Key Facts
- Hepatitis B is a viral infectious disease that affects the liver and occurs in acute or chronic form.
- Transmission of the virus most often occurs perinatally from mother to child, as well as through contact with blood or other biological fluids, in particular during sexual contact with an infected partner, unsafe injection practices, cuts with piercing instruments in medical practice and in domestic conditions, and also among people who inject drugs.
- WHO estimates that in 2021, there were 296 million people worldwide living with chronic hepatitis B (i.e. positive for hepatitis B surface antigen).
- An estimated 820,000 people died from hepatitis B in 2021, primarily as a result of hepatitis-related liver cirrhosis and hepatocellular carcinoma (primary liver cancer).
- As of 2021, 30.4 million (10)% of all people living with hepatitis B were aware of their infection, and 6.6 million (22%) of all diagnosed patients were receiving treatment. According to the latest WHO estimates, in 2021 the proportion of children under five years of age with chronic hepatitis B has fallen to just under 1%, compared with the decades before the introduction of vaccination (i.e. from the 1980s to the early 2000s). x years) this figure was about 5%.
- According to WHO estimates, in 2021, despite the availability of a highly effective vaccine, the number of people primarily infected with hepatitis B was about 1.5 million people.
- Hepatitis B is preventable through safe, accessible and effective vaccines.
Hepatitis B is a potentially life-threatening infectious liver disease caused by the hepatitis B virus (HBV). This disease is a major health problem worldwide. The infection can become chronic with a high risk of death from cirrhosis and liver cancer.
There is a safe and effective vaccine that provides 98–100% protection against hepatitis B. Prevention of viral hepatitis B helps prevent the development of complications such as chronic hepatitis and liver cancer.
Mechanisms of transmission
In highly endemic areas, hepatitis B is most often transmitted either from mother to child during childbirth (perinatal transmission) or through horizontal transmission (contact with infected blood), especially between infected and uninfected children in the first five years of life. Infants who are infected from their mother, or children who become infected under 5 years of age, very often develop chronic infection.
Hepatitis B is also transmitted through needle sticks, tattoos, body piercings, and contact with infected blood and body fluids, including saliva, menstrual and vaginal fluids, and semen. Infection can also occur through the reuse of contaminated needles and syringes or sharps in medical institutions or in domestic settings, as well as among people who inject drugs. Infection can be transmitted through medical, surgical and dental procedures, tattooing, and the use of razor blades and similar devices contaminated with infected blood. In addition, the hepatitis B virus can be transmitted through sexual contact, especially among unvaccinated individuals who have multiple sexual partners.
Chronic hepatitis B develops in less than 5% of people infected as adults, and in about 95% of those infected during infancy and early childhood. The hepatitis B virus can survive outside the human body for at least seven days. During this period of time, the virus retains the ability to cause infection if it enters the body of an unvaccinated person. The duration of the incubation period for hepatitis B ranges from 30 to 180 days and averages 75 days. The virus is detected in the blood within 30–60 days after infection and can persist in the body, causing chronic hepatitis B, especially if infected during infancy or childhood.
Causes of hepatitis B
You can become infected with hepatitis B through contact with the blood or bodily fluids of a sick person without immunity to the virus.
Experts are confident that the risk of infection for tourists visiting potentially dangerous regions is low, but it naturally increases when performing certain activities - dental or medical treatment, unprotected sex, and so on. Therefore, tourists are recommended to get vaccinated against hepatitis B before visiting countries with a high prevalence of infection.
Hepatitis B is transmitted as follows:
- drug addiction when one needle is used by several people;
- penetration of infected blood into a healthy body through cuts, scratches or open wounds;
- use of non-sterile instruments during dental or medical procedures;
- through the blood of laboratory technicians or medical staff;
- blood transfusions in countries where blood is not tested for hepatitis B;
- piercing, tattoos, manicure, pedicure with poor sterilization of instruments and lack of sanitary and hygienic conditions in the salon;
- use of personal hygiene products by strangers;
- unprotected sex with an infected person - including oral and anal;
- vertical route of infection - women with hepatitis B can transmit the infection to their child during pregnancy or childbirth.
Symptoms
In most cases, the primary infection is asymptomatic. However, some patients experience acute symptoms with severe symptoms that persist for several weeks and include icteric discoloration of the skin and sclera, dark urine, severe weakness, nausea, vomiting and abdominal pain. In rare cases, acute hepatitis can lead to acute liver failure with a risk of death.
