CC dossier
Elena Shvedkina
endocrinologist, “Be Healthy” Clinic
city: St. Petersburg
Testosterone is the predominant hormone in a man’s blood, produced predominantly (95%) by the testicles, and in much smaller quantities by the adrenal cortex; formed from cholesterol. About 6 mg of testosterone is released into the blood plasma per day, and a small amount is deposited in the testicles. In plasma, testosterone is transported using sex steroid binding globulin (SSBG) or other blood proteins such as albumin. A small part circulates in the blood in free form.
Classification
Depending on the level of damage to the hypothalamic-pituitary system, the following are distinguished:
- hypergonadotropic hypogonadism (primary) in men. Testosterone production by the testicles is reduced or absent. Here we can distinguish congenital forms (Klinefelter syndrome - Fig. 1, anorchidism) and acquired forms (trauma, radiation, chemotherapy, other toxic lesions of the testicles, late initiation of treatment for cryptorchidism);
- hypogonadotropic (secondary) hypogonadism in men. Pituitary hormones that stimulate testosterone secretion are reduced or absent. This group also includes congenital forms (Kalman syndrome, isolated LH deficiency, other rare congenital diseases accompanied by hypogonadism), and acquired forms (tumors of the pituitary gland and hypothalamus, their surgical treatment or radiation therapy, hemorrhages in them, etc.);
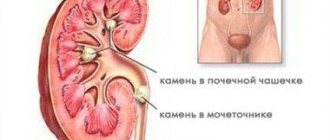
- normogonadotropic hypogonadism. This condition is characterized by low testosterone production with normal levels of gonadotropins. It is based on mixed disorders in the reproductive system, expressed not only in primary damage to the testicles, but also in hidden insufficiency of hypothalamic-pituitary regulation. Typical examples are hypogonadism in obese men, hypogonadism with hyperprolactinemia (Fig. 2) and hypothyroidism, age-related hypogonadism (Fig. 3), iatrogenic hypogonadism;
- hypogonadism due to target organ resistance (feminization as a result of tissue receptor resistance to androgens; 5α-reductase deficiency; deficiency of estrogens, which in physiological concentrations are modulators of the normal effects of testosterone).
Figure 1. Example of patients with Klinefelter's sign
Based on the time of occurrence, prepubertal and postpubertal hypogonadism can be distinguished.
Signs of testosterone deficiency
The importance of testosterone cannot be understated. It affects the condition of the body, and therefore its lack can lead to extremely adverse consequences. You can suspect a hormone deficiency based on the following symptoms:
- deterioration of attention, decrease in concentration;
- decrease or disappearance of libido;
- erection problems;
- increased fatigue;
- decreased strength, decreased muscle mass;
- reduction in the size of the prostate gland and testicles (they acquire a soft consistency);
- hot flashes;
- decreased level of red blood cells, causing anemia;
- brittle bones (osteoporosis);
- infertility caused by a decrease in sperm count.
Also, a decrease in testosterone concentration affects the psycho-emotional state of a man, leading to depressed mood, blues, and depression.
Clinical picture
The clinical picture of the disease depends on the time of occurrence of the disorder and is presented in Table 1.
Table 1. Main signs of hypogonadism
There are nonspecific signs that may lead a clinician to suspect hypogonadism:
- oligo- and azoospermia;
- pathological fractures (discrepancy between the strength of the traumatic factor and the severity of the injury);
- osteopenia;
- moderate anemia (normochromic, normocytic);
- increase in adipose tissue;
- depression, sleep disturbance, memory loss.
Diagnosis of hypogonadism
The diagnosis of hypogonadism in men is established on the basis of anamnesis, clinical picture, confirmed by laboratory and instrumental studies. Recent guidelines recommend that the diagnosis of hypogonadism should be made only in men with symptoms, external manifestations, and clearly reduced serum testosterone levels [2]. However, an analysis of the level of morning total testosterone in serum is recommended as an initial diagnostic test for hypogonadism.
Figure 2-3. Different types of hypogonadism
To calculate the level of free testosterone, you can use the online calculator www.issam.ch/freetesto.htm.
