Saturation (English saturation - “saturation”) of blood with oxygen shows how much of this vital gas for organs is currently contained and circulating in the blood. The indicator is expressed as a percentage. Low saturation, including during coronavirus, indicates hypoxemia, which requires urgent action. It is necessary to increase the level of oxygen in the lungs and blood to prevent complications and sometimes to save the patient's life.
Blood oxygen saturation is measured with a special device - a pulse oximeter. With the help of this express analysis, emergency doctors can obtain objective information about the state of the patient’s respiratory and circulatory system, as well as quickly make a decision on hospitalization and oxygen support. It is not always possible to quickly perform a CT scan of the lungs. If a patient’s saturation is clearly reduced during COVID-19, this most likely indicates a viral infection of the lungs—pneumonia.
Measuring blood oxygen saturation with a pulse oximeter device allows emergency teams to identify seriously ill patients with likely extensive lung damage caused by COVID-19, and also quickly make decisions about hospitalization and the necessary additional oxygen support.
If a patient with coronavirus has such a device at home, then he can carry out monitoring on his own, however, it is important to understand that pulse oximetry (measurement of saturation) does not replace a visual assessment of the condition of the lungs (CT of the lungs), and an incorrect interpretation of this indicator can only frighten the patient and mislead ambulance or cost the patient his life.
A patient with a new coronavirus infection and doctors should not focus solely on the saturation indicator - the measurement result highly depends on a number of third-party factors: the sensitivity of the device, lighting, and the color of the patient’s skin. Meanwhile, if you rely on this indicator as the main one (without spirometry and CT), there is a high probability of an inadequate assessment of a person’s health - in severe pneumonia, the saturation may remain normal for some time, and then drop sharply. At night, saturation decreases even in a healthy person.
In this material we will examine the main issues related to saturation during coronavirus.
What is saturation?
Saturation is an indicator of the saturation of blood with oxygen, which comes from the pulmonary alveoli. Together with blood, oxygen is transported to organs and tissues. A decrease in saturation during COVID-19 indicates hypoxemia, the likely cause of which is viral infection of the lungs. The hypothesis can be confirmed or refuted by computed tomography - during a visual assessment of the lungs.
How coronavirus kills lungs
Coronavirus primarily affects the lower respiratory tract. This is why it is important to constantly monitor saturation during COVID-19. The same thing happens with viral pneumonia. These diseases are characterized by a rapid onset and a sharp onset of respiratory failure. Large areas of the lungs are affected at once.
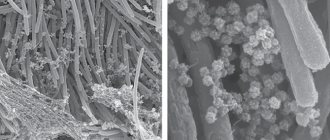
The coronavirus is like a spiked ball. With them, it binds to a certain protein in our body called angiotensin-converting enzyme 2 (ACE2). There is a lot of it in blood serum, as well as in the epithelial tissue of the kidneys. But most of the cells that have this enzyme are located in the lungs; the alveoli are literally lined with them.
Once the virus enters the cells of the alveoli, it begins to multiply rapidly, forming tens of thousands of “clones” that exit the cell, destroying it. In place of the dead cells of the lung tissue, connective tissue is formed that is not capable of breathing, so-called pneumosclerosis occurs.
Coronavirus. Pandemic. COVID-19.
CC0
What is the normal saturation level for a healthy person?
The norm for a healthy person is SpO2 = 95-99 (or 100)%. The rate of blood oxygen saturation depends on the individual characteristics of the human body, for example, on the presence or absence of anemia, apnea, chronic diseases of the respiratory and cardiovascular systems, bad habits, and age. At night, each person's saturation decreases, and the differences can be significant. For example, in people with chronic diseases of the respiratory system (COPD, apnea), who have adapted to a constant lack of oxygen, the rate can drop to 90% (in the deep sleep phase).*
According to the observations of doctors working in hospitals with seriously ill patients who are on oxygen, the most dangerous time is from 3 to 7 am. At this time, the largest number of deaths are recorded due to decreased saturation, or more precisely due to oxygen hypoxemia.
RE Gries, LJ Brooks, Normal oxyhemoglobin saturation during sleep. How low does it go? K. Szabó, F. Ihász, The effect of reduced oxygen saturation during sleep on depression, 2020
Why does saturation decrease during coronavirus?