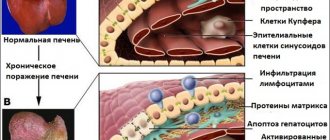
In some people, the hepatitis B virus can also cause a chronic liver infection, which over time can develop into cirrhosis (scarring of the liver) or liver cancer.
Complications of hepatitis B
One of the dangerous complications of hepatitis B is acute liver failure. It develops according to the following scenario:
- Precoma I - the patient’s condition sharply worsens, a specific liver odor appears from the mouth, spatial and temporal orientation is lost, fine motor skills are impaired, and pain is possible.
- Precoma II - impaired consciousness progresses, hemorrhagic and intoxication syndromes intensify, the liver shrinks and disappears under the ribs, tremor of the limbs and tongue appears.
- Terminal stage - the creature is depressed, reflexes weaken and disappear completely. Death occurs as a result of acute cardiovascular failure.
Important! A complication of chronic hepatitis B is cirrhosis of the liver.
Who is at risk for chronic hepatitis B?
The likelihood of developing a chronic infection depends on the age at which a person became infected with the hepatitis virus. Chronic infection is most likely to develop in children infected with the hepatitis B virus before the age of six.
Infants and young children:
- in infants infected in the first year of life, chronic infection develops in 80–90% of cases;
- Children infected before the age of six develop chronic infection in 30–50% of cases.
Adults:
- in people infected with hepatitis B as adults, in the absence of other concomitant diseases, chronic infection develops in less than 5% of cases;
- if chronic infection develops in 20–30% of adults, the disease leads to cirrhosis and/or liver cancer.
Diagnostics
Based on the clinical picture alone, it is impossible to differentiate between hepatitis B and other types of viral hepatitis; Therefore, laboratory confirmation of the diagnosis is extremely important. Several laboratory blood testing methods are available to diagnose and monitor patients with hepatitis B. They can be used for differential diagnosis of acute and chronic infections.
Methods for laboratory diagnosis of infection include detection of hepatitis B surface antigen (HbsAg). To ensure blood safety and prevent accidental transmission of the virus to recipients of blood products, WHO recommends systematic testing of donated blood for hepatitis B.
- Acute HBV infection is characterized by the presence of hepatitis B virus surface antigen (HBsAg) and antibodies to core antigen (HBcAg) - class M immunoglobulins (IgM). During the initial phase of infection, patients also develop hepatitis B virus e antigen (HbeAg). HBeAg is usually a marker of high levels of viral replication. The presence of HBeAg indicates the highly contagious nature of the blood and biological fluids of the infected person.
- Chronic infection is characterized by the persistence of HBsAg for at least six months (with or without the simultaneous presence of HBeAg). The persistent presence of HBsAg is a major marker of the lifetime risk of developing chronic liver disease and liver cancer (hepatocellular carcinoma).
Forecast and prevention of viral hepatitis B
With timely and proper treatment, acute hepatitis B can have a favorable prognosis. However, the consequences are directly dependent on the response of the immune system and the aggressiveness of the virus. The circulation of viral DNA in the human body for more than six months is an unfavorable sign and indicates the chronicity of the pathological process. The prognosis for people with chronic liver disease depends on which part of the liver is damaged and how well the body responds to treatment.
General recommendations for the prevention of viral hepatitis B are to comply with sanitary and hygienic standards, which are aimed at reducing the risk of possible infection during medical procedures.
It is also very important to observe the rules of personal hygiene (do not use other people’s razors and toothbrushes), and avoid casual unprotected sexual contact.
The best way to prevent hepatitis B is vaccination - it is carried out in the first six months of a child’s life.
If infection with viral hepatitis B occurs, it is important to know that there is no specific treatment for this disease. An infected person must take precautions to prevent spreading the virus to others.
Treatment
There is no specific treatment for acute hepatitis B. Therefore, medical care focuses on maintaining physical comfort and proper nutritional balance, including replacing fluid losses caused by vomiting and diarrhea. It is very important to avoid unnecessary drug treatment. Acetaminophen/paracetamol and antiemetics should not be prescribed to patients with hepatitis A.
For chronic hepatitis B, drug treatment may be prescribed, including oral antiviral drugs. Treatment can slow down the development of liver cirrhosis, reduce the risk of developing liver cancer and increase long-term survival rates for patients. WHO estimates that in 2021, 12 to 25% of people with chronic hepatitis B will need drug treatment (depending on conditions and selection criteria).
WHO recommends prescribing the oral drugs tenofovir and entecavir, which are the most effective drugs for suppressing the replication of the hepatitis B virus. Their use less often leads to the formation of drug resistance, is simple (1 tablet per day) and is not accompanied by significant side effects, and therefore there is no the need for careful monitoring of patients.
