What is Escherichiosis?
Escherichiosis (coli infection, colibacillosis) is an acute intestinal infection caused by the gram-negative bacteria Escherichia coli (E.coli), or Escherichia coli, or more precisely, its pathogenic strains. The fact is that harmless strains of E. coli are normally present in the gastrointestinal tract of every person and even have a useful function, helping the body synthesize vitamin K and fight pathogenic microflora. They settle in the intestines of a newborn within the first day after birth and accompany him throughout his life. With escherichiosis, however, other strains of E. coli come into play and cause poisoning.
Depending on what kind of Escherichia the child’s body is infected with, in pediatric medicine it is customary to divide this disease into six subtypes:
- enteropathogenic (EPEC) - affects mainly infants of the first year. It practically never occurs in children over 3 years of age. Premature and weakened children, infants with rickets or anemia, and those who are bottle-fed are especially susceptible to it. It is characterized by pronounced diarrhea, vomiting, flatulence, and, since dehydration quickly begins in young children, it is quite dangerous. And since passive immunity has not yet been formed in children of the first year of life, and the gastrointestinal tract is more vulnerable due to its anatomical features, the infection often generalizes, affecting the entire body, up to the development of coli-sepsis.
- enteroinvasive (EIEC) – affects children of all age groups, mainly over 1 year. Its manifestations are very similar to shigellosis (dysentery), but are less common. The disease begins abruptly, with a jump in temperature and vomiting. In severe form, it practically does not occur in children older than one year.
- enterotoxigenic (ETEC) – occurs mainly in young children and forms stable immunity, therefore it is extremely rarely diagnosed in adults. It is transmitted mainly through food. Unlike other options, it is characterized by severe diarrhea and sometimes vomiting at normal body temperature (not higher than subfebrile values), which makes it similar to cholera. Rapid dehydration develops.
- enterohemorrhagic (EHEC) – usually diagnosed in preschool children from 1 to 5 years of age. It is often transmitted to humans from cattle. In severe forms, it can cause bleeding and necrosis of the intestinal walls.
- enteroaggregative and diffuse-adhesive types are very rare in children and can manifest as extraintestinal inflammation, for example, cystitis, cholecystitis, pyelonephritis.
Enteropathogenic escherichiosis in children
Treatment of patients with escherichiosis is based on the same principles as for other acute intestinal infections. Patients with a severe or moderate form (if they require infusion therapy) are required to be hospitalized. Mild forms are treated without hospitalization. Children for epidemiological reasons, newborns and those with severe concomitant diseases or complications are also admitted to the hospital. The diet should take into account the age of the child, the severity and period of the infectious process, and feeding before infection. Enteropathogenic escherichiosis in children mainly affects the small intestine, making it difficult for the child to digest food. Nevertheless, even with enteropathogenic escherichiosis, one should vigorously increase the amount of food (after appropriate unloading) and introduce new foods into the diet, but as the functional state of the gastrointestinal tract is restored, without leading to digestive failure. During pathogenetic therapy, urgent detoxification is necessary using drugs such as smecta, enterodes or enterosgel (as prescribed by the attending physician). For long-term enterosorption, it is desirable to use a hydrophobic selective enterosorbent that does not damage the intestinal barrier. If measures are carried out in a timely manner, the child’s chances for a speedy recovery without complications of the disease increase. Rehydration therapy is carried out taking into account the type of toxicosis and how dehydrated the child’s body is. Rehydration can be oral or intravenous. In most cases, the first named path is used. In severe forms of the disease, infusion therapy is prescribed (goals: rehydration, intoxication). For severe forms of the disease, the attending physician may prescribe prednisone. The dose is calculated as follows: 2-3 mg/kg body per day. Treatment with hydrocortisone is also possible, the dose of which is 5-10 mg/kg body per day. course of treatment is 3-5 days. Syndromic therapy may also be necessary, the prescription of vitamins, antihistamines, cardiovascular drugs, etc. If there are complications of a bacterial nature, antibiotics or chemotherapy are used. To prevent generalization of the process in newborns and children in the first months of life, antibiotic therapy is also prescribed. In mild cases, a balanced diet, oral rehydration, enzyme preparations, bacterial and symptomatic agents, and enterosorbents are prescribed. If, after a 5-7-day course of therapy with antibacterial drugs, intestinal dysfunction persists, eubiotics are used to restore normal intestinal flora. The same therapy is needed in case of confirmed intestinal dysbiosis. The course of treatment is 1-2 weeks. Diagnosis requires clinical and epidemiological data and requires laboratory confirmation. Diagnostics makes it possible to immediately suspect enteropathogenic escherichiosis in children only in typical forms of the disease. The disease in this case is indicated by gradually increasing toxicosis with exicosis, severe pallor of the skin, persistent infrequent vomiting, flatulence, frequent watery stools (abundant, mixed with transparent mucus), yellow or orange stools. Erased, mild and moderate forms are not easy to diagnose; laboratory diagnostics are required. The leading method is bacteriological. The study is carried out with the collection of feces of a sick child, sometimes vomit or oropharyngeal mucus, and gastric lavage. The luminescent research method allows you to obtain an approximate result within a few hours.
How can a child become infected with escherichiosis?
