Types of interferons
Interferons are the main antiviral proteins in the body. They are part of the cytokine family.
Based on the similarity of biological activity in the human body, there are 3 types of interferons. A variety of interferons of the same type is needed to duplicate the antiviral defense function in the body.
| Interferon | Number of genes | Homology | Interferon type |
| IFN-alpha | 13 | 80% | Type I |
| IFN-beta | 1 | 60% | Type I |
| IFN-omega | 1 | 40% | Type I |
| IFN-kappa | 1 | 30% | Type I |
| IFN-lambda 1 | III type | ||
| IFN-lambda 2 | III type | ||
| IFN-lambda 3 | III type | ||
| IFN- lambda 4 | III type | ||
| IFN-gamma | Type II |
Interferons of one type are determined by binding to specific cellular receptors. In the cytoplasm of cells, the same molecules are associated with them.
The task of type 1 and 3 interferons is cell activation and expression of interferon-stimulated genes.
Type 2 interferon (interferon gamma) has different receptors, different signaling and different activation of signaling pathways. This is due to the fact that it is not an antiviral interferon, but more of an immunomodulator. The name “interferon” was given to it historically, since it was discovered simultaneously with type 1 and 3 interferons.
Use of interferon drugs in medicine
Interferon drugs are actively used in the treatment of a wide range of viral diseases. In particular, we are talking about the human papillomavirus, viral hepatitis, herpes infection, as well as influenza and colds. An important factor in the selection of drugs containing interferon for the treatment of a particular disease will be the concentration of interferon in the drug, how it is obtained and what type of interferon (α, β, γ or λ) it contains. Despite the fact that there are interferon preparations that are available without a prescription, it is still better to consult a doctor in advance, since there are a number of contraindications for these drugs. Based on the method of preparation, interferon preparations can be divided into 4 types6,7:
- Leukocyte interferon is obtained from donor blood.
- Lymphoblastic interferon is obtained from a culture of lymphoblastic cells.
- Recombinant interferon is obtained from bacterial or fungal cultures into which the human gene responsible for the production of interferon has previously been inserted. Most often, interferon preparations contain recombinant interferon.
- Pegylated interferons are produced by combining recombinant interferon with polyethylene glycol. This is done to ensure that the drug lasts longer in the body.
Virus life cycle
The first stage is entry into the cell, the second stage is replication, the third stage is exit from the cell. Antiviral defense proteins fight the virus at all stages and block its replication. It is important that all these proteins are synthesized under the influence of interferons.
When a virus enters a cell, it activates the signaling pathway and type 1 interferons are expressed. Next are two ways:
- One leads to the expression of interferons, and interferon triggers the expression of interferon-stimulated genes.
- The second path leads to the expression of pro-inflammatory cytokine genes - the inflammatory response is triggered.
In most cells, between 200 and 500 genes are activated in response to interferon, all of which are involved in antiviral defense.
| Major interferon-stimulated genes | Mechanisms of antiviral defense |
| PKR | Viral protein translation block |
| MX1 | Transcription suppression |
| OAS1 | Activation of RNase L for viral genome degradation |
| APOBEC3G | Replication suppression, cytidine deamination |
| TRIM5 | Capsid formation block |
| ZAP | Binding to viral RNA |
| ISG15 | Binding to viral proteins |
| ADAR | Suppression of RNA virus replication |
| IFITM1/2/3 | Helicase block, replication suppression |
Advantages and disadvantages of introduced interferons
The advantages of drugs containing interferons include their availability. An important advantage of interferons is their possible use against a wide range of viruses.
The relatively high level of safety of interferon drugs allows them to be used by children, who, as is known, often suffer from influenza and other acute respiratory viral infections.
However, along with the advantages, such drugs also have their disadvantages. Often, excessive amounts of type 1 interferon are associated with suppression of innate antibacterial immunity mechanisms8 and can also provoke a decrease in the production of intrinsic interferon9.
Immunomodulatory effect of interferons
The biological action of type 1 interferons is associated with the activation of several types of cells of the immune system. These are dendritic cells, cytotoxic t-lymphocytes, natural killer cells, macrophages, t-regulatory cells.
One of the most important mechanisms of antiviral defense is the lysis of our own cells infected with viruses. It is provided by killer T cells and NK cells.
This is the polytropic principle of action of cytokines:
- Expression of receptors on cells of different origins and functions.
- Signal transmission using several different intracellular messengers and transcription factors.