Entecavir is not a branded drug. In 2017, all low- and middle-income countries were able to legally purchase generic entecavir, although costs and availability varied widely. Tenofovir is no longer protected by patent in any country in the world. In 2021, the international median price of WHO prequalified generic tenofovir decreased from US$208 to US$32.
For most patients, drug treatment effectively suppresses viral replication but does not completely cure hepatitis B. Therefore, most patients who start treatment for hepatitis B must continue it for life.
In many resource-poor areas, access to hepatitis B diagnosis and treatment remains difficult. In 2021, of the more than 296 million people living with HBV, only 10% (30.4 million) knew of their diagnosis. Only 22% (6.6 million) of diagnosed patients were treated. Many patients are diagnosed in the later stages of liver disease.
Among the chronic complications of hepatitis B, high rates of morbidity and mortality are associated with advanced liver diseases such as cirrhosis and hepatocellular carcinoma. Liver cancer progresses rapidly and, given the limited treatment options, the outcome is usually poor. In low-income countries, most patients with liver cancer die within a few months of diagnosis. In high-income countries, the lives of such patients can be extended by several years through surgery and chemotherapy. Also in high-income countries, some patients with cirrhosis or liver cancer receive liver transplantation, but success rates for such treatment are variable.
Types and stages of the disease
The hepatitis virus affects the liver in acute or chronic form. Acute disease lasts up to 3 months, chronic disease - more than 6 months.
Currently, the following types of viral hepatitis are distinguished:
- A is the most common type of hepatitis, which rarely becomes chronic and most often has a favorable prognosis.
- B is a dangerous form of hepatitis, which can be protected from by vaccination.
- C is a severe form, which almost always becomes chronic with subsequent severe complications.
- D - a form similar to hepatitis B.
- E - similar to hepatitis A; with timely consultation with a doctor, it can be completely cured.
As for the stages of hepatitis B, they are as follows:
- The initial pre-icteric period lasts 1–2 weeks. It occurs with different symptoms. Most often, patients complain of joint pain in the morning and at night, rashes, loss of appetite, nervousness, apathy, and increased fatigue. In some cases, a bright, symmetrical papular rash may be observed. At the end of this period, the feces become discolored and the urine darkens.
- The icteric period lasts about a month. The skin turns yellow, and the patient's general condition worsens. Heaviness and pain appear in the right hypochondrium. Patients complain of bitterness in the mouth, severe itching of the skin that cannot be relieved by any medications, and nausea. The pulse becomes slower, swelling and hypotension occur.
- The final period - the patient’s condition returns to normal, the jaundice subsides. Depending on the state of the immune system, the disease can end in recovery or go into a chronic stage, which is expressed in scanty symptoms. The clinical picture becomes clear only at the stage of multiple organ complications or cirrhosis.
According to the severity of viral hepatitis B, there are:
- light;
- average;
- heavy.
According to the period of the disease, chronic hepatitis B is divided into exacerbation and remission.
Prevention
The main method of preventing hepatitis B is vaccination. WHO recommends that all newborns be vaccinated against hepatitis B as soon as possible after birth, within the first 24 hours of life if possible, followed by two or three doses of the vaccine at least four weeks apart to ensure full vaccination. Timely vaccination of children immediately after birth is an effective way to reduce the incidence of mother-to-child transmission of hepatitis B.
According to the latest WHO estimates, worldwide in 2021 the proportion of children under five years of age with chronic hepatitis B has fallen to just under 1%, compared with the decades before the introduction of vaccination (i.e. from the 1980s to early 2000s) this figure was about 5%.
This has achieved one of the Sustainable Development Goal targets for viral hepatitis elimination: reducing the prevalence of HBV infection among children under five years of age to less than 1% by 2021. This success was achieved in a number of regions with the exception of sub-Saharan Africa.
Increasing hepatitis B vaccination coverage worldwide over the past two decades has been a major public health achievement and has contributed to a decline in the incidence of hepatitis B infection among children.
In 2021, three-dose vaccine coverage reached 85% worldwide, up from around 30% in 2000. However, rates of newborn immunization against hepatitis B remain variable. Thus, the average rate of vaccination coverage with the first dose of hepatitis B vaccine immediately after birth is 43% worldwide, but in the WHO African Region it is only 6%.
