About the disease
Acute respiratory viral infection (ARVI) is a large group of pathologies of the upper and middle respiratory tract, which are provoked by pathogenic microorganisms (viruses).
Scientists have identified approximately 200 pathogens that can cause typical clinical signs. This creates difficulties when it comes to accurately verifying the strain of the virus that caused the child’s illness. According to domestic and foreign experts, 3-4 episodes of ARVI per year are the norm for a child. The Americans even make a clarification. They allow an increase in the number of ARVI episodes up to 12 times per year if the child starts going to kindergarten or school. Experts attribute this to a sharp increase in new “acquaintances” with viruses that the baby had not previously been in contact with. Therefore, it is important to understand that you do not always need to panic when the first snot appears in a 3-year-old child who has not been sick before, if he has begun to actively communicate with peers.
Doctors more often use the term “acute respiratory disease (ARI)” than ARVI. This is due to the fact that in order to mention the viral genesis of the disease, this fact must be confirmed in the laboratory. This is often time-consuming and financially disadvantageous for the patient. Therefore, it is easier to indicate the broader term acute respiratory infections, which includes not only bacterial infections, but also viral ones (ARVI). Diagnosis and treatment of children in both cases is carried out according to the same algorithm, which eliminates the risk of reducing the effectiveness of therapy.
Prevention of ARVI in childhood
Children under 5 years old get sick more often than others, so they need increased attention from adults. Not learning what ARVI is in childhood is the same as never being a child. It will not be possible to avoid diseases, but it is possible to minimize the number of infections.
Follow preventive measures to strengthen the immune system and thereby increase the body's resistance to pathogens. They can both overcome the virus and help the child suffer from a mild form of the disease, while his peers with weakened immune systems will experience a full “bouquet” of symptoms.
Preventive measures that strengthen the immune system against colds and acute respiratory viral infections:
- introduce seasonal vegetables and fruits into your diet;
- ventilate the rooms daily and do wet cleaning;
- exercise;
- exclude contacts with sick relatives;
- wash your hands when returning from the street and before eating food;
- limit visits to crowded places;
- maintain the room temperature at 18-22o;
- eat well;
- get vaccinated before the common cold season;
- maintain a sleep-wake schedule;
- walk outside more often.
Every family can implement these simple rules into their lives. If you follow them, you will protect your children from colds.
ARVI symptoms
ARVI is one of the most common pathologies encountered by both children and adults. Every person in the world has encountered this infection at least once in their life. The most typical clinical signs of ARVI in children are:
- increased secretion of mucus from the nose (sometimes it can acquire a yellowish or even greenish tint);
- redness of the sclera;
- tearfulness;
- cough (in the early stages of the disease it is dry, but then becomes productive with coughing up sputum);
- increased body temperature (usual seasonal acute respiratory viral infections are rarely accompanied by a fever of more than 38.5 ° C, however, even such an increase in body temperature can be dangerous for infants and newborns);
- nasal congestion;
- hoarseness of voice.
ARVI should be distinguished from influenza.
The latter is not accompanied by copious nasal discharge, but occurs against the background of severe fever (up to 40°C) and body aches. Most of these symptoms in the early stages are not critically dangerous. But if they are identified, it is worth showing the child to a pediatrician or family doctor to prescribe adequate treatment and prevent the development of serious complications (sinusitis, otitis media, pneumonia).
Vaccination
Many people think that there is nothing better than vaccination - one injection and you can forget about the disease, but in reality everything is far from simple. Vaccination is an effective method, but against a specific virus. It is physically impossible to vaccinate a child against all types of viruses during cold season. Doctors especially recommend vaccination against influenza for children and when epidemic outbreaks are predicted, since influenza has the most severe complications6.
Disadvantages of vaccination:
- Vaccination must be done in advance, even if the onset of the epidemic has not yet been recorded.
- Vaccination can only be given to a completely healthy child, otherwise unpleasant complications are possible.