At first glance, different biological functions are associated with the fulfillment of one common goal - antiviral protection. This is why interferons are so effective. They can trigger all defense mechanisms in the body without exception.
What is interferon
Antibiotics help us fight bacteria. But with viruses it’s not so simple. For a long time, there were no weapons against viral infections. But today this is no longer the case. In addition to umifenovir and neuraminidase inhibitors, we can counteract viruses with interferon-based drugs. This affordable type of therapy became especially relevant when outbreaks of the new viral disease COVID-19 hit humanity. According to recent studies, high doses of interferon are highly effective in the treatment of this serious illness and other acute respiratory viral infections.
In China, the possibilities of interferon therapy were studied in 77 adults with moderate COVID-19. The study showed that interferon-alpha-2b helps reduce virus concentrations in the upper respiratory tract of subjects, and also prevents the development of inflammation in the body.
Interferon is not one compound. Interferons include a whole group of cytokine proteins with similar properties. All of them are produced by human cells as protective agents when attacked by viruses, bacteria, and also in response to the influence of certain low-molecular substances.
Perhaps the most important property of interferons is the ability to inhibit the reproduction of viruses, and in a very elegant way. Interferons themselves do not harm viruses, but they force cells at the site of infection to produce a cascade of enzymes that block the synthesis of viral proteins (Fig. 1). But that's not all. Interferons, in response to a viral infection, activate many genes responsible for protecting the body from enemy invasions, activate the immune system and push infected cells to self-destruction - apoptosis.
Figure 1. Interferons attach to cells and induce them to produce antiviral enzyme proteins.
Illustration: MedPortal
The three main types of interferons include:
- alpha interferons (produced by leukocytes),
- interferons beta (produced by fibroblasts),
- interferons-gamma (produced by cells of the immune system).
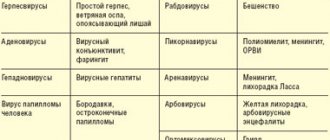
Alpha interferons show high effectiveness in the treatment of severe viral infections (Fig. 2) and those acute respiratory viral infections that we encounter every spring and autumn. One of the most famous is interferon-alpha-2b (IFN-alpha-2b). It is used as a means of therapy against influenza and other diseases associated with damage to the body by viruses.
What is ARVI? The culprits of ARVI or colds are viruses. Most often these are influenza (types A and B viruses), parainfluenza, adeno- and coronaviruses. The latter includes the new virus SARS-CoV-2, responsible for the COVID-19 pandemic. ARVI is characterized by:
- airborne transmission (the virus travels through the air along with microdroplets released when sneezing or coughing and enters the body, settling on the mucous membrane of the nasopharynx),
- damage to the respiratory system (infection develops in the upper respiratory tract, gradually affecting the lower ones),
- rapid development and acute course (colds are usually accompanied by fever, muscle aches, severe fatigue, sore throat, cough, congestion and runny nose).
Most often, ARVI occurs in a relatively mild form and does not last long, but sometimes a cold ends in complications. If symptoms do not subside for more than a week, the likelihood of developing bronchitis, sinusitis, pneumonia, myocarditis (inflammation of the heart muscle), otitis media and even meningitis increases. Therefore, it is necessary to treat ARVI, not only by relieving the symptoms, but also by supporting the body in the fight against the virus.
Imbalance of innate and acquired immune responses
The task of innate immunity is to block viral replication through the synthesis of interferon and to induce adequate synthesis of proinflammatory cytokines to activate acquired antiviral immunity.
However, highly pathogenic influenza viruses induce a hyperinflammatory response with hypersynthesis of proinflammatory cytokines. A state of acute hypercytokinemia develops. It happens that it is not supported by a sufficient level of endogenous interferon and the development of effective acquired immunity. Then inappropriately strong inflammation occurs, the development of respiratory distress syndrome, pulmonary edema and death of patients in especially severe cases.
Interferon inducers
Interferon inducers are substances that induce the cell to produce its own interferon. They can have a different nature, be of natural or synthetic origin. Among the products in this group you can find: meglumine acridone acetate, gossypol copolymer (plant pigment), tilorone.
Interferon inducers are used for the prevention and treatment of acute respiratory viral infections along with recombinant interferon, but for a pronounced therapeutic effect they need much more time, from 2 to 5 days. As a rule, medications in this group are available in tablet form and have age-related contraindications for use. Also recommended for the treatment of herpes.
Counteracting viruses to the body's immune system
Different types of viruses have learned to block the first signaling pathway – the induction of interferon synthesis. Moreover, they block the second signaling pathway – the action of interferon itself. Violation of interferon synthesis leads to severe viral diseases.
