Home » Intestinal dysbiosis
Intestinal dysbiosis is a common pathology that is associated with disorders of the gastrointestinal tract. Many medical experts argue that this is not a disease, but intestinal dysfunction, which is the result of pathology or poor lifestyle. Symptoms of intestinal dysbiosis in adults have different intensity, frequency, and character. If left untreated, it leads to serious complications and consequences.
With normal microflora and undisturbed peristalsis, the large intestine contains a small number of microbes that should be in the body of every person. Microorganisms and bacteria perform important functions for the human body.
What is intestinal dysbiosis in adults?
Dysbacteriosis is the opposite state of normbiocenosis. Intestinal activity decreases and food processing takes much longer. Microflora and intestinal motility worsen. Opportunistic bacteria appear in the human body, which disrupt the functioning of internal organs.
A lack of lactobacilli and necessary microorganisms leads to disruption of intestinal function. The digestion process worsens, metabolism slows down, and immunity decreases. There is a lack of nutritional components in the body. The digestive tract becomes weakened and reacts to environmental influences.
The human intestine contains beneficial and pathogenic bacteria. The average weight of the first group is two kilograms. There are more than five hundred varieties of such microorganisms. The following components are considered the most common:
- bifidobacteria;
- lactobacilli;
- coli.
Pathogenic bacteria include:
- peptococci;
- Candida mushrooms;
- staphylococci;
- clostridia.
There are not as many harmful bacteria released as beneficial ones. In a healthy person, bacteria are located in the body and do not manifest themselves, since the body has a strong immune system. If the immune system weakens, then certain symptoms appear.
Necessary microorganisms are responsible for the synthesis of vitamins, for lowering cholesterol levels, for processing food and absorption into the intestinal walls. Metabolism occurs.
Sources
- Yu.V. Yudina, Doctor of Medical Sciences, Prof. A.A. Korsunsky, Doctor of Medical Sciences, Prof. A.I. A minova, G.D. Abdullaeva, Doctor of Medical Sciences, Prof. A.P. Prodeus “Intestinal microbiota as a separate system of the body”, Evidence-based gastroenterology, 2021, T. 8, No. 4-5, p. 36-43.
- Zimmerman Ya.S. Gastroenterology: a guide. – 2nd ed., revised. and additional – M.: GEOTAR-Media, 2015. – 816 p.: ill.
- T.Yu. Demidova, K.G. Lobanova, O.Sh. Oinotkinova “Intestinal microbiota as a risk factor for the development of obesity and type 2 diabetes mellitus,” Therapeutic archive, 10, 2021.
- Monograph edited by E.L. Nikonova and E.N. Popova "MICROBIOTA".
Causes of intestinal dysbiosis in adults
The causes of intestinal dysbiosis have different etiologies. Disturbed microflora is always caused by certain factors. The reasons that influence the appearance of dysbiosis are as follows:
- deficiency of enzymes responsible for food processing;
- weakness of the intestinal muscles that must process food;
- increased acidity or alkali level in internal organs;
- deficiency of substances that promote the growth of essential bacteria;
- excessive number of parasites in the intestines.
You can cure an intestinal disease only if you are sure of the cause that influenced the appearance of the pathology. The above factors may be caused by the following reasons:
- diseases of the gastrointestinal tract, such as gastritis, duodenal ulcer, colitis;
- viral, fungal, parasitic infections;
- congenital or acquired structural disorders of the gastrointestinal tract;
- a disrupted diet consisting of fried and fatty foods;
- genetic predisposition
- environmental damage, environmental situation in the region;
- excessive physical activity, especially in men;
- excessive consumption of alcoholic beverages, which kill microflora;
- long-term use of antibiotics and other medications;
- nervous tension (this factor is common among females);
- pregnancy or hormonal imbalances;
- fasting or sudden change of diet;
- reduced immunity;
Allergic reactions can also provoke intestinal dysbiosis. Very often, the disease occurs in people who are associated with climate change and often travel. The body needs to adapt and get used to a different climate zone.