A full course of vaccination produces protective antibodies in more than 95% of infants, children and young adults. Immunity acquired through vaccination lasts for at least 20 years and probably throughout life. Therefore, WHO does not recommend booster vaccinations for people who have completed the three-dose vaccine.
In countries with low or moderate endemicity of hepatitis B, vaccination is indicated for all unvaccinated children and adolescents under 18 years of age. In these countries, high-risk groups are more likely to become infected and should also be vaccinated. These risk groups include:
- individuals who frequently require blood or blood products, dialysis patients, and solid organ transplant recipients;
- prisoners in places of deprivation of liberty;
- injection drug users;
- persons who have household and sexual contact with people with chronic HBV infection;
- persons with multiple sexual partners;
- healthcare workers and other persons who may have contact with blood and blood products while on duty;
- International travelers who have not completed a full course of HBV vaccination and who are eligible for vaccination before departure to HBV-endemic areas.
The vaccine has an excellent safety and efficacy record and has reduced the proportion of children under five years of age with chronic HBV infection to just under 1% in 2021, compared with the decades before the introduction of the vaccine (i.e. since the 1980s). until the early 2000s), this figure was about 5%.
In addition to infant vaccination, which includes a timely first dose immediately after birth, WHO recommends prophylactic antiviral therapy to prevent mother-to-child transmission of hepatitis B. Pregnant women with a high concentration of HBV DNA (high viral load) and/or the presence of HBeAG in the blood are at high risk of transmitting the virus to their unborn child, even if the child receives the first dose of vaccine immediately after birth and completes the full course of vaccination against hepatitis B. Therefore, pregnant women with high The concentration of HBV DNA during pregnancy may indicate a prophylactic course of antiviral therapy to prevent perinatal HBV infection and protect the unborn newborn from the disease.
In addition to infant vaccination and prevention of mother-to-child transmission, HBV transmission can be prevented through blood safety measures, including quality screening of all donated blood and blood products used for transfusion. Globally, 97% of donated blood units were screened and quality controlled in 2013, but gaps remain. Effective measures to prevent the transmission of hepatitis B virus include ensuring safe injections and avoiding unnecessary injections and injections performed in unsafe conditions. Between 2000 and 2010, the rate of unsafe injections worldwide fell from 39% to 5%. In addition, one of the effective measures to prevent infection is to improve the safety of sexual intercourse, including minimizing the number of sexual partners and the use of barrier contraception (condoms).
Our phone numbers:
Human viral hepatitis represents a traditionally difficult global problem that is still far from being resolved. According to WHO estimates, hundreds of millions of people are infected with viral hepatitis in different countries of the world. This significantly exceeds the prevalence of HIV infection but, at the same time, has not attracted due attention. At the present stage, as in an earlier period, the high epidemic potential of all known viral hepatitis - A, B, C, D, E, G - remains high.
A completely unfavorable epidemiological situation regarding viral hepatitis has developed in the former Soviet Union. The number of patients with acute viral hepatitis reaches 1 million per year.
In the light of modern knowledge, the group of human viral hepatitis, called hepatitis A, B, C, D, E, G, includes nosologically independent infectious diseases, the characteristics of which are very diverse. The unifying principle is the hepatotropic nature of the pathogens, which determines the development of selective liver damage. Viral hepatitis A, B, C, D, E, G differ in all aspects - taxonomic affiliation of viruses, mechanism of infection and routes of transmission, pathogenesis and immunogenesis, clinical manifestations, severity and outcomes, likelihood of chronicity and malignancy, specific diagnostic criteria, different therapy and prevention programs.
The current stage is called the “golden era” of studying the problem of viral hepatitis. Thanks to the use of methods of virology, molecular biology, genetic engineering, in particular recombinant technology, new horizons for understanding the problem and its further study have opened up.
The Nobel Prize-winning discovery of the “Australian antigen” was the first in a chain of brilliant research that made the unknown known.
The causative agents of viral hepatitis - A, B, C, D, E, G - were discovered. The long-standing dream of clinicians about the separate specific diagnosis of viral hepatitis of different etiologies was realized not by exclusion or indirect signs, but on the basis of direct studies using highly specific and highly sensitive test systems . The use of new research methods has shown that the “hepatitis alphabet” is far from being exhausted. There remains a niche of viral hepatitis, neither A, nor B, nor C, nor D, nor E, nor G, caused by other pathogens.
Types of hepatitis viruses.
Hepatitis A
Of all the fairly numerous forms of viral hepatitis, hepatitis A is the most common. Although this disease is characteristic mainly of third world countries with poor hygiene and sanitation, isolated cases or outbreaks of hepatitis A can occur even in the most developed countries.