To fight viruses that block the action of interferon, humanity has learned to make additional interferon molecules. These genetically engineered molecules are completely identical to endogenous ones. With their help we can overcome the blocking effect of viruses.
When the influenza virus, coronavirus, or MS virus infect the upper respiratory tract, the synthesis of just a few cytokines is activated.
If the lower respiratory tract is infected by these viruses, hypersecretion of mucus, collapse of the alveoli, infiltration of immune cells, and impaired air exchange as a result of pulmonary edema may develop. In this case, the synthesis of most cytokines increases. This suggests that in severe cases, infection with the virus leads to activation of the immune system, and if there is a lack of interferon alpha, it can lead to severe clinical manifestations.
Emergency immunoprotection against viruses
The effectiveness of natural interferons (produced in the body) has been proven more than once10. For this reason, given the disadvantages of drugs containing interferons, it is more advisable to stimulate the production of the body’s own interferon. Interferon inducers cope with this task. These are drugs that stimulate the production of one’s own (endogenous) interferon. Interferon inducers, unlike introduced interferons, are slightly allergenic, and most importantly, they cause prolonged production of endogenous IFN in physiological doses sufficient to achieve therapeutic and preventive effects11.
A natural activator of the immune system and, in particular, stimulation of its own interferon are bacterial lysates, which stimulate local immunity without affecting the functioning of the general immune system. One of these is the IRS®19 spray, which contains lysates of 18 bacteria that most often cause respiratory diseases. Unlike systemic immunomodulators, IRS®19 acts locally without interfering with the functioning of the general immune system. It is noteworthy that bacterial lysates are destroyed microorganisms that cannot cause disease, but do induce an immune response14. IRS®19 can be used by both adults and children from 3 months12, which indicates its safety profile. This is especially important because children’s immune systems, which have not yet strengthened, are less able to cope with respiratory infections, which is why children get sick more often13.
The advantage of IRS®19 is that in addition to activating the production of its own interferon, the drug naturally enhances other factors of local immune defense of the nasopharyngeal mucosa: phagocytosis, increases the level of lysozyme and the production of local antibodies, in particular, secretory immunoglobulin A, which makes it possible to cope with both viruses and viruses. and with bacteria. This complex effect on local immunity helps speed up the healing process by 2 times1. IRS®19 acts on the cause of the disease, prevents infection from entering the body and reduces the risk of complications by activating antiviral and antibacterial mechanisms of emergency immunoprotection at the entrance gates of infection13. When IRS®19 is sprayed, a fine aerosol is formed that covers the nasal mucosa, which leads to the rapid mobilization of protective mechanisms12,14.
Another important advantage of IRS®19 is the possibility of using the drug for preventive purposes. Immunological memory after a course of IRS®19 application lasts on average about 4 months13. Such prevention is especially relevant during the season of viral attacks for both adults and children.
Our body, in the process of evolution, has adapted to fight viruses, but if necessary, we can help it without interfering too much with its work.
Scientific and clinical effectiveness of interferon alpha for the prevention and treatment of ARVI
A 2014 study on human cell cultures using electron microscopy proved the antiviral effect of interferon alpha.
In 2013, treatments for experimentally infected monkeys were studied. Treatment with interferon alfa and ribavirin demonstrated a significant reduction in the development of symptoms of viral pneumonia, respiratory failure and a decrease in the synthesis of proinflammatory cytokines.
To date, the clinical effectiveness of intranasal interferon alpha for viruses has already been shown:
- Adenovirus
- Coronavirus
- Rhinovirus
- Influenza A virus (H1N1, H3N2)
- Influenza B virus
- Parainfluenza virus
- Respiratory syncytial virus
Recombinant interferon alpha, administered externally into the respiratory tract, can enhance the antiviral effect.
Local application of interferon alfa allows the drug to be administered exactly where the drug is intended to act. Now there are various dosage forms: nasal drops, aerosol, spray. Local rather than systemic use can significantly reduce the dose of interferon alpha and eliminate side effects.
The use of intranasal interferon alpha can give a good preventive effect during an epidemic of influenza, coronavirus and other respiratory viruses.
Interferons and antiviral immunity
Interferons are a group of regulatory proteins characterized by the unique ability to suppress viral reproduction without affecting the metabolism of host cells. One of the representatives of this class of drugs is VIFERON®. The drug is approved for use in acute respiratory viral infections, viral pneumonia, labial and genital herpes, cytomegalovirus and enterovirus infections, virus-associated glomerulonephritis, meningeal forms of tick-borne encephalitis, various forms of mumps.