University
→ Home → University → University in the media → “War” of intestinal microflora, or 10 questions about dysbiosis
The human body is home to up to 1016 microorganisms. This is more than 10 times the number of his own cells.
About 60% of microflora is found in the gastrointestinal tract. Any failure in the coordinated work of the microcosm can cause problems in many systems and functions.
1. What is dysbiosis? You can often find other designations - dysbiosis and enhanced microbial growth syndrome.
The term “dysbacteriosis” was proposed in 1916 by the German scientist Alfred Nissle, using this word to designate a quantitative change in E. coli. In 1972, the Soviet physiologist Alexander Ugolev described dysbiosis as a change in the qualitative and quantitative composition of the intestinal bacterial flora, which occurs under the influence of poor nutrition, physical and mental stress, serious illnesses, taking antibacterial drugs, surgical interventions, immunodeficiency, environmental pollution, etc. In our country, the term “dysbacteriosis” was introduced into medical use by academician Alexander Bilibin (1897–1976) to name qualitative and quantitative changes in the microbiocenosis of the intestine, especially the large intestine, disturbances in the species and quantitative composition of microbial populations in a certain biotope. Russian scientist Professor Yakov Zimmerman proposed the term “dysbiosis”: it reflects changes not only in the bacterial flora, but also in fungi, as well as metabolic, trophic and other disorders of the macroorganism associated with disturbances in the intestinal microecology. Today, the terms “dysbacteriosis” and “dysbiosis” are disputed and even denied by representatives of Western medicine and their supporters in our country. Instead of the concept of “dysbiosis”, “bacterial overgrowth syndrome” (SIBO) is popularized in the specialized literature (in English literature - bacterial overgrowth syndrome). However, it reflects a different pathophysiological and clinical situation - the spread of microbial growth into the small intestine (more than 105 microorganisms per 1 ml of intestinal contents in adults and more than 104 per 1 ml in children), i.e., not a qualitative, but a quantitative shift in the microcenosis. ICD-10 does not contain the terms “dysbacteriosis”, “dysbiosis” and “SIBO”. But in clinical practice they are actively used.
2. Can dysbiosis and SIBO be called independent diseases? Do they require treatment?
SIBO and dysbiosis are secondary syndromes that accompany many pathological processes. An imbalance of intestinal microflora is observed in irritable bowel syndrome, traveler's diarrhea, antibiotic-associated diarrhea, inflammatory bowel disease and other pathologies. However, this does not mean that SIBO and dysbiosis should not be diagnosed and treated. Disorders of intestinal microbiocenosis and an increase in the number of opportunistic and pathogenic intestinal microflora (Staphylococcus aureus, enteropathogenic Escherichia coli, Enterobacter, Proteus, Klebsiella, Pseudomonas aeruginosa, Shigella, Campylobacter, Clostridia, Candida, etc.) require therapy, because they cause and support local inflammation, are accompanied by intoxication and can lead to the development of sepsis. For subcompensated and decompensated intestinal dysbiosis, treatment is mandatory.
3. What are the causes of problems with intestinal microflora?
Dysbiosis develops as a result of infectious diseases and post-infectious conditions; after antibiotic, hormonal and polychemotherapy, the use of laxatives and sorbents; surgical removal of part of the intestine. Excessive, unbalanced and disordered nutrition play a role; deficiency of dietary fiber in the diet; consumption of products with an abundance of preservatives, dyes, xenobiotics; radiation damage to the intestines; Colon hydrotherapy. SIBO appears in hypo- and anacid conditions of the stomach; lactase and disaccharidase deficiency, celiac disease; chronic pancreatitis and cholecystitis, inflammatory diseases of the small intestine (Crohn's disease, Whipple's disease, vasculitis); neuropathies and myopathies; intestinal tumors and chronic constipation.