Not all patients with COVID-19 have a decrease in saturation, but only with the development of a complication - viral pneumonia. A decrease in saturation indicates probable respiratory failure. If a coronavirus infection has penetrated the lung tissue, and a person’s immune system cannot cope with it, a destructive process begins in the lungs - the alveolar septa (and interstitium) are damaged and inflamed, and the alveoli themselves are filled with liquid exudate - normally they are filled with air and are the starting point of transportation oxygen to organs, including the heart and brain. Since there is no damage to the bronchial tree with coronavirus, a decrease in saturation in a patient may indicate a reduction in the functional areas of the lung tissue.
If coronavirus saturation is below 95%, the patient may be hospitalized.
UPD: inexpensive pulse oximeters
DEAR READERS, FOR THE COOLEST SALE FROM ALIEXPRESS ON 11.11.2021 WE HAVE PREPARED A PROMOTION FOR THE BEST CHEAP PULSE OXIMETERS. Just click on this ad
Perhaps the devices listed above seemed a little expensive to you, then we offer you a cheaper alternative. Please note that this is a purchase at your own risk. Here are some interesting options.
Pulse Oximeter
A miracle of Chinese production, which is actively sold on Aliexpress for 500 rubles ($6.5), and in domestic online stores - from 900 rubles (almost $12). We can’t find any information about the brand or the model name, so for us it will remain just Pulse Oximeter. It shows pulse, saturation and pulse wave, turns off after 8 seconds of inactivity. There is a sound indication for low saturation and arrhythmia. Powered by two AAA batteries, not included, but the product comes with a strap. This is surprising, but hundreds of reviews say that the device does its job well and gives accurate measurements if all instructions are followed.
You can find it on the sites due to its low price and appearance. It is almost exactly the same as the CONTEC CMS 50D we mentioned above, only it comes in a different box without the brand name. It turns out that this is a Chinese replica, since even on Aliexpress the CONTEC CMS 50D costs at least 2,300 rubles ($30). Cheap and cheerful. If you decide to, you can buy it here.
Attention to the packaging and its difference from CONTEC CMS 50D
ARSTN Oximeter M170A
Another example of a popular device from Aliexpress. If you believe the reviews, this pulse oximeter is quite functional and, most importantly, accurate. Users note that they checked the readings with devices in clinics, and the result was the same. This model has several brightness levels, sound notification, and collects statistics. It is powered by two batteries and comes with a solid case. Cost – 1080 rubles (about $14).
You can view the model here. The page also presents other models of the manufacturer; there are also cheaper ones, without sound alerts and with an LED screen. Judging by the reviews, all are accurate, but be careful when purchasing - do not confuse the models.
YK-82C
Nice device with a bright display. The user is given the opportunity to assign the minimum and maximum permissible values of heart rate and saturation, and outside this range, sound and light indications will be triggered. There are several information output modes. The kit includes a case and lanyard, no batteries. The reviews are very good. Price – 800 rubles (a little more than $10). You can order here.
Why measure saturation during coronavirus?
Coronavirus saturation is measured to quickly detect life-threatening hypoxemia. In this way, the severity of the disease is determined and a decision is made on further actions: hospitalization, oxygen support, computed tomography.
In foreign literature there is the term “silent hypoxemia”, which appeared only recently, during the COVID-19 pandemic, when it became clear that a fairly large percentage of patients were admitted to the hospital with an acute lack of oxygen, disproportionate to the symptoms. It turns out that patients can breathe, do not choke, there is no strong cough and no fever, while the lungs are severely damaged, saturation is critically low, and additional oxygen is needed.
Can a patient with symptoms of coronavirus somehow suspect that he has a lack of oxygen due to pneumonia? Yes.
What to do with low saturation
At critical levels, life-sustaining drugs and equipment should be used. This is done by the medical staff.
If it is low, it is recommended to do the following:
- breathe fresh and clean air, do breathing exercises;
- drink water in small sips and take blood thinning medications (as prescribed by your doctor);
- consume foods high in iron (buckwheat, meat, apples).