Acute respiratory viral infections (ARVI) lead in the structure of morbidity throughout the world. The relevance of the problem of influenza and other acute respiratory viral infections is due to the consistently high incidence rate in all age groups of the population, especially in the children's population, as well as polyetiology, the emergence of new viruses with a changed structure and new properties that cause outbreaks and pandemics.
According to the World Health Organization, during interpandemic periods around the world, on average, about 1 billion people get sick with influenza every year, with 3-5 million of them developing severe forms of infection, and from 300,000 to 500,000 of those infected dying. The maximum mortality rate from respiratory infections is observed among young children and the elderly, which makes influenza and ARVI the leading position in terms of medical and social significance among all diseases. For example, in Russia, out of the total number of cases of temporary disability associated with infectious diseases, the share of temporary disability in the adult population caused by ARVI and influenza accounts for about 12–14% [1–3]. At the same time, influenza, due to the unique ability of the virus for genetic variability, still remains an uncontrolled infection and causes the emergence of new strains, against which the existing population immunity turns out to be untenable.
Despite the long history of creating active preventive immunization against ARVI, doctors and patients only have influenza vaccines in their arsenal [4].
MT Osterholm et al. A meta-analysis of randomized controlled trials of influenza vaccines published from 1967 to 2011 assessed the effectiveness of immunization in terms of the relative reduction in the risk of morbidity caused by all circulating influenza viruses. Data included in the meta-analysis from ten trials of trivalent vaccines in eight of 12 seasons indicated a 59% effectiveness in immunizing adults [5]. Based on this, the authors of the meta-analysis stated:
- influenza vaccines can provide moderate protection against virologically confirmed influenza, but the degree of protection varies widely, up to complete absence in some seasons;
- live attenuated influenza vaccines are consistently highly effective in children six months to seven years of age;
- New, more effective vaccines are needed to further reduce influenza morbidity and mortality [5].
To enhance protection against pathogens that infect or penetrate mucous membranes, in particular ARVI pathogens, mucosal delivery of vaccines has been proposed, reproducing the process of natural infection of mucous membranes. In addition to the well-studied intranasal and oral administration, alternative routes have been proposed - rectal, paramucosal, sublingual. In addition, it is possible to use eye drops [6, 7].
The severity and speed of development of clinical manifestations of ARVI are determined not only by the properties of the pathogen and the massiveness of the invasion, but also by the activity of immune defense factors that initiate a complex system of protective and adaptive reactions aimed at limiting the reproduction of the pathogen and its subsequent elimination.
It has been proven that the clinical picture and characteristics of the course of infectious diseases directly depend on the level of cytokine production and the degree of their influence on immunoregulatory and effector immune mechanisms. The incidence of ARVI, as well as the severity, are associated with a certain type of response of the immune system, the main element of which are regulatory molecules - cytokines [3, 4, 8].
The primary targets for influenza viruses and other ARVI pathogens are the epithelial cells lining the respiratory tract. These cells, detecting the virus using pattern recognition receptors, initiate an immune response [9]. The main cells involved in innate defense responses against viruses in the respiratory tract, in addition to epithelial cells, are monocytes/macrophages, natural killer (NK) cells and dendritic cells. During viral invasion, epithelial cells produce chemoattractants (in particular, the chemokine CCL2), which attract alveolar macrophages and monocytes. Attracted and activated macrophages produce proinflammatory mediators that trigger antiviral immune responses, but also largely determine the local and general symptoms of the disease. Alveolar macrophages play a direct role in limiting viral spread by phagocytosis of antibody-coated viral particles and infected cells [4, 9]. Humoral and cellular adaptive immune responses are also important. As is known, antibodies to viral hemagglutinin have virus-neutralizing activity, while antibodies to viral neuraminidase block the spread of the pathogen. The protective effect against influenza is associated with a humoral response to some other antigens - the internal proteins of the virion - M2 and NP. Protection against viruses is provided not only by circulating antibodies, but also by mucosal secretory immunoglobulin (Ig) A, which directly protects the epithelium of the respiratory tract [10].
Analysis of works devoted to modulation of the immune response allows us to conclude that the main directions of immunotherapy for infectious diseases remain unchanged:
- modulation of innate immunity;
- modulation of acquired immunity;
- correction of the quantitative and qualitative composition of the intestinal microbiota [11].
