestyle and adhere to a rational, age-appropriate diet have a lower chance of encountering appendicitis. But there is no absolutely effective prevention. Let's proceed from the fact that we all benefit from preventing constipation and regular physical activity - all this allows us to stimulate intestinal function and avoid the formation of fecal stones and spontaneous spasms in the gastrointestinal tract.
The appendix is a branch of the cecum ranging from 4 to 20 centimeters in length and only 1 centimeter in diameter. This worm-like appendage is located where the small intestine meets the large intestine. Bacteria easily colonize in this place and fecal stones can get stuck, so the appendix, consisting of lymphoid tissue, performs immune and protective functions in relation to the intestines. (The tonsils and adenoids protect the respiratory organs in the same way.) Inflammation of the appendix often occurs when its mouth is blocked, usually due to the accumulation of fecal stones. The appendix can also become inflamed after a spasm of the intestines due to the consumption of large amounts of protein foods, fast carbohydrates and foods rich in fats, against the background of an intestinal infection that provokes excessive growth of bacteria in the intestine. In all cases, vasospasm, blood stagnation and swelling of the smooth muscles of the intestines occur. Because of this, the nutrition of the appendix is disrupted, bacteria from the intestinal lumen penetrate the walls of the appendix, and an active inflammatory process begins, which is almost always accompanied by pain.
About Lisa, Yasha and Dima - real stories from mothers
Lisa (8 months old) had a sharp rise in temperature, she cried without interruption for more than an hour, her tummy seemed larger than usual, she had loose stools, and a few hours after the temperature spike, she began to lie down, pulling her legs towards her stomach. I gave her Nurofen, but there was no change in Lisa’s condition, and we went to the hospital. (Later we realized that it was not worth giving Nurofen and wasting time). At the hospital, doctors first suggested an intestinal infection or disease of the abdominal cavity, and also said that this could be a change in the anatomy of the intestine. They did a blood test and found high white blood cells, a high ESR (about 90 units), and a urine test showed no signs of inflammation. Lisa then had an ultrasound, which at first showed nothing but severe flatulence, which made it difficult to see anything else. Then the ultrasound diagnostician began to scrutinize the area of the intestine where the appendix was, and finally saw that it was very inflamed. Diagnosis: acute phlegmonous appendicitis with local peritonitis. A few minutes after the ultrasound, Lisa was already on the surgical table. The laparoscopic surgery went well, Lisa recovered quickly. The doctors told us that we did absolutely the right thing by arriving at the hospital almost immediately, and we, in turn, are very grateful to the doctors for the high-quality diagnosis and successful operation. (Lena, Lisa's mother).
Yasha (6 years old) fell ill with the coxsackie virus at sea, in Turkey. He developed a high temperature, characteristic spots appeared on his legs and arms, and his appetite decreased - everything is as usual with a viral infection. After a couple of days, the temperature dropped, but he did not eat better, even refused ice cream, and drank only water. He was lethargic and thoughtful, but never complained of abdominal pain. We called a doctor, the doctor examined Yasha, and then for the first time, while palpating his abdomen, Yasha screamed that he was in pain. The doctor said that this is most likely a consequence of inflammation caused by the coxsackie virus, it’s okay, continue therapy, and if the temperature persists, come and take a blood test. We asked the question: is this appendicitis? - and received the answer that no, this is pain caused by a virus, due to which, apparently, the liver or intestines were slightly inflamed. It was on Friday, and on Saturday morning Yasha was already holding his stomach, pressing his leg to his stomach and could not get to the toilet on his own. We took him to the hospital in our arms, where he was immediately given a blood test, which showed very high leukocytes and ESR, and an ultrasound revealed that the appendix (yes, it was appendicitis) had already burst. After 20 minutes, Yasha was already on the operating table; the abdominal surgery lasted an hour and a half. Unfortunately, we were unlucky with a general practitioner, and we ourselves did not have sufficient information about how to recognize appendicitis. Please don't repeat our mistakes. (Zhenya, Yasha’s mother).
