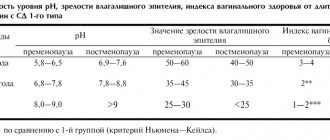
Detailed description of the study
Prothrombin, or factor II of the blood coagulation system, acts as a precursor to thrombin (the most important component in the formation of a blood clot). It is constantly present in the blood plasma and is activated at the moment of tissue or organ damage. As part of the blood coagulation system, it participates in the formation of a blood clot (thrombus), which prevents excessive blood loss during injury.
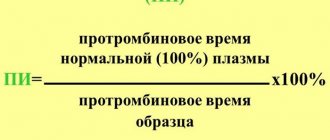
Prothrombin time (PTT) and prothrombin index (PTI) are indicators that characterize one of the stages of blood coagulation. Prothrombin time measures the number of seconds it takes for a blood clot to form after certain reagents are added to a blood sample being tested. Prothrombin index is the ratio between the clotting time of control (so-called healthy) blood plasma and the test sample. Determination of these indicators is necessary to assess the functioning of the entire blood coagulation system.
When tissue is damaged and subsequent bleeding occurs, the human body initiates a blood clotting process called hemostasis. Hemostasis involves a series of sequential chemical reactions (coagulation cascade). This cascade involves blood clotting factors, which are activated one after another and lead to the formation of a blood clot.
To ensure a normal coagulation process, there must be a sufficient amount of all factors in the blood, each of which must be functionally active. Insufficient activity can lead to excessive blood loss, excessive activity can lead to excessive clotting.
The test evaluates the overall ability to form a blood clot over a certain period of time (measured in seconds). The prothrombin index expresses the ratio of the clotting time of the test blood plasma to the control (normal) plasma.
Tests of prothrombin time and prothrombin index are ordered on a regular basis when a person is being treated with anticoagulant drugs (Warfarin) to ensure that the drug is having the desired effect.
Also prescribed if a person has signs or symptoms of excessive bleeding, such as frequent unexplained bleeding (nose, gum), multiple bruises.
PTT and PTI studies are performed before planned surgery when there is an increased risk of blood loss or when the person has had episodes in the past that indicate abnormalities in the blood clotting system.
A shortening of prothrombin time and an increase in the prothrombin index may indicate increased blood clotting and is mainly diagnosed in thrombosis, as well as thrombophilia (high risk of thrombosis).
The study of prothrombin time and determination of the prothrombin index indirectly allows us to assess the deficiency of prothrombin complex factors (II, V, VII, X).
During pregnancy, an additional uteroplacental circulation is formed, thanks to which the mother's blood, along with nutrients, flows to the fetus. Increased activity of the blood coagulation system (hypercoagulation) in the third trimester of pregnancy is a physiological process aimed at preparing for childbirth and preventing massive bleeding. Determination of prothrombin time and prothrombin index in pregnant women is mandatory research, since in case of changes associated with insufficient activity of coagulation factors, the risk of bleeding (including postpartum bleeding), placental abruption, and spontaneous termination of pregnancy increases.
Prothrombin time during pregnancy
Monitoring the clotting rate is important during pregnancy, especially when taking medications that affect clotting. The normal rate for pregnant women is considered to be a clotting rate of 18-25 seconds.
Deviation from the norm can lead to complications during pregnancy, the most dangerous of which is DIC syndrome (disseminated intravascular coagulation). In pregnant women it occurs for two reasons:
- placental abruption, accompanied by bleeding;
- amniotic fluid embolism;
- endometritis.
Often, pregnancy ends spontaneously as a result of antiphospholipid syndrome, which causes blood clots to form in the arteries and veins. These deviations lead to disruption of intrauterine development.
References
- Zobova, D.A., Paramonova, T.K., Tyurina, N.A. et al. Pathology of the hemostatic system in very early premature birth. – Journal of scientific articles, health and education in the 21st century, 2021. - No. 8. — P.185-187.
- Ponizovich, E.V., Zolotavina, M.L., Chernyavskaya, O.V. Changes in blood hemostasis in patients suffering from viral hepatitis. — Scientific forum: medicine, biology and chemistry, 2021. — pp. 13-17.
- Haram, K., Mortensen, J., Mastrolia, S. et al. Disseminated intravascular coagulation in the HELLP syndrome: how much do we really know? — The journal of maternal-fetal and neonatal medicine, 2017. — Vol. 30(7). — P. 779-788.
Prothrombin, INR (Prothrombin, INR)
Prothrombin is one of the most important laboratory indicators of a coagulogram, characterizing the state of the coagulation system.
Material for research: blood plasma.
Research method: coagulometry (Quick calculation).
Execution time: 1 day
Taking blood for Prothrombin analysis in the BRIGHT-Bio central laboratory.
Preparation for the study: blood is taken on an empty stomach. At least 8 hours (preferably 12 hours) must pass between the last meal and the test. Juice, tea, coffee (especially with sugar) are not allowed. You can drink water.
Units of measurement and conversion factors: %
BRIGHT-Bio measures prothrombin according to Quick (%). For patients taking indirect anticoagulants, Prothrombin is calculated in INR units. Therefore, if necessary, Prothrombin should be reported in INR units.