Research on the relationship between the microbiota and the immune system has been considered a promising source of information for the development of immunomodulators [11, 12]. Non-pathogenic bacteria that colonize the human body generally have a beneficial effect on his health. The relationship between such microorganisms and the macroorganism is mutually beneficial. Moreover, in recent years, ideas about the mechanisms of interaction of bacteria with the human immune system, Th1/Th2/Th17/Treg subpopulations of lymphocytes have been modernized [13], ligand-receptor systems have been identified, through which bacteria provide strengthening of anti-infective defense and immune tolerance of the macroorganism [14] . The role of the predominant mucosal IgA isotype as a factor supporting symbiont colonization of mucous membranes has been reconsidered.
According to most experts, the central link of antiviral immune defense against ARVI pathogens is the interferon (IFN) system - cytokines, first discovered as mediators of the phenomenon of interference, that is, the prevention of recurrent viral infection [15, 16].
The discovery of IFN in 1957 by A. Isaacs and D. Lindenmann is considered one of the most important achievements of the last century. IFNs have an antiviral effect aimed at all known viruses. At the same time, IFNs are characterized by strict species specificity. IFNs are part of a biological multisystem - a cytokine network that carries out intercellular interactions and thereby maintains cellular homeostasis at a constant level. IFNs implement an innate nonspecific local and systemic reaction of the body in response to the introduction and replication of the virus [4].
Three types of IFN are known: the first (IFN-alpha, IFN-beta, IFN-omega, etc.), the second (IFN-gamma) and the third (IFN-lambda - interleukin (IL) 29, IL-28A, IL-28B) . IFNs of the first and third types are the most important components of innate antiviral defense. Type 1 IFNs are produced by various cells in response to viral invasion, while type 3 IFNs are produced predominantly by epithelial cells, including those of the respiratory tract, and play a significant role in protection against ARVI pathogens. The biological action of these types of IFNs is realized through different receptor-signaling systems. Nevertheless, the paths of the biochemical events induced by them converge at certain stages and lead to the expression of IFN-stimulated genes, the protein products of which block key stages of the virus life cycle - from its entry into the cell to the release of daughter virions. They potentiate adaptive cellular antiviral responses [14–16]. The cascade of reactions leading to the expression of IFN genes of the first and third types is triggered by pattern recognition receptors.
IFN-gamma is the main mediator that switches the differentiation of naive (immature) CD4+ T lymphocytes towards Th1 cells and potentiates adaptive cellular immune responses against virus-infected cells. The main producers of this cytokine are T lymphocytes and NK cells [17]. IFN-alpha/beta and IFN-gamma potentiate adaptive cellular antiviral responses, so they can be considered as a link between the innate humoral response and adaptive cellular defense. It is possible that IFN-lambda has even greater antiviral potential compared to IFN-alpha/beta in acute respiratory viral infections and other viral infections that mainly affect epithelial cells [18].
Thus, IFN is a group of regulatory proteins that have the unique ability to suppress viral reproduction without affecting the metabolism of host cells. They induce an antiviral effect in infected and neighboring uninfected cells, modulate the immune response by stimulating antigen presentation and macrophage function, cytokine production and the activity of dendritic cells and natural killer cells, and improve the adaptive immune response [19, 20].
Type I IFNs are produced by all nucleated cells in response to the introduction of foreign genetic information in the form of DNA and RNA molecules. The interaction of IFN with cells begins with the binding of the protein to specific CD118 receptors, which are expressed on most cells of the body (fibroblasts, lymphocytes, monocytes, macrophages, granulocytes and dendritic cells). The resulting complex (CD118 receptor + IFN) is immersed inside the cell, after which the bond is broken and the released CD118 receptor returns to the cell surface and restores its expression after 28–72 hours [21].
Increased production of IFN-alpha, type 1 IFN, occurs almost immediately after the introduction of the virus (30–40 minutes), and the increased concentration of this cytokine in the peripheral blood is determined already 2–8 hours after the onset of the infectious process. IFN-alpha is the most powerful activator of macrophages. In addition, it activates NK cells and suppresses the proliferation of T and B lymphocytes. An increase in the level of IFN-alpha in the acute period of viral infections with a decrease to normal during the period of convalescence characterizes the pathogenesis of many acute infections, including ARVI [19]. However, modern viruses are characterized by the ability to suppress innate defense mechanisms, including the production and biological function of IFN. A number of molecular mechanisms have been deciphered that allow respiratory viruses to resist the protective effect of IFN. The most studied methods of suppressing the innate immune response are those implemented by influenza viruses. The non-structural protein of the influenza virus NS1 blocks at different levels a cascade of biochemical events leading to the activation of genes for IFNs of the first and third types and other cytokines with mediated antiviral activity. NS1 inhibits the recognition of viral RNA, suppresses further signals aimed at the activation and translocation into the nucleus of interferon-regulating factor 3, nuclear factor kappa bi and activating protein 1, and directly inhibits the expression of type 1 IFN genes and other cytokines [22].