Hepatitis A virus is transmitted by the fecal-oral route. The most common route of transmission of hepatitis A virus is through close household contact between people and consumption of food or water contaminated with fecal material.
One of the most important factors on which the clinical manifestations of hepatitis A depend is age. Unlike adults, children do not have the “classic” picture of hepatitis A. Moreover, in young children, hepatitis A can be asymptomatic. The frequency of occurrence and severity of symptoms of the disease increases with age, so the icteric form of hepatitis A is characteristic of almost all adult patients. Elderly patients are more likely to develop a severe form of the disease, and they are more likely to develop severe complications of hepatitis A. Patients over 40 years of age are more likely to require hospitalization, and the mortality rate among them, compared to other age groups, is also higher. In typical cases, the clinical course of hepatitis A has four stages: the incubation period, the prodromal phase, the icteric phase and the convalescent period. An infected patient releases the virus in the initial stages of the disease, and the infection is transmitted to others long before the development of clinical symptoms. After the most contagious incubation period of 15 to 50 days, most patients with hepatitis A begin to experience prodromal symptoms of the disease. This is followed by the clinical manifestation of the disease, which is characterized by great variability of symptoms. As with other viral infections, the prodromal symptoms of hepatitis A are usually nonspecific, with patients experiencing weakness, gastrointestinal distress (including food aversions, diarrhea, and vomiting), and flu-like symptoms such as headache, chills, and fever. In addition, respiratory problems, muscle weakness, skin rashes and joint pain may often occur. The appearance of dark urine and uncolored feces at the end of the prodromal period are important signs indicating infection with the hepatitis A virus and usually cause the patient to seek medical help. At the end of the acute period of the disease, which usually lasts several weeks, most patients recover. However, in some cases, a relapse of the disease, the development of cholestatic jaundice or fulminant hepatitis may occur26. Patients who have recovered from the disease have long-term, possibly lifelong, immunity to hepatitis A. Long-term and persistent immunity to the disease is developed only after hepatitis.
Hepatitis B
This rather severe and common form of hepatitis is also called serum hepatitis. This name is due to the fact that infection with the hepatitis B virus can occur through the blood, and in an extremely small dose. The hepatitis B virus can be transmitted sexually, through injections with non-sterile syringes from drug addicts, or from mother to fetus. Hepatitis B is characterized by liver damage and occurs in different forms: from carriage to acute liver failure, cirrhosis and liver cancer. From the moment of infection to the onset of the disease, 50-180 days pass. In typical cases, the disease begins with fever, weakness, joint pain, nausea and vomiting. Sometimes rashes appear. The liver and spleen become enlarged. There may also be darkening of the urine and discoloration of the stool.
A specific reaction for diagnosing hepatitis B, or its carriage, is the detection of HbsAg. Treatment requires an integrated approach and depends on the stage and severity of the disease. The main drug was the immune drug - Interferon and its analogues. Hormones, hepatoprotectors, and antibiotics are also used. Various types of vaccines are used to prevent hepatitis B virus infection. To build immunity, the vaccination is repeated one month and six months after the first injection.
Hepatitis C
Hepatitis C is the most severe form of viral hepatitis, which is also called post-transfusion hepatitis. This means that they contracted it after a blood transfusion. This is due to the fact that testing of donor blood for the hepatitis C virus began only a few years ago. Quite often, infection occurs through syringes among drug addicts. Sexual transmission is possible from mother to fetus.
The greatest danger is the chronic form of this disease, which often develops into cirrhosis and liver cancer.
A chronic course develops in approximately 70-80% of patients. The combination of hepatitis C with other forms of viral hepatitis dramatically worsens the disease and can lead to death.
Hepatitis D
The causative agent of delta hepatitis has a defect, which means that the virus cannot reproduce independently in the human body; it requires the participation of a helper virus. This helper is the hepatitis B virus. This tandem gives rise to a rather serious disease. Doctors call this “union” a superinfection. Most often, infection occurs through blood transfusions, through syringes from drug addicts. Sexual transmission is possible from mother to fetus. All persons infected with the hepatitis B virus are susceptible to hepatitis D. The risk group includes hemophiliacs, drug addicts, and homosexuals.
Often, infection with hepatitis B and D viruses occurs simultaneously. From the moment of infection to the development of the disease, it takes 1.5-6 months, as with hepatitis B. The clinical picture and laboratory data are the same as for hepatitis B.
However, with mixed infection, severe forms of the disease predominate, often leading to liver cirrhosis. Doctors agree that the prognosis for this disease is often unfavorable. Treatment is the same as for hepatitis B.