Regular breathing training, combined with physical exercise, will strengthen the body and make it easier to endure any disease due to the improved function of oxygen supply to all tissues in need.
Symptoms of decreased saturation
- Try holding your breath for a few seconds - if you can't help but breathe as long as before, and this action is causing difficulty, it makes sense to measure your saturation.
- Your breathing and heart rate have increased.
- The skin turned pale and acquired a bluish tint (face, lips, fingertips).
- You feel very tired and sleepy.
- My head hurts and feels dizzy, I have problems with memory and concentration.
- You are experiencing some symptoms of a respiratory system disease: shortness of breath, discomfort and unusual sensations in the chest, coughing.
What to do if saturation drops?
Don't panic about low saturation - normal vital signs can be quickly restored, and even a reading of 70% within a few days is compatible with life, and the chances may be even higher if the patient has, for example, chronic obstructive pulmonary disease, and to a low level oxygen, his body has already adapted. Saturation may drop for several days.
However, if during coronavirus the saturation drops to 95%, 93, 90...%, and all measurements are made correctly (it is important to check that the pulse oximeter has an adequate battery level, and that the device itself is registered as a medical device and not purchased from dubious manufacturer) - you need to call an ambulance.
Why do you need to measure oxygen levels?
The level of oxygen in the blood is important for the doctor, among other indicators of the patient’s condition, in order to provide timely assistance with breathing and prevent oxygen starvation of organs and tissues.
Pandemic. Kiss.
CC0
Signs of hypoxia - oxygen deficiency - may include:
- weakness and fatigue;
- increased sleepiness (mainly during the day);
- headache;
- memory impairment;
- periodic dizziness;
- decreased concentration;
- tachycardia, increased cardiac output;
- decreased blood pressure;
- pale skin;
- swelling of the lower extremities (a sign of heart failure).
In addition to coronavirus patients, measuring oxygen levels is important for people suffering from COPD, chronic obstructive pulmonary disease, which is characterized by chronic restriction of air flow in the airways.
COPD symptoms get worse over time. Shortness of breath during exercise gradually turns into shortness of breath at rest. This disease is often undiagnosed and can be life-threatening. In the past, COPD was often referred to by the terms “chronic bronchitis” and “emphysema.”
Coronavirus. Pandemic. Analyzes.
CC0
Why can pulse oximetry data be misleading?
It is important to understand that the result of pulse oximetry can be influenced by: the sensitivity of the device (including battery charge), lighting, and the color of the patient’s skin (the darker, the higher the indicator, which does not reflect the real state of affairs).
The concept of “saturation rate” is very arbitrary. It happens that patients with signs of coronavirus infection and a mobile non-invasive device for measuring saturation begin to panic and call an ambulance if the oxygen in the blood drops, for example, to 93%. To do this, let’s look at the data from the conditional norm table:
Details for instructions for use
Each pulse oximeter package contains the necessary documentation, including instructions for use. It is not difficult to understand, since the device is compact and simple. Most home pulse oximeters run on AA batteries or rechargeable batteries. To use the device, you must insert the batteries and wait a few minutes. Then you should pay attention to the device's charge level - if it is low, the readings may not be accurate enough. Next, you just need to follow a few simple steps yourself or with an assistant.
- The first step is to take a stationary position, sitting or lying down, with your arm supported. It is recommended to remain in this position for several minutes before measuring to obtain more accurate readings.
- The second step is to place your finger in the special hole of the pulse oximeter. It must be clean and free of nail polish and other coatings that could affect the measurement result. The sensor will operate for 20–30 seconds, depending on the model of the device, and during this time the finger must remain motionless.
- When the results are displayed on the monitor, the measurements are completed. It is recommended to record the data in order to keep a constant record of heart rate and saturation levels. After this, the pulse oximeter should be turned off and placed in a box to keep it away from sunlight and dust.
The device can be used independently or with an assistant. Even simple portable pulse oximeters can measure pulse and saturation in bedridden patients, as well as during sleep. For longer measurements, it is recommended to use instruments that continuously read data and display it on the screen. The monitor is attached to the wrist, and the data is accurate even if you do not hold your finger in a stationary position. These pulse oximeters are effective for diagnosing sleep apnea and for monitoring heart rate and saturation levels around the clock.