NS1 is not the only influenza virus protein that dampens the innate immune response. The viral proteins PB2 and PB1-F2 limit IFN-beta production by binding to mitochondrial antiviral signaling protein. The PA-X protein, discovered relatively recently, suppresses the expression of host genes involved in the initiation of the cellular immune response. The nucleoprotein inhibits the action of protein kinase R, the most important antiviral factor induced by IFNs of the first and third types [23]. Mechanisms that other respiratory pathogens, in particular parainfluenza viruses and metapneumoviruses, use to counteract innate defense responses have been revealed. They also block the production of type 1 and type 3 IFNs and the antiviral signals induced by these cytokines. Respiratory syncytial virus suppresses the synthesis of IFN types 1 and 3 [10] and apoptosis of infected cells, potentiating virus reproduction [24]. Thus, there is an urgent need for treatment methods that can overcome these features of respiratory viruses, in particular the introduction of IFN from the outside.
Currently, three most significant criteria have been identified that should be taken into account when deciding on the prescription of a particular immunomodulatory drug: effectiveness - experimentally proven immunotropic activity and clinical effectiveness due to cellular and molecular mechanisms for the implementation of pharmacological effects, safety and physiology of the immune modulation caused by the drug. In addition, the immunomodulatory agent must have a known structure and/or have a technologically stably reproducible composition [12].
In Russia, IFN drugs and their inducers are traditionally used for the prevention and treatment of influenza. IFNs are physiological because they are natural mediators of effector and regulatory signals of the immune system. The undoubted advantages of this group of drugs include their high immunotropic activity, due to the presence of specific receptors for cytokines on the surface of immunocompetent cells. However, like all cytokines, they have too many-sided effects on the body, which does not exclude the possibility of developing side effects, especially when administered parenterally [20].
The history of the discovery and study of the properties of IFN indicates that the therapeutic potential of this class of cytokines has not been exhausted. IFN-alpha drugs are divided into two large groups: biological and human recombinant, for the production of which genetic engineering methods are used. Recombinant IFNs are a large group of drugs with high therapeutic and prophylactic properties. Dose optimization and combination of recombinant IFNs in various forms make it possible to achieve the best treatment results. The development of topical, rectal and oral forms of recombinant IFN-alpha, characterized by fewer side effects and other organ/tissue targets of action, has made it possible to expand the range of diseases in which IFNs have a pronounced therapeutic and preventive effect [15]. The creation of topical (ophthalmic, intranasal) and rectal forms of IFN partly solved the problems of delivering these drugs to the zone of pathogen invasion and side effects caused by parenteral administration of cytokines [16].
Topical forms of IFN are administered directly to the primary sites of viral entry in the upper respiratory tract and act on the corresponding receptors of epithelial and other cells of this biotope. In this case, a small part of IFN can enter the systemic blood circulation and the central nervous system.
Currently, a special place in the complex therapy of ARVI is given to IFN drugs of the first and second types. Type I IFNs combine a number of positive properties of suppressing the proliferation of all known respiratory viruses, a sufficient duration of antiviral action and a high therapeutic effect. Type II IFNs do not have a direct virostatic effect and are classified as immunotropic drugs. These drugs help accelerate the apoptosis of viral cells, interrupting the reproduction of the virus in them. Topical and rectal forms of cytokines, mainly type I IFN, are the means of choice for the prevention and complex treatment of ARVI [15, 25, 26].
Back in 1981, it was shown that during acute viral infection the level of IFN increases significantly. At the same time, more than 70% of cells are in a state of antiviral status, and in severe viral infections, the IFN system is in a state of functional deficiency [27]. Acute viral infection can lead to depletion of the IFN system and transient immunosuppression. As a consequence, the addition of a secondary infection cannot be ruled out [28]. At the same time, viruses can not only evade the effects of IFN, but also inhibit its action and disrupt its production through a variety of mechanisms.
Numerous studies have revealed the presence of congenital and acquired defects of the IFN system associated with low levels of IFN production [29]. Congenital disorders in the IFN system were systematized in 2014 [30]. They have been shown to contribute to severe viral and bacterial intracellular infections, often leading to death.