- The effectiveness of vaccinations is high, but it is not universal. That is, vaccination in general does not help against ARVI.
Causes of ARVI
The cause of ARVI development is viruses.
When they enter the mucous membrane of the upper respiratory tract, pathogens penetrate the cells and disrupt their normal function. This process is accompanied by local inflammation with hyperproduction of mucus, which leads to a runny nose or cough. Factors that increase the risk of infection are:
- child hypothermia;
- too dry air (under conditions of hyperthermia, the protective function of the mucous membrane of the upper respiratory tract decreases and, accordingly, the aggressiveness of pathogens increases);
- congenital or acquired immunodeficiency;
- malnutrition, prematurity;
- abnormalities of the upper respiratory tract;
- exacerbation of chronic somatic diseases.
The source of infection is a sick person. Viruses are transmitted by airborne droplets and through contaminated personal hygiene items.
How to treat a child with ARVI: all the methods for use
In most children, ARVI is not severe, so treatment is carried out on an outpatient basis. It is recommended to hospitalize a child only in exceptional cases, for example, when serious complications occur, the development of toxicosis, convulsive or hyperthermic syndrome.
In 2021, recommendations from the Russian Ministry of Health “Acute respiratory viral infection (ARVI) in children” addressed to pediatricians were published, which detail the treatment method.
All medications for the treatment of ARVI can be divided into two groups - for symptomatic therapy , in other words, used to reduce symptoms, and for etiotropic therapy , that is, those used directly to combat viruses. Any medication for a child should be prescribed only by the attending physician, since the child’s body is especially susceptible to drugs: an incorrectly selected drug, instead of a cure, can lead to deterioration and harm health.
Direct acting antivirals
These include oseltamivir, rimantadine and umifenovir. Medicines based on rimantadine are active only against influenza A. Other types of viruses are highly resistant to this drug. Products for children are produced in the form of syrups and are recommended for use from the age of one year [8].
Oseltamivir is the main modern etiotropic drug, which is highly effective against all strains of influenza A and B known today. But it should be borne in mind that drugs based on oseltamivir are exclusively anti-influenza and do not have an effect on other pathogens of ARVI. Indications for their use can only be cases with a clearly influenza etiology of the disease. Unfortunately, at the moment in Russia there is no special children's form of such drugs, so the suspension has to be made independently, using the contents of the capsule. Oseltamivir is approved for use in children over one year of age[9].
Umifenovir - drugs based on it are active both against various influenza viruses and against other pathogens of acute respiratory viral infections. But these products have age restrictions: suspensions are allowed for children from two years old, and tablets - from three years.
Interferon preparations
Interferon-based drugs are nonspecific antiviral drugs with a broad spectrum of action. Interferons themselves have not only antiviral, but also immunomodulatory and antiproliferative effects in relation to the entire body. This leads to the rapid elimination of foci of inflammation. In addition, interferons can inhibit the ability of viruses to reproduce, and therefore stop the development of the disease. The interferon contained in these products is actively absorbed by the mucous membrane and fixed in the cells, due to which it has a local effect. Part of it also enters the lymphatic and circulatory systems, providing a quick therapeutic result.
However, the choice of medication should be dictated not only by its effectiveness, but also by its safety in accordance with the child’s age. Thus, for very young children - literally from the first days of life - only natural and recombinant interferon preparations are officially allowed. They can be in the form of suppositories: Genferon® light (LSR-005614/09)[10], Viferon® (R N000017/01)[11] and Kipferon® (R N000126/01)[12], as well as in the form nasal agents: drops and spray “Genferon® light” (LP-002309 and LSR-009046/10) [13, 14], drops and spray Grippferon® (P N000089/01 and LP-001503) [15, 16].
Immunomodulators and inducers of interferon production
According to the clinical recommendations of the Ministry of Health of the Russian Federation “Acute respiratory viral infection (ARVI) in children”, prescribing drugs with an immunotropic effect for children with ARVI is inappropriate, since they do not have a proven significant therapeutic effect [17].