How to understand pulse oximeter readings
As a result of the measurement, all data is displayed on the monitor screen. The first indicator that a pulse oximeter reads is the pulse. It is displayed in the number of heartbeats per minute. In an adult, the normal pulse ranges from 60 to 90 beats per minute. It can increase after physical exertion, with chronic diseases of the heart and blood vessels, and also as a result of a sharp decrease in oxygen levels in the blood. The pulse is not a constant value and can change frequently, so to obtain more accurate data it is recommended to measure it several times at intervals of 3-4 minutes.
The second indicator for which portable pulse oximeters are used is saturation (SpO2). It is displayed as a percentage and indicates the level of oxygenated hemoglobin. In a healthy person at rest, it will correspond to 95% or more. However, if the monitor displays a result of 98–100%, it is worth repeating the procedure - the device may be faulty. The saturation level from 90 to 94% corresponds to 1 degree of hypoxia, from 75 to 89% - 2 degrees, from 60 to 75% - 3 degrees. When saturation decreases to 60%, hypoxic coma is observed, which poses a danger to the patient’s life. It is recommended to consult a doctor if the monitor displays a saturation level of 94% or lower - even minor oxygen deprivation can significantly affect the functioning of internal organs and tissues.
When is hospitalization and oxygen support needed?
- If the indicator has dropped to 93% and the patient feels unwell (hypoxemia, respiratory failure, respiratory symptoms are severe).
- With a significant percentage of lung damage on CT (> 50%, with CT-3, CT-4).
- Old age of the patient.
- Concomitant chronic diseases of the respiratory system.
- Concomitant chronic diseases of the cardiovascular system.
- Initially low saturation due to anemia.
- Pregnant women.
- Patients with immunodeficiency.
- Obese patients.
- For diabetes mellitus.
A decrease in saturation is dangerous primarily for these groups of patients.
If a hospitalized patient's saturation is low and does not rise even with oxygen, then, according to the current recommendations of resuscitators, the patient undergoes tracheal intubation.
Is it possible to quickly increase the saturation on your own?
Before the ambulance and oxygen therapy arrive, the patient can take the following measures:
1. Do breathing exercises
Sit up straight, lower your shoulders, straighten up and try to relax.
Exercise 1
- Raise one hand up and grab the floor lamp/beam/door handle to secure the position of your hand.
- Place your other hand on the diaphragm. Breathe deeply, lifting your diaphragm as you inhale.
Exercise 2
- Continue to hold one arm up while keeping the other extended forward.
- As you inhale, turn your body towards your outstretched arm (if your left hand is raised, turn your body to the left and vice versa).
Exercise 3
- Breathe deeply with one arm raised up. The hand is fixed on any object (floor lamp) or wall.
Open the windows and ventilate the room.
Lie on your stomach for up to 30 minutes.
Important! Due to individual anatomical characteristics, elderly patients should not lie on their stomach - compression of the respiratory organ is possible.
There is no evidence that any medications can effectively increase saturation in a coronavirus patient. However, in the absence of individual intolerance and the presence of aspirin in the home medicine cabinet, the use of this drug is acceptable.
The anticoagulant aspirin is associated with a reduction in the need for mechanical ventilation and admission to the intensive care unit, as well as a reduction in mortality in patients hospitalized with COVID-19.
In general, doctors who worked with seriously ill patients have repeatedly noted that oxygen therapy, or rather the constant stay of the patient “on oxygen,” is less effective than breathing exercises. The patient must breathe independently, under the supervision of medical personnel, “kneading” and stimulating the lungs.
Important! Performing the popular exercise with “inflating” balloons is not permissible in cases of lung damage KT-2, KT-3, KT-4 and especially in elderly patients, since the damaged and overstretched pulmonary matrix may simply not withstand the load.
COVID-19 and pulse oximetry at home
COVID-19 and pulse oximetry at home: how to get correct saturation results?
Currently, there is a sharp rise in the incidence of COVID-19: this is felt by both outpatient clinics and hospitals. One of the main issues that must be resolved at the outpatient stage of medical care is how not to miss the deterioration of the condition of a person who has contracted a coronavirus infection.