4. How to diagnose microbiocenosis disorders?
Since more than 500 species of bacteria live in the intestines (their total mass can reach 2.5 kg), it is not easy to determine violations of the quantitative and qualitative composition of microflora. The following methods are used: classical bacteriological analysis of feces (culture for dysbiosis) with determination of the main types of microorganisms; culture of intestinal contents obtained endoscopically on bacterial media (to determine SIBO); breath test with lactulose, xylose, labeled with the 14C carbon isotope; bacteriological examination of feces by PCR, FISH method, study of microbial metabolites (indican, phenol, paracresol, ammonia, etc.); gas chromatography-mass spectrometry of the generic composition of microorganisms, which allows you to detect living and dead microorganisms and find out their concentrations.+
5. How does dysbiosis manifest itself?
Symptoms are nonspecific; can be observed in diseases of the gastrointestinal tract that are not accompanied by a violation of microbiocenosis. The main symptoms are dyspeptic syndrome (belching, unpleasant taste in the mouth, increased gas formation, bloating, rumbling, diarrhea, pain and itching in the anus), maldigestion syndrome (impaired digestion and absorption of fats, meat, carbohydrates), abdominal pain, allergic reactions (bloating, loose foamy stools, itching, urticaria, Quincke's edema, bronchospasm, polyarthralgia). The presence of internal intoxication is very typical: weakness, fatigue, lack of appetite, headaches, fever. With a long course, malabsorption syndrome develops, manifested by multivitamin deficiency, weight loss, and anemia. During the day, several liters of gas are formed in the digestive tract, which is mainly absorbed by the intestinal wall. About 600 ml is excreted daily through the rectum, and with excessive bacterial growth, its amount increases to 2 liters or more.+
6. What treatment is needed for SIBO and dysbiosis?
Indications for the destruction of microbial contamination (decontamination) are SIBO and the presence of high titers of opportunistic microflora, which pose a threat of transfer of microbes to the small intestine. For this purpose, several groups of drugs are used: +
- antibacterial drugs;
- non-pathogenic fungi;
- preparations of spore-forming transient flora;
- microbial metabolites.
Antibiotics should not be absorbed from the intestines and suppress the growth of normal microflora. Rifaximin, a local intestinal antiseptic that is well tolerated and does not cause bacterial resistance, meets these requirements. The drug has a wide spectrum of action against opportunistic and pathogenic gram-positive (streptococci, staphylococci, enterococcus, tuberculosis bacillus), gram-negative (shigella, salmonella, yersinia, proteus, E. coli, peptostreptococcus, vibrio cholerae), aerobic bacteria, as well as anaerobic gram-positive ( clostridia, peptococcus) and gram-negative (bacteroides, Helicobacter pylorus). This drug is successfully used for the treatment of acute intestinal infections, correction of SIBO, sanitation of the colon in case of dysbacteriosis and hepatic encephalopathy. Rifaximin is used for a week at 400 mg 3 times a day. At the same time, the level of exhaled hydrogen decreases by 3–5 times already by the third day of therapy, which indicates rapid sanitation of the small intestine.
You can also use other antibacterial drugs: derivatives of hydroxyquinols (Intetrix), nitrofurans (nifuroxazide, or stopdiar), nitroimidazoles (metronidazole, tinidazole), enterofuril. Metronidazole and tinidazole are indicated for contamination with anaerobic microorganisms. Intetrix and nifuroxazide have an antimicrobial effect against Shigella, Salmonella, Yersinia, Campylobacter, Proteus, Klebsiella, pathogenic cocci, and Intetrix also inhibits the growth of fungi and amoebae. The duration of therapy for SIBO is 12–14 days.
An effective treatment for SIBO is enterol, which is a non-pathogenic yeast fungus of the genus Saccharomyces boulardii, obtained from tropical plants and fruits and possessing genetically determined resistance to almost all groups of antimicrobial drugs. The antimicrobial effect of enterol has been established in relation to a wide range of opportunistic microorganisms and protozoa. At the same time, enterol does not suppress the growth of obligate microorganisms in the intestinal cavity. These mushrooms have an antiviral and trophic effect (synthesize polyamines) and 2–5 days after the end of administration they are completely eliminated from the body without side effects. Enterol is used as an antidiarrheal and antiseptic for acute intestinal infections (as an alternative to antibiotics when their use is impossible), antibiotic-associated diarrhea, pseudomembranous colitis, parasitic diarrhea, dysbiosis, SIBO.