Hepatitis E
Previously (before the detection of the hepatitis E virus), the disease, together with hepatitis C, D, G, was included in the group of so-called “neither A nor B” hepatitis. The mechanism of infection, like hepatitis A, is fecal-oral. That is, the disease is transmitted from a sick person who excretes the virus in their feces. Infection often occurs through water. As with hepatitis A, the prognosis is favorable in most cases. The exception is women in the last three months of pregnancy, in whom mortality reaches 9-40% of cases. Susceptibility to viral hepatitis E is universal. Mostly young people aged 15-29 years old become ill. The disease is especially common in countries with hot climates and extremely poor water supplies.
From the moment of infection to the onset of the disease, 14 to 50 days pass. Hepatitis E begins gradually with indigestion, deterioration in general health, and less often with a short rise in temperature. Unlike hepatitis A, the appearance of jaundice does not improve the health of patients.
After 2-4 weeks from the onset of the disease, a reverse development of symptoms and recovery is observed. Unlike other types of viral hepatitis, severe liver and kidney damage is observed in severe forms of hepatitis E. With hepatitis E, more often than with hepatitis A, moderate and severe forms of the disease are observed. Hepatitis E is characterized by a severe course in pregnant women in the second half of pregnancy with a high number of deaths. Fetal death occurs in almost all cases. Hepatitis E is not characterized by a chronic course and viral carriage. Treatment and prevention as for hepatitis A.
HepatitisG
Hepatitis G (Hepatitis G) is widespread. In Russia, the frequency of detection of the pathogen ranges from 2% in Moscow to 8% in Yakutia. According to the figurative expression of English doctors, hepatitis G is the younger brother of hepatitis C. Indeed, they have a lot in common. Hepatitis G is transmitted in the same way: through blood. This is reflected in the widespread prevalence of the disease among drug addicts. Infection also occurs during blood transfusions and parenteral interventions. Sexual transmission and vertical transmission from an infected mother to a child are possible.
In terms of clinical manifestations, hepatitis G also resembles hepatitis C. However, it is not characterized by the progression of the infectious process inherent in hepatitis C with the development of cirrhosis and cancer. As a rule, the acute infectious process is mild and asymptomatic. The main marker for diagnosing hepatitis G is the PCR (polymerase chain reaction) method.
The outcomes of acute hepatitis G can be: recovery, the formation of chronic hepatitis or prolonged carriage of the virus. Combination with hepatitis C can lead to cirrhosis.
Routes of infection, diagnosis and symptoms of hepatitis.
Hepatitis viruses enter the human body in two main ways.
A sick person can excrete the virus in their feces, after which it enters the intestines of other people with water or food. Doctors call this mechanism of infection fecal-oral. It is characteristic of the hepatitis A and E viruses. Thus, hepatitis A and hepatitis E arise mainly due to poor personal hygiene, as well as imperfect water supply systems.
This explains the greatest prevalence of these viruses in underdeveloped countries.
The second route of infection is human contact with infected blood. It is characteristic of hepatitis B, C, D, G viruses.
The greatest danger, due to the prevalence and severe consequences of infection, are the hepatitis B and C viruses.
Here are the situations in which infection most often occurs: - Donor blood transfusion. Worldwide, on average, 0.01 - 2% of donors are carriers of hepatitis viruses, so currently donor blood is tested for the presence of hepatitis B and C viruses before transfusion to the recipient. The risk of infection increases in persons who require repeated transfusions of blood or its products.
- Using the same needle by different people greatly increases the risk of contracting hepatitis B, C, D, G. This is the most common route of infection among drug addicts.
- Viruses B, C, D, G can be transmitted through sexual contact. Hepatitis B is most often transmitted sexually. It is believed that the likelihood of contracting hepatitis C in spouses is low.
- The route of infection from mother to child (doctors call it “vertical”) is not observed so often. The risk increases if a woman has an active form of the virus or suffered acute hepatitis in the last months of pregnancy. The likelihood of infection of the fetus increases sharply if the mother, in addition to the hepatitis virus, has HIV infection. The hepatitis virus is not transmitted through mother's milk.
Hepatitis B, C D, G viruses are transmitted through tattooing, acupuncture, and ear piercing with unsterile needles. In 40% of cases, the source of infection remains unknown.
Complications of viral hepatitis can include functional and inflammatory diseases of the biliary tract and hepatic coma, and if the disruption of the biliary tract is treatable, then hepatic coma is a formidable sign of the fulminant form of hepatitis, ending in death in almost 90% of cases. In 80% of cases, the fulminant course is caused by the combined effect of hepatitis B and D viruses.