This is especially significant when monitoring patients who are traditionally at risk for complicated and severe COVID-19:
1) persons over 65 years of age
2) patients with chronic concomitant pathology (especially diabetes mellitus, oncohematology, serious diseases of the cardiovascular and pulmonary systems, chronic renal failure, liver cirrhosis, drug immunosuppression - taking cytostatics, glucocorticosteroids, etc.).
3) overweight persons (a body mass index of 30 or more already increases the risk of severe COVID-19!)
Recently, devices for assessing hemoglobin oxygen saturation—pulse oximeters—have become significantly cheaper and have become available to the population.
Key points for their correct use to identify developing respiratory failure and promptly seek medical help.
- A portable pulse oximeter (clip-on pulse oximeter) consists of a sensor and a display and runs on a battery. To perform the measurement, the sensor is placed on the patient's finger.
- How it works: Pulse oximeter sensors have light-emitting diodes that illuminate tissue with two types of red light. A sensitive element on the opposite side detects light passing through the tissue and, based on its characteristics, determines what kind of hemoglobin is contained in the pulsating (arterial) blood. The pulse oximeter display shows the SpO2 saturation value (percentage of hemoglobin saturation with oxygen) as a percentage, the heart rate value, as well as the pulse wave, which determines the blood flow itself.
- It is important to follow certain principles in order to obtain correct saturation measurement results:
— correctly position the sensor on the finger (usually choose the index, middle or ring finger; the sensor should fit snugly to the nail bed, but not squeeze the finger too much);
— if varnish is applied to the nail plate, it is optimal to remove it (otherwise there may be errors in saturation measurement);
— if you doubt the correctness of the pulse oximeter readings in a sick person, first measure the saturation in a healthy person;
— to correctly measure saturation, the pulse wave on the display of the pulse oximeter must be clearly visible, its waves ideally look the same after the same period of time;
— the hands of the patient whose saturation is measured should not be cold (otherwise they must be warmed);
— while measuring saturation, the hand should not move.
- Normally, the saturation value for an adult should be above 95% . But even here there are exceptions. For example, patients with chronic obstructive pulmonary disease and some other diseases may initially have low saturation values. Therefore, it is important for them to fix the initial saturation value at the onset of the disease and then monitor its changes during the treatment process.
- In a patient with COVID-19, it is optimal to assess saturation at least 3 times a day (every 8 hours). A single low saturation value (<94%) is often a consequence of incorrect measurement or the temporary influence of some factor that changes pulse oximetry readings. Therefore, it is important to recheck this indicator over time after a few minutes, using the other hand. If the saturation indicator upon repeated measurement also turns out to be low or continues to decrease to an even greater extent, we seek medical help. , a heart rate above 120 per minute are “ red flags ” , usually requiring hospitalization .
- It is necessary to especially carefully monitor the value of saturation in patients at risk for severe and complicated COVID-19, starting from the 5th day of illness. The same should be done in patients without the risk factors listed above, including young age, but for a long time (more than 5–7 days) maintaining a fever above 38.0–39.0 * C, poorly reduced by antipyretic drugs, and with pronounced manifestations of intoxication ( severe weakness, weakness, headaches, dizziness, muscle pain, etc.).
- If a patient with COVID-19 is seen at the clinic/hospital emergency department level and sent home for treatment, saturation and pulse monitoring should continue at home. Thus, one study in the UK showed that if a patient with coronavirus infection sent home, when assessed at rest, developed a tachycardia above 120 beats per minute or saturation less than 92%, he needed to be readmitted to the hospital (Gootenberg D et al., BMJ Health Care Inform, 2021).
- Fitness trackers and smartwatches, even from well-known manufacturers, despite the ability to assess blood oxygen saturation, are generally not intended for medical use. You should not trust their readings too much in a patient with COVID-19, as diagnostic errors are possible.
Thus, pulse oximetry, in addition to clinical patient assessment, may be an effective tool for early identification of deteriorating COVID-19 patients in the outpatient setting.
Below are images of stationary pulse oximeter sensors, as well as the type of pulse wave and key indicators - saturation and heart rate displayed on the pulse oximeter display.
Source of information: Nikita Solovey · View on Medium
How to increase saturation after viral pneumonia?