The therapeutic potential of IFN drugs is in the area of special attention today. This is evidenced by data from studying the pharmacokinetics of rectal forms of IFN-alpha. It has been proven that topical and rectal forms of IFN are acceptable for strengthening anti-infective protection in different parts of the respiratory tract. Preference is given to the safe and highly effective recombinant IFN-alpha-2b - the drug VIFERON®. The suppositories contain human recombinant (without the use of donor blood components) IFN-alpha-2b, vitamins E and C and a base of cocoa butter. The composition of the drug VIFERON® ointment includes human recombinant IFN-alpha-2b, vitamin E and a mixture of anhydrous lanolin with medical petroleum jelly as a base, the composition of the drug VIFERON® gel - human recombinant IFN-alpha-2b, alpha-tocopherol, methionine, benzoin and citric acid and gel base excipients. The therapeutic effect of the drug VIFERON® is ensured not only by the recombinant IFN-alpha-2b included in its composition, but also by the entire complex. It has been established that during the development of the infectious process, regardless of the type of pathogen, the antioxidant activity (AOA) of the blood plasma is significantly reduced, which leads to increased lipid peroxidation (LPO) and damage to cell membranes. As a result, membrane interactions between IFN molecules and cellular receptors for IFN are disrupted, and signal transmission into the cell is disrupted. In addition, against the background of increased permeability of lysosomal membranes caused by viruses and increased lipid peroxidation, the release of cellular lysosomal proteases accelerates. As a result, the proteolytic activity of blood plasma increases and conditions are created for a high rate of inactivation and catabolism of circulating IFN molecules.
The membrane-stabilizing components included in the drug VIFERON® - antioxidants vitamins E and C - have a normalizing effect on the LPO/AOA ratio in the blood plasma and prevent the accelerated inactivation and catabolism of IFN, thereby increasing the antiviral activity of recombinant IFN-alpha-2b by 10-14 times.
The research results suggest that there is no formation of antibodies that neutralize the antiviral activity of recombinant IFN-alpha-2b.
One of the modern drugs in this series is VIFERON® gel - a dosage form developed by FERON LLC (Russia). This is a complex drug that includes human recombinant IFN alpha-2b, membrane-stabilizing components and a base. Natural antioxidant vitamin E and its synergists - citric and benzoic acids, methionine help stabilize cell membranes. The gel base ensures a prolonged effect of the drug and forms a protective film that protects against secondary infection.
The complex composition of the drug VIFERON® gel determines a number of new qualitative characteristics: in the presence of antioxidants, citric and benzoic acids, the specific antiviral activity of recombinant IFN increases tenfold, its local immunomodulatory effect is enhanced, and the content of locally formed immunoglobulins of class A increases [31–35]. The dosage form in the form of a gel makes the use of the drug simple, safe and painless.
The inclusion of the drug VIFERON® gel in the treatment regimen for ARVI is accompanied by the restoration of the secretory IgA content in nasal secretions, which was reduced at the onset of the disease in most children [36].
The drug VIFERON® gel, used for ARVI in children to lubricate the nasal passages and tonsils, the drug VIFERON® in the form of suppositories help reduce the duration of all clinical manifestations of the infectious process [33–36].
In order to optimize preventive measures for influenza and ARVI, an assessment was made of the epidemiological and immunological effectiveness of the antiviral drug VIFERON® gel in organized military groups [37]. The epidemiological effectiveness coefficient of the drug was 50.2%, the effectiveness index was 2.0. A 2.1-fold decrease in the incidence of bronchitis was recorded. The drug increased the general nonspecific resistance of the body and statistically significantly increased the initially reduced induced production of IFN. The drug was well tolerated by patients and did not cause side effects or allergic reactions.
The clinical effect of using the drug VIFERON® in pregnant women with acute respiratory infection was comparable to the effectiveness in groups of pregnant women receiving neuraminidase inhibitors or VIFERON® in combination with neuraminidase inhibitors [33, 34].
The results of many years of clinical studies of the effectiveness of VIFERON® drugs, modern regimens and doses of therapy used in clinical practice are presented in the work of I.V. Nesterova [38].
Thus, IFNs, as natural factors of nonspecific defense of the body and mediators of immunity, have the widest spectrum of action. Many years of practice and numerous clinical studies have confirmed that the use of various forms of the drug VIFERON® reduces the duration of all clinical manifestations of the infectious process, significantly reduces the period of release of viral antigens, restores the functioning of endogenous IFNs, normalizes the balance of indicators in the "LPO/AOD" system and stabilizes local and systemic immunity.