In case of grade IV colonic dysbiosis and the ineffectiveness of intestinal antiseptics, general resorptive antibiotics are needed, preferably fluoroquinolones (ofloxacin, ciprofloxacin, norfloxacin, pefloxacin); for pseudomembranous colitis - vancomycin, metronidazole, enterol, bacitracin.
Indications for antibiotics: microbial contamination of the small intestine; generalized form of dysbacteriosis; severe intoxication syndrome; persistent diarrhea syndrome; severe immunodeficiency.
The use of bacteriophages for intestinal dysbiosis has not lived up to the hopes placed on them: it provokes bacterial mutations.
To relieve symptoms of dysbiosis, regulators of intestinal motility (debridat, meteospasmil, motilium, dicetel, mucofalk, imodium), enterosorbents (smecta, enterosgel, enterodes) are used.
7. What biological drugs are used to treat dysbiosis?
There are several groups of biological agents for the correction of intestinal microflora disorders. Eubiotics, or probiotics, contain living obligate microorganisms; symbiotics - a combination of several types of living organisms; prebiotics - growth stimulators of normal microorganisms; synbiotics - live bacteria; prebiotic complexes - a rational combination of probiotics, prebiotics, sorbents, vitamins, microelements.
8. How do probiotics work?
In the broad sense of the word, these are living microorganisms and substances of microbial and other origin that have a beneficial effect on the physiological functions, biochemical and behavioral reactions of the body through the optimization of its microecological status. There are 4 generations of probiotics. The 1st includes single-component (colibacterin, bifidumbacterin, lactobacterin), i.e. containing 1 strain of bacteria. 2nd generation drugs (bactisubtil, biosporin, sporobacterin, etc.), based on the use of microorganisms non-specific for humans, are self-eliminating antagonists of pathogenic microflora. 3rd generation drugs include multicomponent probiotics, which contain several symbiotic strains of bacteria of the same type (acylact, acipol, etc.) or different types (linex, bifiform) with a mutually reinforcing effect. The 4th generation includes bifid-containing drugs immobilized on a sorbent (bifidumbacterin forte, probifor). Sorbed bifidobacteria effectively colonize the intestinal mucosa, providing a more pronounced protective effect than unsorbed analogues. The effects of these drugs on the human body: synthesis of nutrients and antioxidants (vitamins C, K, group B, folic acid, short-chain fatty acids, butyrate, nitric oxide); protective function (colonization of the colon mucosa, production of lysozyme, bacteriocins, decreased production of endotoxins, decreased mutagenicity); immunomodulatory (stimulation of macrophages, IgA synthesis, suppression of IgE synthesis, modulation of cytokine response); digestive (breakdown of carbohydrates, fiber, fats, proteins, deconjugation of bile acids); cytoprotective (neutralization of toxic substrates and metabolites, stimulation of regeneration and differentiation of the intestinal epithelium, anticarcinogenic effect of butyrate through the regulation of apoptosis).
9. What are prebiotics?
These are drugs or dietary supplements of non-microbial origin. They are not digested in the intestines, but have a positive effect on the body, stimulating the growth and/or metabolic activity of normal intestinal microflora. Typical representatives of prebiotics are compounds belonging to the class of low molecular weight carbohydrates: disaccharides, oligosaccharides, which are widespread in nature. Prebiotics should not be hydrolyzed by digestive enzymes and should be absorbed in the upper digestive tract. They selectively stimulate 1 species or a specific group of colon microorganisms. Oligosaccharides (soy oligosaccharide, fructooligosaccharides) are used as prebiotics; monosaccharides (xylose); disaccharides (lactulose); polysaccharides (pectins, dextrin, inulin), dietary fiber from herbs (psyllium), cereals (bran, Rekitsen-RD), fruits; peptides (soy, dairy); enzymes (saccharomyces proteases, etc.); amino acids (valine, arginine, glutamic acid); antioxidants (carotenoids, glutathione, vitamins A, C, E, selenium salts); unsaturated fatty acids; organic acids (acetic, propionic, citric); other substances (lecithin, para-aminobenzoic acid, lactoferrin, lectins, algae extracts, plant and microbial extracts). Prebiotics are best used in the initial stages of dysbiosis, as well as for its prevention.