Dima (10 years old) began to complain of headache and nausea, he vomited several times and was put to bed. I decided that it was a rotavirus, because such cases had happened before. By evening, the temperature rose to 37.8, Dima did not want to eat anything, he drank water and lay down. In the morning the temperature was 37.2, there was no appetite, I insisted that I at least eat oatmeal with water. During the day, Dima complained for the first time of abdominal pain, not severe, according to him. I was at work all day, we called each other, his condition did not change, his stomach did not hurt more. In the morning everything was the same, the temperature remained at 37.2-37.5 and I called a pediatrician from the Central Clinical Hospital and went to work (there was a nanny at home). About two hours later the doctor called me and said that she was calling an ambulance to Dima because there was a serious suspicion of appendicitis. The ambulance arrived with me, Dima was taken to the clinic in Polyanka, they did a blood test, an ultrasound, and immediately took him to surgery. The surgeon said that in just a couple of hours the appendix would have burst, and then laparoscopic surgery would not have been possible. I concluded that when complaining of abdominal pain, even minor ones, the first step is to rule out appendicitis and not trust any of your previous experiences. And, of course, it’s good when there are wonderful, attentive doctors nearby!..)) (Irina, Dima’s mother)
Gut is thin
Intestinal intussusception also occurs in young children, which also gives a picture of an acute abdomen. What happens? The intestine of the lower section is “implemented” into the overlying one. Due to the resulting narrowing, the intestinal vessels are pinched and blood circulation is disrupted.
The main danger is that necrosis (death of tissue) of the intestine may develop. In infants, intussusception most often occurs due to improper introduction of complementary foods with vegetables or fruits, which increase peristalsis. Moreover, this happens much more often in boys than in girls. In older children, the cause may be an abnormal protrusion of the wall of the small intestine, polyps on the inner wall of the intestine, a tumor and other pathologies that impair motility. Very often the disease develops suddenly:
● The child cries, breaks out in sweat, bends over, twists his legs.
● After the first attack, which lasts 5–10 minutes, the child becomes lethargic and apathetic until the next attack. As the attacks become more frequent, bloating develops.
● Blood is visible in the stool.
● Vomiting may occur, after which peristalsis can be heard; vomit contains blood mixed with mucus, resembling raspberry jelly.
● Sometimes between attacks you can feel a lump in the intestines - a “bump” in the tummy.
● Your temperature may rise.
If such symptoms appear, the child must be hospitalized immediately. If no more than 12–18 hours pass from the first attack of pain to the start of treatment, the strangulated area of the intestine can be saved.
To establish a diagnosis of intussusception, the child is given an x-ray: an enema with a barium sulfate solution is given so that the damaged area becomes “visible” during examination.
If time is not lost, air is pumped into the colon through the rectum, and under the influence of pressure it gradually straightens.
When the child is brought to the hospital too late, surgery is necessary. It can be performed using laparoscopy: the surgeon manually, applying slight pressure, straightens the damaged area. In cases where necrosis of the intestinal tissue does occur, the surgeon cuts out the damaged area and then stitches the healthy edges of the intestine.
Differential diagnosis
As has already been said many times, appendicitis can disguise itself as a variety of diseases, therefore, its differential diagnosis is carried out with a host of pathologies:
- acute cholecystitis,
- viral mesadenitis,
- pyelonephritis on the right,
- renal colic on the right,
- acute right-sided adnexitis,
- ovarian cyst rupture
- ectopic pregnancy,
- exacerbation of peptic ulcer disease,
- intestinal obstruction, etc.
After doctors are convinced of the correctness of their diagnosis, the patient is immediately treated, which can only be surgical.
Contraindications for laparoscopic appendectomy:
- late stages of pregnancy;
- severe blood clotting disorders;/li>
- undergone operations on the abdominal organs;/li>
- severe cardiovascular and respiratory failure;/li>
- abnormal location of the appendix;/li>
- old age;/li>
- pronounced adhesive process;/li>
- widespread peritonitis requiring sanitation and drainage of the abdominal cavity;/li>
- dense appendicular infiltrate;/li>
- gangrenous appendicitis./li>
Preparing for an appendectomy:
In acute appendicitis, preparation for appendectomy is carried out promptly; as a rule, the condition of the patient's cardiac and respiratory systems is assessed.
For a planned operation , the results of blood tests, urine tests, fluorography, and an electrocardiogram are required. Women need to be examined by a gynecologist to rule out inflammatory processes that can lead to complications.
You should not take food or water for at least six hours before surgery. In case of laparoscopic surgery, it is necessary to first perform an ultrasound of the abdominal cavity.