In the treatment of ARVI in young children (up to one year), it is possible to use release-active interferon inducers - “Anaferon for children” (LP-N (000019)-(RG-RU) [18] can be used in children from one month.
Homeopathic remedies
These are drugs such as Oscillococcinum® (P N014236/01) [19] and others; they are also not recommended for use in the treatment of ARVI in children due to unproven effectiveness.
As for symptomatic therapy, for example, to combat a runny nose, it is recommended to inject saline solution into the nose two to three times a day, and to alleviate the condition, it is allowed to use vasoconstrictor drugs for a course of no more than five days.
To reduce a child’s temperature, you can wipe him with a sponge or towel moistened with water at a temperature of about 25–30°C. Antipyretics for children older than three months are recommended only if the temperature rises above 39–39.5 ° C, and acetylsalicylic acid (aspirin) should not be used.
Non-drug methods
In addition to taking medications, it is also advisable to follow a few simple recommendations for a speedy recovery.
A sick child should be isolated from other children as soon as possible. This measure will not allow him to become a spreader of the virus, and will also protect the body weakened by the disease from the effects of other possible infections.
- It is necessary to limit the child’s physical activity in order to preserve his strength, so bed rest is necessary.
- The child should be given warm drinks often - this helps remove toxins from the body and reduce the temperature.
- It is recommended to do wet cleaning in the room where the patient is located as often as possible and to ventilate the room.
- It is advisable to rinse the nose - this makes it possible to effectively stop a cough that occurs due to irritation of the larynx by secretions flowing from the nose. Steam and aerosol inhalations for the treatment of ARVI, despite their popularity, do not have the desired effect, and in addition, are not recommended by WHO[20].
- Diet. You should not force your child to eat food against his wishes. Foods high in proteins and vitamins should be included in your diet. Food should be easily digestible and nutritious.
In general, ARVI is a benign disease, but it is also the most common reason for the use of various “fashionable” procedures and means, most often completely unnecessary, and often completely harmful. With the right approach, minimal intervention is sufficient for a quick therapeutic effect. The doctor’s task is to correctly and quickly select the appropriate remedy. Parents must strictly comply with all appointments and instructions, abandoning the idea of treating the child themselves.
Diagnosis of ARVI
The SM-Doctor clinic is an advanced medical institution that operates according to the standards used in leading medical centers in Europe and the world.
This means that the child undergoes only informative examinations and receives treatment that has proven its effectiveness. The diagnosis is based primarily on an assessment of the patient's clinical condition. The doctor analyzes the complaints of the child and his parents, clarifies the medical history, and conducts a physical examination with auscultation of the lungs. To confirm the diagnosis, the pediatrician may also use the following examinations:
- chest x-ray;
- a set of laboratory tests to assess the patient’s general health (blood and urine tests, blood biochemistry);
- microscopic analysis of nasal mucus or sputum.
If necessary, the doctor can additionally refer the baby for a consultation with related specialists (cardiologist, gastroenterologist, pulmonologist).
How do children become infected with ARVI?
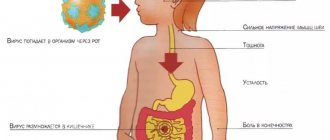
One of the transmission routes is airborne droplets. Infection occurs when a child inhales air containing viruses1. When coughing or sneezing, microscopic viral particles spread from a sick person to a distance of more than 6 meters3 and through the “entry gate” - the nasal cavity and nasopharynx - enter the respiratory tract of a healthy child4.
However, you can also become infected with ARVI through contact and household contact1,5 - through interaction with contaminated surfaces. Children's toys, door handles, elevator buttons, handrails in public transport - these are the places where viruses persist for up to several days6. To “introduce” the virus into the body, it is enough to touch infected objects and then scratch your eyes or nose with dirty hands1.