10. Is herbal medicine prescribed for dysbiosis?
Treatment with medicinal herbs can become a preventive and auxiliary method of correction. The most famous plants that have an antibacterial effect against certain pathogenic microorganisms: apricot - suppresses putrefactive microorganisms, Proteus, Klebsiella, Pseudomonas aeruginosa; barberry (berberine) - hemolytic staphylococci, streptococci, dysentery bacteria, enterobacter; lingonberry (juice) - candida growth; strawberries - Staphylococcus aureus, Enterobacter; cranberries (berries) - putrefactive bacteria of the genus Proteus and Klebsiella; black currant - mushrooms and Staphylococcus aureus, influenza viruses; blueberries - staphylococcus, shigella; rosehip - gram-positive bacteria; apples - pathogenic E. coli, influenza A viruses. Their therapeutic effect is not strong and is observed only after prolonged exposure. Depending on the form and severity of dysbiosis, patients with disorders of the intestinal microflora can be recommended for home treatment for: staphylococcal dysbiosis - eucalyptus, St. John's wort, calamus, calendula, barberry, coltsfoot, Icelandic moss. The diet should include blueberries, rowan berries, strawberries, and raspberries; garlic, horseradish; mycotic candidal dysbacteriosis - linden, thyme, birch buds, eucalyptus, mint, lemon balm, fennel, sage, calamus, Icelandic moss, valerian, speedwell, elecampane, bergenia. You should eat lingonberries, carrots, wild garlic; yeast, potato, pumpkin and rice extracts; putrefactive dysbacteriosis - nettle, lingonberry, caraway, currants, cinquefoil, bergenia, birch buds, celandine, wormwood, maquea, burdock. Apricots, currants, rowan berries, lingonberries are shown; Jerusalem artichoke, red sweet pepper; Proteus dysbacteriosis - eucalyptus, calendula, calamus, plantain, St. John's wort, alder, bergenia, wormwood, cinquefoil erecta. Cranberries, raspberries, currants, peppers, garlic, and onions are useful.
There are 3 degrees of microbiocenosis disturbances.
Easy. The amount of bifid flora is reduced slightly, anaerobes predominate over aerobes, opportunistic flora is represented by no more than 2 species in titers up to 106. Average. The number of aerobes increases. The bifid flora titer decreases. The number of anaerobes and aerobes is approximately the same. Atypical forms of E. coli appear, and the titer of opportunistic microorganisms increases. Heavy. The number of aerobes exceeds the number of anaerobes. The titer of bifidobacteria and lactobacilli is sharply reduced. The number of opportunistic flora has increased - 107 and higher. Patients complain of stool upset, flatulence; there are signs of intoxication: fever, weakness, fatigue.
Anatoly Bliznyuk, Associate Professor of the Department of Polyclinic Therapy of BSMU, Candidate of Medical Sciences Medical Bulletin , June 25, 2014
Share
Types of dysbacteriosis
The following types of dysfunction are distinguished:
- chronic dysbacteriosis;
- acute dysbacteriosis;
The acute variety occurs in most cases and is considered the most common. With timely diagnosis and treatment, unpleasant symptoms disappear within a few days after the start of treatment therapy.
The chronic type of dysbiosis is diagnosed much less frequently. Dysfunction manifests itself if the acute type was not diagnosed and treated on time. Also, the acute stage becomes chronic if the patient abuses alcohol or leads an unhealthy lifestyle.
Dysbacteriosis is divided according to the type of pathogen. Highlight:
- proteaceae,
- staphylococcal,
- associative,
- and fungal species.
The easiest way to cure Proteus dysbiosis. Associative dysfunction is considered dangerous; the period of treatment and rehabilitation is long.