If even after suffering from coronavirus the saturation is slightly reduced, then this is normal - the lung tissue needs time to restore the previous vital capacity of the respiratory organ. Breathing exercises (see Strelnikova’s set of breathing exercises) and walks in the fresh air with moderate physical activity are extremely useful.
To prevent aggressive adhesions in the lungs in patients with fibrous changes evident on CT; usually with CT-4, CT-3, less often with CT-2 and very rarely with CT-1, antioxidant therapy for pulmonary fibrosis is prescribed, which includes a diet enriched with antioxidants, acetylcysteine, and vitamins E (if there are no allergies).
To clarify the diagnosis and causes of reduced saturation after coronavirus, CT control is important.
How to saturate the blood with oxygen if the lungs are not working
The main methods of treating distress syndrome are artificial ventilation (ALV) and extracorporeal membrane oxygenation (ECMO).
A ventilator is essentially a compressor that, one might say, forces oxygen into the patient’s lungs. To do this, doctors insert an endotracheal tube into the trachea. A special humidifier heats the air from the ventilator to body temperature and humidifies it. The device also removes exhaust air - carbon dioxide.
Patients are given medications that relax the diaphragm and other muscles—effectively immobilizing them—to allow the machine to fully regulate breathing.
There is also non-invasive ventilation, when the patient is put on a mask with a tube over the mouth and nose, but the tube is not inserted into the respiratory tract.
An ECMO machine is like an artificial heart and lung for the patient. To connect the device to the body, special long devices, called cannulas, are inserted into the patient’s large blood vessels. Through them, the blood enters the oxygenator - a device with a special membrane, with the help of which oxygen is added to the blood, and carbon dioxide (exhaust air) is removed.
The oxygenated blood is then warmed and returned to the patient's body. To comply with physiological mechanisms, blood sampling and infusion occurs as close to the heart as possible.
New ventilator in Barnaul Clinical Hospital No. 11.
Anna Zaikova.
When else does a person have low saturation?
- For heart defects;
- With hypoventilation of the lungs (with a slowdown in the frequency of exhalations and inhalations);
- For anemia;
- For chronic diseases of the lungs and bronchi (COPD, emphysema);
- If the oxygen concentration in the air is reduced;
- For diffuse disorders;
- Under excessive loads;
- When smoking;
- If you are overweight;
- When there are changes in atmospheric pressure;
- At night (from 3 to 7 o’clock) and in the deep sleep phase;
- When he is under general anesthesia.
How is saturation measured?
Saturation is measured with a pulse oximeter. Ambulance teams are equipped with mobile devices. You can also purchase it for home monitoring. The device resembles a clothespin that is attached to your finger.
Within a minute, a sensor with LEDs reads data, namely the color of the blood (hemoglobin), which changes depending on the saturation, as well as a specific pulsating light signal that changes depending on changes in blood pressure.
The pulse oximeter display shows two numbers - the top one shows the percentage of oxygen in the blood, the bottom one shows the pulse.
Saturation is measured in a sitting or lying position, the patient's hand should lie on the surface and not hang in the air.
Hospitals also use invasive devices to help laboratory technicians measure blood gases. To do this, it is taken from an artery or vein.
Important numbers
Oxygen in the human body is the driver of the formation of 90% of energy. Saturation is an indicator that reflects the degree of oxygen saturation in the blood. A low level may indicate heart defects, blood disorders, and respiratory diseases. Among them are pneumonia, pneumonia, tuberculosis, and bronchitis. This is why it is so important to monitor saturation in patients who have recovered from COVID-19: this virus causes interstitial lung damage, which causes the body to lack oxygen. This is manifested by the following symptoms: a person experiences weakness, drowsiness, fatigue, and difficulty breathing.
© Andriy Onufriyenko/Moment/Getty Images
Blood oxygen levels (oxygenation) vary depending on age and health status.
For adults and children over one year of age, the values are 94–99%. In newborns, the rates range from 93 to 96%. For patients with chronic lung diseases - 92–95%.
After suffering from COVID‑19, the permissible values are 90%, but already at this level unpleasant symptoms make themselves felt, primarily hypoxia and oxygen deficiency.