Indications for prescribing a blood test for Prothrombin:
- Study of blood coagulation pathology
- Screening study of the state of the coagulation system
- Control of blood clotting during long-term treatment with indirect anticoagulants (coumarins, etc.)
- Study of liver functions - assessment of the synthesis of prothrombin complex factors in the liver.
Functions of Prothrombin. A coagulation test in which the clotting time of the patient's plasma is determined after adding a mixture of tissue thromboplastin and calcium ions to it. Determination of prothrombin time and prothrombin according to Quick is a way to assess the deficiency of prothrombin complex factors and the activity of the extrinsic coagulation pathway. The test results, with normal content and quality of fibrinogen, depend on the content of factors II, V, VII, X (activity of the prothrombin complex). The formation of the main factors of the prothrombin complex occurs in the liver, so this test is often used to assess its protein synthesizing function. The synthesis of these coagulation factors in the liver depends on the presence of vitamin K in the body, the antagonists of which are indirect anticoagulants or indirect anticoagulants (ANDA), therefore the prothrombin test is used to monitor therapy with indirect anticoagulants. The most commonly used AEDs are 4-hydroxycoumarin derivatives - monocoumarols (phenprocoumarol, acenocoumarol), among which warfarin (synonyms - Aldocumar, Athrombin - K1, Cofarin, Coumadin, Coumadine, Cumatox, Omefin, Orfarin, Marevan, Panwarfin, Prothromadin, Warfilone, Warnerin).
The results of the prothrombin test can be presented in the following forms:
1. Prothrombin according to Quick (%) - like the prothrombin index, allows you to determine the activity of the prothrombin complex of the patient’s plasma in comparison with the measured prothrombin time of the control plasma. But in this case, the calculation is carried out according to the curve of the dependence of prothrombin time on the % content of prothrombin complex factors, constructed using different dilutions of control plasma. This way of presenting results is more accurate, especially in the low value range. The prothrombin index and Quick prothrombin may coincide with each other in the range of normal values. In the area of low values recommended for the management of patients taking indirect anticoagulants, the performance of these tests diverges. A prothrombin index of 50-60% may correspond to 30-40% prothrombin according to Quick. Calculation of prothrombin according to Quick is currently a generally accepted method.
Reference values for Prothrombin according to Quick: 70-130%
2. INR (International Normalized Ratio) , Latin abbreviation INR (International Normalized Ratio) is an additional way of presenting the results of a prothrombin test, recommended for monitoring therapy with indirect anticoagulants by the WHO expert committee, the International Committee for the Study of Thrombosis and Hemostasis and the International Committee for Standardization in Hematology.
The optimal INR limits that should be achieved during treatment with indirect anticoagulants depend on the therapeutic goals and are determined by the attending physician.
In patients not taking anticoagulants, normal Prothrombin INR is 0.85 - 1.15. For patients taking indirect anticoagulants, normal Prothrombin INR is 2.0-3.5.
Diseases and conditions in which the concentration of Prothrombin may change
Increased concentration of Prothrombin
- Tendency to thrombosis: thromboembolic conditions, myocardial infarction, pre-infarction conditions, hypohydration due to increased blood viscosity, hyperglobulinemia
- Medicines that inhibit the action of coumarin (barbiturates, vitamin K) or can inhibit it (corticosteroids, oral contraceptives, meprobamate)
- Antihistamines
- Polycythemia
- Malignant tumors.
Decrease in Prothrombin concentration
- Hereditary or acquired deficiency of factors I, II, V, VII and X
- Idiopathic familial hypoprothrombinemia
- Acquired and hereditary hypofibrinogenemia
- Vitamin K deficiency in diet (factors II, VII, X are formed in hepatocytes in the presence of vitamin K)
- Vitamin K deficiency in the mother (hemorrhagic diathesis in the newborn)
- Medicines - vitamin K antagonists (anticoagulants - phenylin, etc., coumarins and drugs that enhance their effect: anabolic steroids, clofibrate, glucagon, thyroxine, indomethacin, neomycin, oxyphenbutazone, salicylates, heparin, urokinase / streptokinase).
INR and prothrombin according to Quick correlate negatively - a decrease in prothrombin according to Quick corresponds to an increase in INR.
Attention to the Patient
- the concept of norm is not absolute and has no clear boundaries
- Normal reference values often vary significantly among people of different sexes and age groups.
Remember that only your attending physician, who knows your medical history well, can provide a clear interpretation of the test results.
To the attention of the DoctorReference limits for healthy and sick people are often largely the same. You can contact your BRIGHT-Bio consultant for more information. |
Lengthening time
Prolongation of Prothrombin time occurs in the following conditions:
- deficiency or anomaly of prothrombin complex factors when taking indirect anticoagulants, vitamin K deficiency, factor V deficiency, afibrinogenemia, hypofibrinogenemia;
- diseases of the liver and biliary tract;
- treatment with unfractionated heparin;
- hypocoagulation phase of DIC syndrome;
- syndrome of massive blood transfusions, against the background of colloid transfusion.
The APTT test is very informative for assessing the internal (platelet-vascular) component of blood plasma coagulation.
This test is sensitive to deficiency of all coagulation factors (except VII), to heparin (the test is used to monitor the effect of heparins), to specific inhibitors (antibodies to factors VIII and IX) and to nonspecific inhibitors (lupus anticoagulant) of coagulation factors.