To determine the type of dysbiosis, it is worth visiting a medical specialist. In the private proctology clinic “Proctologist 81”, diagnostic studies are carried out using modern equipment.
What else is prescribed with this study?
Adenovirus (diarrhea syndrome), antigen test
157.0. Feces 2 days
1,000 ₽ Add to cart
Determination of pathogen sensitivity to antibacterial drugs (DDM)
01. 1 day
490 ₽ Add to cart
Determination of pathogen sensitivity to bacteriophages
03. 1 day
220 ₽ Add to cart
Determination of pathogen sensitivity to an expanded range of antibacterial drugs
02. 2 days
600 ₽ Add to cart
Determination of pathogen sensitivity to an expanded range of antibacterial drugs, with determination of the minimum inhibitory concentration (MIC, MIC)
13. 2 days
960 ₽ Add to cart
Stages of dysbiosis
Intestinal dysfunction has several stages. Depending on the stage, the patient is prescribed treatment. The following stages of development of intestinal dysbiosis are distinguished:
| Dysbacteriosis of the first degree | At the initial stage, the amount of E. coli, namely Escherichia, decreases in the human body. There are no symptoms, no deficiency of lactobacilli is observed. |
| Dysbacteriosis of the second degree | The number of Escherichia in the body is rapidly decreasing. A deficiency of bifidobacteria and other beneficial microorganisms that are responsible for metabolism and the digestive process is diagnosed. The number of pathogenic bacteria increases. |
| Dysbacteriosis of the third degree | There is a severe shortage of bifidobacteria and lactobacilli. The patient feels a lot of discomfort and problems with bowel movements appear. Intestinal function is disrupted, microflora and peristalsis are disrupted. |
| Dysbacteriosis of the fourth degree | Bifidoflora in the intestines is in a terrible state. Lactobacilli are completely absent. Dangerous destructive processes occur in the intestines, peristalsis is completely disrupted. |
To avoid complications and negative consequences, treatment should be started at the initial stage.
Drugs and their action
The most effective way to restore microflora and get rid of dysbiosis is to use drugs from the group of probiotics. Manufacturers offer medicines in different forms:
- capsules;
- pills;
- powder;
- drops;
- solution.
The dosage form is selected by the doctor depending on the age of the patient. Children and elderly people who have difficulty swallowing tablets are prescribed a solution or powder for its preparation. At the age of 0-3 years, it is easier to give probiotic drops to a child. For everyone else, capsules or tablets are recommended.
Anti-dysbacteriosis medications are medications that can be purchased without a doctor's prescription. But self-medication is not recommended; only a specialist can tell you which type is best to take.
Probiotics usually contain 1-2 types of bacteria that restore mucous membranes well. Usually these are lacto- and bifidobacteria. They are normal inhabitants of the intestines that help improve microbial balance. The mechanism of action of this therapeutic group is associated with suppression of the growth of pathogenic flora. Lactic acid bacteria compete for receptors on the mucosal epithelium and nutrients. They secrete lactic acid and cytokines, which have an inhibitory effect on pathogens.
Preparations from the group of prebiotics help to effectively cure dysbiosis. These are medications that belong to the group of dietary fibers: inulin and lactulose, as well as drugs based on them.
They are not broken down by digestive enzymes and enter unchanged into the large intestine, where they become a nutrient substrate for lacto- and bifidobacteria. Therefore, microbes multiply well, increase the volume of bacterial mass, and restore the intestinal wall. To make the treatment as effective as possible, it is recommended to take prebiotics and probiotics at the same time.
Treatment of dysbiosis is not contraindicated in case of concomitant pathologies of the digestive tract. Probiotics are not harmful to patients with stomach ulcers, liver disease, or gallbladder disease. And in some cases they will speed up recovery.
In advanced cases of intestinal dysbiosis and when the symptoms of dyspepsia are too painful, medications from the group of enzymes can help. They should be selected by a doctor, depending on the type of digestive disorder. These medications must be taken daily before meals.
It’s hard to say how long it will take to treat dysbacteriosis. In some cases, this can last for several weeks, and in advanced cases – several months.