It is not surprising that
children in kindergarten are more likely to get ARVI than children who did not attend kindergarten, because here they use shared toys and spend time indoors. But kids who “missed” nursery and kindergarten usually get sick more often as soon as they start going to school 1 .
Up to contents
Treatment of ARVI
ARVI, which occurs without complications, is not a serious problem for an experienced doctor. According to modern recommendations, the following key aspects can be identified in the treatment of seasonal colds:
- Bed rest. Peace for a child is a hall for the rapid restoration of lost strength.
- Drink plenty of fluids. Preference should be given to breast milk (children under 1-2 years old), warm tea, and fruit drinks. The liquid helps remove toxins from the child’s body.
- Complete nutrition. A sufficient supply of protein, vitamins and minerals promotes rapid recovery and complete tissue restoration.
- Taking antipyretic medications (paracetamol, ibuprofen) when body temperature rises above 38.5°C.
If complications develop, the doctor may additionally prescribe antibiotics, vasoconstrictors, and antihistamines.
It all depends on the characteristics of a particular clinical case. “SM-Doctor” is a clinic where pediatricians with over 10 years of experience effectively treat children with any form of ARVI. Our specialists have their own laboratory and access to modern equipment. All this guarantees the highest quality of services provided and improvement of the patient’s well-being in a short time. Contact qualified specialists!
General recommendations
Quite often, doctors give recommendations that help maintain the immune system in working order and help the child survive the cold season6:
- More fresh air;
- Hardening, but not during illness, otherwise complications are possible;
- Physical activity;
- Careful hygiene, especially during periods of illness;
- Maintaining a healthy weight;
- Increasing air humidity in the room where the child is;
- Drinking plenty of water.
Eating healthy foods is always an important and logical factor in resisting colds. Fresh vegetables and fruits (especially citrus fruits) are healthy in themselves; also, during colds, doctors advise eating garlic, berries (cranberries, raspberries and lingonberries), fruit drinks, compotes and herbal decoctions. The main thing is to know when to stop and not to overuse certain types of foods in order to avoid allergic reactions or problems with the gastrointestinal tract.6.
General preventive recommendations may not be enough, in which case drug support is required. Imudon® can act as an effective drug. The medicine has a high degree of safety and is available in a convenient form of lozenges, so it can be easily given to children aged three years and older. The drug helps strengthen the immune system in the throat during periods of increased respiratory disease. When prescribed in complex therapy together with other medications, Imudon® helps speed up the healing process and eliminate sore throat, as well as prevent complications7,8.
Contraindications
There are contraindications for the flu shot:
- age up to six months;
- presence of allergies to the components of the drug;
- severe reaction to a previous vaccination.
Children who have:
- egg allergy;
- dysfunction of the immune system.
In any case, before vaccination, you must be examined by a doctor and undergo tests. Two weeks before the vaccination date, it is advisable to avoid traveling. If you are prone to allergies, you should start giving antihistamines three days before the procedure. If a child falls ill within three weeks before vaccination, it is recommended to postpone the vaccination date to a later date.
Complications of flu and colds
Not only the viruses themselves are dangerous, but also the toxic products of their vital activity. Among the most common and unfavorable consequences of ARVI are inflammations of the sinuses, ears, throat, larynx, bronchi and lungs. Parents need to pay special attention to fever. Prolonged and uncontrollable fever with numbers greater than 38.5 degrees Celsius requires immediate intervention. At lower temperatures the body fights on its own, but at higher temperatures it needs help. To reduce the temperature, you can use antipyretics, but strictly under the supervision of a doctor. Today you can find a lot of recipes in popular literature that supposedly quickly and reliably relieve fever from viral infections. But it is extremely dangerous to trust such recommendations. For example, the most common misconception is that antibiotics reduce fever. But for viral diseases, these drugs will not have an effect, since they only destroy bacteria and do not affect viruses. Antibacterial agents are prescribed only when complications develop.