Table 2. Testosterone standards
If necessary, determine the levels of SSSH, FSH, LH, prolactin. High risk factors for developing hypogonadism:
- space-occupying formations of the hypothalamic-pituitary region;
- surgical interventions and/or radiation in the area of the sella turcica;
- long-term use of glucocorticoids, ketoconazole, opioids;
- diabetes mellitus, infertility, osteopenia and osteoporosis.
General population screening is not practical [3].
To identify a group at risk of hypogonadism, specialized questionnaires can be used.
How to increase testosterone levels when they are low
Medications prescribed as part of hormone replacement therapy (HRT) can help with this problem. With its help, normal levels of testosterone concentration in the blood are achieved and, thereby, the symptoms of its deficiency are eliminated.
You can undergo all the necessary tests to determine the level of testosterone and other substances related to it in a medical office. A competent urologist-andrologist will prescribe the necessary laboratory tests and interpret their results during the consultation. In case of any violations, an individual drug treatment regimen will be developed for the patient, taking into account indications and contraindications. Only a specialist can prescribe effective therapy that will not cause harm.
Andrologist in Lipetsk: +7 (4742) 90-40-50, and you can also make an appointment online
Treatment of hypogonadism in men
When starting to treat hypogonadism, the doctor sets a number of goals:
- elimination of androgen deficiency (restoration of potency, libido, well-being and behavior);
- ensuring virilization (growth of hair on the face and body according to the male type, change in voice timbre, physique, increase in muscle mass, enlargement of the penis and testicles, pigmentation of the scrotum, development of folding), if possible, ensuring fertility;
- potentially - reducing cardiovascular risks, preventing osteoporosis.
Depending on whether it is necessary to restore fertility, the choice of therapy is between hormone replacement therapy (HRT) with testosterone preparations, on the one hand, and preparations of human chorionic gonadotropin (hCG), luteinizing hormone (LH), follicle-stimulating hormone (FSH) and gonadotropin- releasing hormone (GRH) - on the other.
There are a large number of dosage forms of testosterone for intramuscular, subcutaneous, transdermal, oral and buccal use. However, testosterone HRT leads to a decrease in testicular volume and suppression of spermatogenesis.
Therefore, if testicular function is preserved and hypogonadism is of hypothalamic or pituitary origin, either hCG, LH, FSH drugs, or pulsatory administration of GnRH are used. These hormones increase the production of your own testosterone, which leads to the induction of spermatogenesis and restoration of fertility.
Clinical case
Patient K. (39 years old) consulted an endocrinologist with complaints of sexual dysfunction (decreased sexual desire, erectile dysfunction), general weakness, increased fatigue, shortness of breath during exercise, episodes of increased blood pressure (maximum up to 165/100 mm Hg). .), excess weight, ineffectiveness of physical activity and diets.
He said that he follows the principles of rational nutrition and regularly visits the gym. The above complaints have been bothering me for the last year. He was not independently treated or examined. Objectively upon examination:
- height - 183 cm;
- weight - 127 kg;
- BMI - 37.9 kg/m2;
- waist circumference (WC) - 123 cm;
- hip circumference (HC) - 135 cm;
- OT/OB - 0.91;
- Blood pressure - 145/90 mm Hg. Art., heart rate - 82 beats per minute.
Hair growth in the armpits, chest, anterior abdominal wall, and groin area is unremarkable. Bilateral false gynecomastia. The external genitalia are formed correctly, without any peculiarities.
When using the ADAM questionnaire, positive answers to 8 out of 10 questions, which indicates the severity of symptoms of androgen deficiency in this patient.
Laboratory indicators:
- total cholesterol - 6.4 mmol/l (normal 3.1–5.2);
- LDL - 3.8 mmol/l (normal 0–3.3);
- triglycerides - 2.6 mmol/l (normal - less than 2.3);
- total testosterone - 7.2 nmol/l (normal 12.0–41.0);
- SSSH - 28.9 pmol/l (normal 12.9–61.7);
- LH - 4.7 U/l (normal 2.5–11.0);
- TSH - 1.8 mU/l (normal 0.25–4.0);
- prolactin - 243 IU/l (normal 50–610);
- estradiol - 164 pmol/l (normal 20–240);
- total PSA - 0.6 ng/ml (normal 0-4).