Signs of intestinal dysbiosis in an adult
At the second stage, symptoms appear that indicate intestinal dysbiosis. There are no specific symptoms, so patients often confuse intestinal dysfunction with other pathologies.
- bad breath;
Putrefactive processes occur in the body. These processes are caused by the accumulation of harmful components in the intestinal tract.
- gastrointestinal disorders;
The patient is worried about diarrhea. The walls of the anus are injured, the mucous membrane is irritated, which leads to the formation of anal fissures. Diarrhea occurs up to ten times a day, regardless of food intake. Often, stool has a foamy structure in appearance.
Constipation is also observed with dysbacteriosis, but much less frequently. Fecal masses collect in the intestines, so the patient develops colicky pain and the stomach swells. Constipation is observed in older people whose peristalsis is noticeably impaired.
- bowel dysfunction;
The stool is disrupted, with constipation alternating with diarrhea. Bloody impurities, mucus and even pus are found in the stool. This symptom indicates an inflammatory or infectious process. The color of the stool becomes greenish. After eating, rumbling appears in the stomach. We are talking about problems in the intestines. Flatulence increases. Excessive gas formation brings discomfort to the patient. Belching is observed.
- painful sensations;
Pain appears in the intestines. Unpleasant sensations intensify with constipation and pushing. Nausea and vomiting, itching and burning in the anus, and heartburn appear. With dysbacteriosis, food is slowly absorbed, so the patient rapidly loses weight and becomes constantly tired and sleepy. The patient becomes tense and nervous.
It is extremely rare for the temperature to rise to 38 degrees. The symptom indicates severe intoxication of the body. After eating food, an allergic reaction occurs, a skin rash and itching appears.
- avitaminosis.
The condition of bones, hair and nails deteriorates. Skin color becomes pale.
Causes
The intestinal microflora in adults is in a state of dynamic equilibrium. It contains certain bacteria, which make up the majority, and about 3% of microorganisms that change their composition. Normally, fluctuations occur under the influence of food and eating habits. The microflora is affected by the predominance of sweets and fatty foods in the diet or predominantly plant foods.
Research shows that fatty foods inhibit bifidobacteria and enterococci, but under these conditions bacteroides multiply. A predominantly carbohydrate diet stimulates the proliferation of bifidobacteria and the total number of microorganisms. But these changes are temporary and do not lead to the appearance of symptoms of dysbiosis. They disappear on their own after a change in diet.
Intestinal dysbiosis in adults appears as a result of other diseases. The main causes of microflora disturbance are:
- long-term treatment with antibiotics;
- pathologies of the overlying parts of the digestive tract;
- long-term mono-diets and constant poor nutrition;
- intestinal infections.
Broad-spectrum antibiotics act nonselectively. They inhibit the growth or cause the death of all microorganisms. The longer the course of treatment, the higher the likelihood that dysbiosis will develop after it. Tetracycline antibiotics are especially dangerous. They significantly inhibit the proliferation of intestinal microflora, which leads to hypovitaminosis B, K, and an increased risk of bleeding.
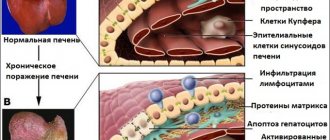
Gastritis, cholecystitis, pancreatitis, hepatitis or biliary dyskinesia can lead to the development of dysbiosis. Cirrhosis of the liver, tumor processes in the stomach or ulcers are dangerous. These pathologies are accompanied by impaired digestion of food and enzyme production. Therefore, food enters the intestines insufficiently processed and cannot serve as a breeding ground for bacteria. Some of them die, and a seemingly pathogenic flora takes their place.
A fasting day, when the diet is based on the consumption of one food product, does not harm the body. But a mono-diet that lasts several weeks or becomes a way of life can lead to dysbiosis. Constant consumption of food containing simple carbohydrates and animal fats is dangerous. These are sweet, flour, fast food dishes. Such a diet inhibits the reproduction of normal flora, fermentation processes are activated in the intestines, and a large number of yeast fungi appear.