Hepatic coma occurs due to massive necrosis (necrosis) of liver cells. The breakdown products of the liver tissue enter the blood, causing damage to the central nervous system and the extinction of all vital functions.
Recovery from viral hepatitis is long-term. Often, the disease takes on protracted forms. Some patients infected with the hepatitis B, C, D virus do not get sick themselves, but being carriers, they pose a danger in terms of infecting others. A very unfavorable outcome of acute hepatitis is its transition to the chronic stage, mainly with hepatitis C.
Chronic hepatitis is dangerous because the lack of adequate treatment inevitably leads to cirrhosis and sometimes liver cancer. In this regard, doctors consider hepatitis C to be the most serious disease: In 70-80% of cases, its acute form becomes chronic, although there may be no external signs of the disease. Moreover, the majority of patients with acute hepatitis C experience the phenomenon of “imaginary recovery”, in which the data of biochemical blood tests return to normal. This phenomenon lasts from several weeks to several months or even years, and patients may mistake this period for recovery. This dictates the need for long-term and regular monitoring of patients and mandatory specific therapy. Hepatitis C is not unreasonably compared in severity to AIDS.
But the most severe course of hepatitis is caused by a combination of two or more viruses, for example B and D or B and C. Even B+D+C is found. In this case, the prognosis is extremely unfavorable. Often, the signs of chronic viral hepatitis are mild, which allows a person to ignore the disease for the time being. Often, obvious clinical manifestations of the disease are detected already at the stage of cirrhosis.
Cirrhosis occurs in approximately 20% of people with hepatitis C. Hepatitis B with or without hepatitis D can also cause this complication. The presence of cirrhosis creates obstacles to normal blood flow in the liver. The blood is forced to find additional bypass routes, which leads to dilation of blood vessels in the esophagus and stomach.
These dilated blood vessels are called varicose veins; they stretch and can become a source of bleeding, requiring emergency medical attention. Another problem associated with the development of liver cirrhosis is ascites (accumulation of fluid in the abdominal cavity), which is externally manifested by an increase in the size of the abdomen. Sometimes, patients with cirrhosis develop liver cancer, which in the early stages can be treated with medications or surgery. If cirrhosis of the liver has formed, it cannot be eliminated, even if the inflammation of the liver has already passed. Therefore, treatment for viral hepatitis should be started as early as possible!
Treatment and prevention of hepatitis.
To protect yourself from hepatitis infection, you must follow simple rules.
You should not drink unboiled water, always wash fruits and vegetables, and do not neglect heat treatment of products. This way you can prevent infection with hepatitis A, the transmission of which is associated with food contamination from the feces of a sick person. The great rule “Wash your hands before eating” is a guarantee of health in this case as well.
In general, contact with other people's body fluids should be avoided. To protect against hepatitis B and C - primarily with blood.
Blood in microscopic quantities can remain on razors, toothbrushes, and nail scissors. You should not share these items with other people.
Medical institutions take measures to prevent hepatitis infection. However, if you had an endoscopy or dental treatment ten to fifteen years ago, when the fight against hepatitis was not yet carefully organized, you need to get checked. There is still a small risk of infection today.
Never share syringes and needles when taking drugs. Never perform piercings or tattoos with non-sterile equipment. Remember - the hepatitis virus is very tenacious and, in contrast to the AIDS virus, persists in the external environment for a long time (sometimes up to several weeks). Invisible traces of blood can even remain on straws used when using cocaine, so in this case, you should be wary of contamination.
Hepatitis B is most often transmitted through sexual contact, but infection with hepatitis C is also possible. It is especially necessary to take precautions during sex during menstruation and anal intercourse, however, oral sex can also be dangerous.
Hepatitis is also transmitted in the so-called “vertical” way - from mother to child during pregnancy, childbirth, and breastfeeding. With proper medical support, you can try to avoid infection of the baby - this will require careful adherence to hygiene rules and taking medications.
However, the route of hepatitis infection very often remains unknown. To be completely calm, you need to get vaccinated.
Currently, healthcare practice has effective vaccines only against hepatitis A and B. Intensive research is underway to develop a vaccine against hepatitis C, but it is at an early stage, because The high variability of the virus and the lack of an effective protective antibody response after hepatitis C infection make these studies difficult. In this regard, timely treatment of hepatitis C can prevent the development of severe progressive changes in liver tissue, which will certainly improve the patient’s quality of life.