According to ultrasound of the prostate gland, no echographic signs of pathology were identified.
The patient was diagnosed with normogonadotropic hypogonadism.
Metabolic syndrome: Abdominal obesity (2nd degree). Arterial hypertension. Dyslipidemia. Treatment goals:
Normalization of testosterone levels. A prolonged form of testosterone (testosterone undecanoate 1000 mg) was prescribed intramuscularly according to a regimen with dose titration to maintenance.
Weight loss and maintenance. It is recommended to follow the principles of a balanced diet with limited consumption of fats and easily digestible carbohydrates, table salt, as well as additional aerobic exercise (active walking for 1 hour a day).
When assessing the results of therapy after 10 months, the patient noted significant positive dynamics in general well-being - improvement in erectile function (increased sexual desire, increased frequency of spontaneous erections), disappearance of complaints about fatigue, depressed mood; stabilization of blood pressure to 130/80 mm Hg. Art. Objectively, upon examination, there was a decrease in all anthropometric indicators: weight - 99 kg, BMI - 29.5 kg/m2, WC - 88 cm, WC - 109 cm, WC/WC - 0.81. During treatment, all hormonal and biochemical parameters also normalized. In the future, it was decided to continue therapy with monitoring of laboratory parameters once every six months.
ESTRADIOL
In women, estradiol is produced in the ovaries, placenta and zona reticularis of the adrenal cortex under the influence of FSH, LH and prolactin. Estradiol is formed in small quantities during the peripheral conversion of testosterone. In men, estradiol is formed in the testes, in the adrenal cortex, but most of it is formed in peripheral tissues due to the conversion of testosterone. Estradiol ensures in women the formation of the reproductive system according to the female type, the development of female secondary sexual characteristics during puberty, the formation and regulation of menstrual function, the development of the egg, the growth and development of the uterus during pregnancy. It is also responsible for the psychophysiological characteristics of sexual behavior and ensures the formation of subcutaneous fatty tissue according to the female type. A necessary condition for the effects of estradiol to occur is the correct relationship with testosterone levels. Estradiol has an anabolic effect, enhances bone turnover and accelerates the maturation of skeletal bones; promotes sodium and water retention in the body, reduces cholesterol levels and increases blood clotting activity. Daily fluctuations in the concentration of estradiol in the serum are associated with the rhythm of LH (luteinizing hormone) secretion: the maximum occurs between 15 and 18 hours, and the minimum between 24 and 2 hours. In women of childbearing age, the level of estradiol in the blood serum and plasma depends on the phase of the menstrual cycle. cycle. The highest levels of estradiol are observed in the late follicular phase. During pregnancy, the concentration of estradiol in serum and plasma increases at the time of delivery, and after delivery it returns to normal on the 4th day. With age, women experience a decrease in estradiol concentrations. During postmenopause, the concentration of estradiol decreases to the level observed in men. Indications for the purpose of the analysis: diagnosis of disorders of the menstrual cycle and fertility (ability to produce offspring) of women, amenorrhea, oligomenorrhea, anovulation, hypogonadism, disorders of puberty, osteoporosis (in women), hirsutism, infertility, premenstrual syndrome, signs of feminization in men. An increase in estradiol levels is observed with hyperestrogenism; endometrioid ovarian cysts; tumors of the ovaries, testicles, liver cirrhosis, pregnancy, taking hormonal drugs. Estradiol levels are reduced during intense physical activity in untrained women, with significant weight loss, a high-carbohydrate, low-fat diet, in vegetarians, and in early pregnant women who smoke; for chronic inflammation of the internal genital organs, chronic prostatitis, insufficiency of the gonads and other conditions. Preparation for the study: on the eve of the study, avoid physical activity (sports training) and smoking. In women, the analysis is performed on days 6-7 of the menstrual cycle, unless other dates are indicated by the attending physician.