Food infections cause double damage to the intestines. They damage the mucous membrane, and antibiotic treatment kills beneficial bacteria. Therefore, recovery from illness is especially difficult.
Smoking has a negative effect on the condition of the intestines. It creates conditions for the proliferation of yeast, so smokers often suffer from unpleasant symptoms.
Symptoms of intestinal dysbiosis in women
Signs of intestinal dysbiosis in women are accompanied by abdominal pain before defecation. There is increased activity of the sebaceous glands, and acne appears on the face and body. Particularly painful sensations intensify before menstruation .
The mucous membrane of the nasopharynx and vagina becomes irritated, and rashes appear on it. The patient is bothered by itching and burning. Cardiac symptoms appear. Such signs include headache, dizziness, tachycardia, surges in blood pressure and even fainting.
Dysbacteriosis in women is always accompanied by deterioration of the skin. It becomes dehydrated, dry, loses firmness and elasticity.
Vaginal dysbiosis and pregnancy
Pregnancy is one of the factors that can provoke an exacerbation of vaginal dysbiosis. During pregnancy, discharge, itching or burning in the genitals, pain during intercourse, etc. may appear or intensify. This is due to the fact that during pregnancy a woman’s body undergoes serious hormonal changes, which cannot but affect both the immune system and the vaginal microflora.
Complete treatment of vaginal dysbiosis during pregnancy is not possible. Even if this treatment is not associated with taking antibiotics, which is extremely undesirable during pregnancy, it is always associated with immunocorrection, and this is completely unacceptable during pregnancy. Therefore, the doctor’s task during an exacerbation of vaginal dysbiosis in a pregnant woman is only to eliminate the symptoms and prepare the woman for childbirth.
In our clinic, for this purpose, a course of procedures is carried out that, if not normalize the situation, then make it more tolerable. Local treatment carried out in this case is completely harmless to the fetus. If necessary, this treatment can be carried out repeatedly throughout pregnancy.
Diagnosis of intestinal dysbiosis
If symptoms appear, you should contact a gastroenterologist or proctologist . The healthcare professional will conduct a survey to learn about the patient's complaints and symptoms. After collecting anamnesis, the attending physician examines the patient’s chart, learns about previous diseases, and about the surgical intervention that was performed previously.
Next, an examination with palpation is carried out to determine the condition of the large intestine. After this, the patient is sent for a general blood, stool, and urine test. A bacteriological analysis of stool is required. This is the only way to determine whether there is dysfunction in the body.
A few days before diagnostic tests, it is worth excluding fermented milk products, fermentable vegetables, taking antibiotics, kvass, and drinking alcoholic beverages from the diet. Beer is strictly prohibited. The patient is referred for a comprehensive examination of the abdominal organs.
Ultrasound diagnostics , X-ray examination using contrast fluid, computed tomography, magnetic resonance imaging are performed. Research is carried out only if there are no contraindications.
Restoration of intestinal microflora
If you notice any signs of dysbiosis, it is recommended to immediately consult a gastroenterologist.
The basis of treatment is to eliminate the cause that caused the disruption of intestinal microflora. If dysbiosis is caused by antibiotics, their use must be stopped, and if due to the wrong regimen or diet, you need to return to the original diet. However, the symptoms of dysbiosis themselves also need treatment. For dysbiosis, 3 types of treatment are recommended:
- Diet;
- Prebiotics;
- Probiotics.
Treatment of intestinal dysbiosis
With intestinal dysfunction, it is extremely important not only to eliminate the symptoms, but also to eliminate the source of the pathology. Medical experts are trying to:
- stop the growth of pathogenic microorganisms;
- stimulate the proliferation of beneficial bacteria;
- boost immunity.
It is necessary to change the diet, exclude fried foods, baked goods, and foods that cause fermentation. Vegetables and fruits, cereals and broths should be included in the menu. The diet is prepared by a professional nutritionist to avoid complications. It is strictly forbidden to drink alcoholic beverages or smoke. Treatment is carried out with medications.