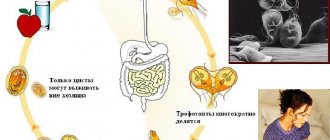
E.coli is usually transmitted through food or water, as well as through airborne dust and household contact, including from person to person. There are also known cases of infection from domestic animals. They can survive on the surfaces of objects at room temperature for more than 100 days, in milk for up to a month (and reproduce well in it), in infant formula for up to 3 months. They do not die when dried. At the same time, many strains have developed resistance to many antibiotics. They die only when boiled and when treated with disinfectants.
The seasonal increase in incidence depends on the strain: for EPEC it is winter-spring, for others it is summer.
Based on this, the prevention of colibacillosis comes down to compliance with generally accepted hygiene standards: washing hands and objects that the baby can put in the mouth with soap, washing vegetables and fruits, and, if possible, heat-treating foods.
How to understand that a child has escherichiosis?
Symptoms vary depending on the subtype of pathogenic bacteria, the age of the child, and the severity of the infection. They can be similar to many other gastrointestinal diseases - ranging from dyspepsia to salmonellosis and cholera. In addition, escherichiosis can cause complications: otitis media, cystitis, pyelonephritis and even meningitis. Therefore, for any manifestations of gastrointestinal damage, it is necessary to contact a competent pediatrician as soon as possible in order to begin treatment and avoid the development of severe forms of intoxication.
For infants, enteropathogenic (EPE) and enterotoxigenic (ETEC) forms are more typical. The symptoms for both are quite similar. With food transmission, the disease begins abruptly, with a rise in temperature, vomiting and diarrhea, with contact it is more gradual. The stools are watery, yellow or orange, sometimes foamy or mushy. Vomiting persists up to 2 times a day. Characterized by pale skin, bloating, flatulence, and decreased appetite. Manifestations reach their peak on days 5-7, then decline.
The remaining subspecies usually affect children older than one year. With the enteroinvasive form, the temperature rises (usually moderately), cramping pain in the abdomen occurs, and stool is scanty, mixed with mucus or blood. Symptoms of intoxication subside after the first two days. With the enterohemorrhagic variant, the temperature rarely rises, the stomach begins to ache very much, the stool is watery, and later an admixture of blood appears in it. The skin becomes very pale, and on days 3-5 the patient’s condition worsens.
To make a diagnosis, E. coli infection must be confirmed by laboratory testing. The test usually involves stool and/or blood. General blood and urine tests and a biochemical blood test are also required.
Escherichiosis (Coli infection)
Enteropathogenic escherichiosis
Class I EPEC usually develops in young children, the incubation period is several days, and is manifested mainly by vomiting, loose stools, severe intoxication and dehydration. There is a possibility of developing a generalized septic form. Adults get sick with class II EPKD, the disease proceeds like salmonellosis.
Enteroinvasive escherichiosis
EICP lesions are characterized by a course similar to dysentery or shigellosis. The incubation period lasts from one to three days, the onset is acute, moderate intoxication (headache, weakness), fever ranging from low-grade to high, and chills are noted. Then abdominal pain appears (mainly around the navel), diarrhea (sometimes streaked with blood and mucus). Palpation of the abdomen notes pain along the colon. Often, escherichiosis of this type occurs in a mild and erased form; a moderate course may occur. Usually the duration of the disease does not exceed several days.
Enterotoxigenic escherichiosis
ETC infection may manifest with clinical symptoms similar to those of salmonellosis, foodborne illness, or resemble a mild form of cholera. The incubation period is 1-2 days, intoxication is mild, the temperature usually does not rise, repeated vomiting, profuse enteritis diarrhea are noted, dehydration gradually increases, and oliguria is noted. There is pain in the epigastric region, which is cramping in nature.
This infection is often called “travelers' disease”, since it often affects people who go on a business trip or vacation to countries with a tropical climate. Climatic conditions contribute to the occurrence of severe fever with chills and intoxication symptoms, and intense dehydration.
Enterohemorrhagic escherichiosis
EHEC develops most often in children. Intoxication is moderate, body temperature is subfebrile. There is nausea and vomiting, loose watery stools. In severe cases, by the 3-4th day, the disease develops severe abdominal pain of a cramping nature, diarrhea intensifies, and an admixture of blood and pus may be noted in the stool, which loses its fecal character.
Most often, the disease goes away on its own after a week, but in severe cases (especially in young children), on days 7-10, after the disappearance of diarrhea, there is a possibility of developing hemolytic-uremic syndrome (a combination of hemolytic anemia, thrombocytopenia and acute renal failure). Cerebral regulation disorders are common: limb spasms, muscle rigidity, disturbances of consciousness up to stupor and coma. The mortality rate of patients with the development of this symptomatology reaches 5%.
How is Escherichiosis treated?
Children with mild illness are usually treated at home, where they are visited by a pediatrician from the clinic. Patients with moderate to severe disease are hospitalized, as well as usually newborns, since their doctors must monitor them constantly.
Typically, the pediatrician prescribes rehydration therapy for the patient to replenish fluid and electrolyte levels, symptomatic therapy to alleviate his condition, probiotics, enterosorbents, enzymes and sometimes immunoglobulins. Antibiotics are prescribed to children under one year of age and to patients in moderate to severe condition.
As with any intestinal disorder, diet is very important. Infants need to be fed in smaller portions, but more often than usual. Gradually, the volume of each feeding increases, as does the interval between them.
The prognosis is favorable in most cases.
MAKE AN APPOINTMENT PRICES