The complex composition of the drug, included in traditional treatment programs for many diseases, makes it possible to significantly reduce the dose and duration of the course during antibacterial and hormonal therapy, and reduce the toxic effect of chemotherapy. The drug is approved for use in such virus-associated diseases as ARVI, viral pneumonia, labial and genital herpes, cytomegalovirus infection, enterovirus infection, virus-associated glomerulonephritis, meningeal forms of tick-borne encephalitis, various forms of mumps. The drug is approved for use by patients of all age categories, even premature newborns (only VIFERON® ointment is prescribed from one year of age), pregnant women from 14 weeks of gestation, as well as during lactation.
Effect of endogenous interferon levels on protection against influenza virus
In 2021, it was experimentally proven that restoration of intestinal microflora improved the synthesis of interferon by lung epithelial cells.
The study was conducted on mice. Antibiotics disrupted the composition of the intestinal microflora. As a result, the level of interferon in the lungs decreased and resistance to experimental infection with the influenza virus decreased. A severe course of the disease was observed as the virus replication became more active.
Normalization of the microbiota restored interferon synthesis and protection against the influenza virus. The study proved that the stimulating effects of intestinal microflora provide tonic signals to activate the expression of interferon genes.
Recombinant interferon preparations
Recombinant interferons are the most successful on the market, they are created using genomic technologies and produced by microbial synthesis. Producing interferon from modified E. coli is much cheaper than isolating cytokines from human blood cells and allows for the production of drugs in large quantities. Moreover, the structure of recombinant interferon is identical to natural proteins.
Recombinant interferons-alpha (in particular, IFN-alpha-2b) are most often used in practice today. As a result of treatment of ARVI with interferon, the duration of illness is reduced, the manifestation of flu-like symptoms is reduced, and the risk of developing complications after viral infections is significantly reduced.
How is interferon taken?
The main methods of delivering interferon to the body as part of anti-cold products: intranasal and rectal. The intranasal route of administration is safe, but ineffective if the product is an aqueous solution. In this case, the absorption of interferon in the nose is hindered by mucous mucus, which repels water (more about this in the article “Current aspects of immunoprophylaxis of ARVI and COVID-19 in difficult epidemiological conditions”).
Gels are an excellent alternative to aqueous solutions for intranasal administration. They stay on the mucosal surface longer and are highly effective as a therapeutic and prophylactic agent against ARVI and COVID-19, including in children. The gel can be applied to the mucous membranes of the nose and mouth (tonsils) to prevent infection or during illness to reduce the rate of spread of infection by activating local immunity.
An interferon-based gel reduces the number of relapses of respiratory viral diseases for several months after completing a course of medication.
The most effective method of delivery remains rectal - interferon-based drugs are available in the form of rectal suppositories (Fig. 2). This method does not cause unwanted side effects and guarantees rapid absorption of the drug in the intestine (the drug is directly absorbed into the blood, bypassing the liver), due to which interferon begins to work within 15-20 minutes after administration.
Figure 2. Dynamics of release of pathogen antigens from the throat and nose of children with ARVI during treatment using IFN-alpha-2b.
Source: elibrary.ru
The combined use of rectal suppositories and topical gel is more effective in the treatment of ARVI and helps to quickly reduce the severity of symptoms (Fig. 3).
How to increase the bioavailability of interferon?
Some interferon-based medications also contain well-known antioxidants: vitamins C and E. Their role is to reduce oxidative stress and fight free radicals that destroy our cells day after day.
Tocopherol not only protects cell membranes from oxidative damage, but also serves as an excellent chemical conductor. Being fat-soluble, it easily overcomes transepidermal barriers, opening the way for other active substances, for example, interferon. It is not surprising that interferon preparations containing tocopherol acetate show increased effectiveness in the treatment of viral infections.
What drugs contain interferon?
Today there are many medicines on the market that have the root “feron” in their names. However, not all of them contain interferon. For example, “Anaferon” and “Ergoferon” do not contain interferon, and also do not contain any significant quantities of any active ingredients; these are homeopathic remedies. "Cycloferon", in turn, contains meglumine acridone acetate and belongs to the group of interferon inducers.
Recombinant interferon-alpha-2b contains over-the-counter antiviral drugs: “Viferon” (rectal suppositories or gel for topical use, also contains vitamins C and E), “Grippferon” (nasal spray), “Genferon” (rectal suppositories ).