It is not difficult to protect yourself from hepatitis A - one vaccination provides protection for more than 1 year. Second dose after 6 - 12 months. after primary provides long-term protection. For adults, the vaccine is administered in a dose of 0.5 ml into the deltoid muscle. Course - 3 vaccinations according to the schedule of 0, 1 and 6 months. Children are injected with 0.25 ml into the deltoid muscle twice with an interval of 1 month. As planned, medical workers, staff of preschool institutions, and service sector workers (primarily those employed in public catering establishments, water supply and sewerage facilities) are vaccinated against hepatitis A; traveling to regions and countries hyperendemic for hepatitis A (Middle East, Africa, Latin America, Indonesia); In the event of accidents at water supply and sewerage facilities (wastewater entering the water supply network), the population that used this water main is subject to vaccination against hepatitis A.
Since 1981, more than 1 billion doses of hepatitis B vaccines have been used worldwide with excellent safety and efficacy indicators; the vaccine is 95% effective in preventing the development of chronic carriage of the hepatitis B virus. The hepatitis B vaccine is the first anti-cancer vaccine, since chronic carriers of the hepatitis B virus are at high risk of mortality due to cirrhosis and liver cancer. Because of the critical importance of hepatitis B vaccine, the World Health Assembly recommended in 1992 that all countries should include hepatitis B virus vaccination in their national immunization schedules. To date, 100 countries have introduced hepatitis B vaccination into their national immunization schedules. In addition, adolescents are vaccinated in many industrialized countries. In some US states, newborns are vaccinated without exception.
The hepatitis B vaccine has been included in the national calendar of preventive vaccinations since 1996.
According to the National Preventive Vaccination Calendar, the first vaccination against viral hepatitis B is given to newborns in the first 12 hours of life, the second at the age of 1 month, and the third at 6 months.
Children born to mothers who are carriers of the hepatitis B virus or who are sick with viral hepatitis B in the third trimester of pregnancy are vaccinated against viral hepatitis B according to the schedule of 0-1-2-12 months.
Post-vaccination reactions when using the vaccine are rare. In 3.5-5% of cases, slight passing local pain, erythema and induration at the injection site are possible, as well as a slight increase in temperature, complaints of malaise, fatigue, joint pain, muscle pain, headache, dizziness, nausea. These reactions develop mainly after the first two injections and disappear after 2-3 days. Particularly sensitive people may develop immediate allergic reactions, so the vaccinated person requires medical supervision for 30 minutes.
Contraindications: hypersensitivity to yeast and other components of the drug, acute infectious and non-infectious diseases, chronic diseases in the acute stage (immunization is carried out no earlier than a month after recovery (remission)), decompensated forms of diseases of the cardiovascular system and lungs, pregnancy.
Conclusion.
Viral hepatitis is a common and dangerous infectious disease.
They can manifest themselves differently, but among the main symptoms are jaundice and pain in the right hypochondrium.
To diagnose hepatitis, you need to do a blood test, urine test, and in difficult cases, a liver biopsy.
Of all forms of viral hepatitis A is the most common. From the moment of infection to the appearance of the first signs of the disease, 7 to 50 days pass. Most often, the onset of the disease is accompanied by a rise in temperature, and may resemble the flu.
Most cases result in spontaneous recovery and do not require active treatment. In severe cases, droppers are prescribed to eliminate the toxic effect of the virus on the liver.
The hepatitis B virus is transmitted sexually, through injections with non-sterile syringes from drug addicts, and from mother to fetus.
In typical cases, the disease begins with fever, weakness, joint pain, nausea and vomiting.
Sometimes rashes appear. The liver and spleen become enlarged. There may also be darkening of the urine and discoloration of the stool.
Hepatitis C is the most severe form of viral hepatitis, which is also called post-transfusion hepatitis. This means that they contracted it after a blood transfusion. This is due to the fact that testing of donor blood for the hepatitis C virus began only a few years ago. Quite often, infection occurs through syringes among drug addicts. Sexual transmission is possible from mother to fetus.
The greatest danger is the chronic form of this disease, which often develops into cirrhosis and liver cancer.
A chronic course develops in approximately 70-80% of patients. The combination of hepatitis C with other forms of viral hepatitis dramatically worsens the disease and can lead to death. Hepatitis D is a “companion disease” that complicates the course of hepatitis B.
Hepatitis E is similar to hepatitis A, but it starts gradually and is more dangerous for pregnant women. The last in the hepatitis family, G, is similar to C, but less dangerous.