How to recognize acute bronchitis
The main symptom of acute bronchitis in adults is a cough, which occurs as a response of the body to an irritant and a desire to restore patency of the airways. On average, it lasts 2-3 weeks, accompanied by other signs of colds. Cough with bronchitis changes its character over time. At first it is dry, intrusive, sometimes even annoying, debilitating. As the disease progresses, it gradually becomes wet (productive). At this moment, a protective mechanism is launched: the cells of the bronchial mucosa begin to actively produce sputum, and with it, during a wet cough, various pathogenic agents, primarily viruses and bacteria, are removed from the body. The color and consistency of sputum, among other things, can tell the doctor the cause of the disease and, therefore, the optimal treatment regimen.
In addition to coughing, bronchitis may be accompanied by symptoms such as:
- weakness, feeling of weakness, fatigue;
- increased body temperature;
- runny nose;
- sweating;
- headache;
- chest pain;
- shortness of breath (in severe cases of the disease).
The symptoms of acute bronchitis in children are the same as in adults, but may be more pronounced.
Bronchitis. Causes. Diagnostics. Treatment.
Acute bronchitis is a diffuse acute inflammation of the bronchial mucosa and bronchial tubes. Refers to common diseases.
Etiology, pathogenesis.
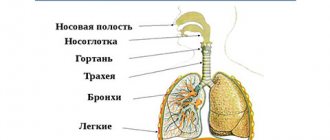
The disease is caused by viruses ( influenza viruses ( including COVID-19)
, parainfluenza, adenoviruses, respiratory syncytial, measles, pertussis, etc.), bacteria (staphylococci, streptococci, pneumococci, etc.); physical and chemical factors (dry, cold, hot air, nitrogen oxides, sulfur dioxide, hypothermia, etc.). The damaging agent penetrates the nasopharynx, and then into the trachea and bronchi with inhaled air, hematogenously or lymphogenously (uremic bronchitis). Acute inflammation of the bronchial tree may be accompanied by a violation of bronchial patency due to an edematous-inflammatory or bronchospastic mechanism.
In severe forms, the inflammatory process affects not only the mucous membrane, but also the deep tissues of the bronchial wall.
Factors predisposing to the occurrence of the disease.
Bronchitis of infectious etiology often begins against the background of acute rhinitis, laryngitis, and influenza.
- with a mild course of the disease, there is rawness behind the sternum, a dry, less often wet cough, a feeling of weakness, and weakness. - body temperature is subfebrile (37.2º-37.5º) or normal.
This course is observed more often with damage to the trachea and large bronchi.
In moderate cases, the following are significantly pronounced:
- general malaise,
- weakness,
- characterized by a severe dry cough with difficulty breathing and shortness of breath,
- sweating,
- pain in the lower chest and abdominal wall associated with muscle strain when coughing.
The cough gradually becomes wet, the sputum becomes mucopurulent or purulent in nature.
The body temperature remains low-grade or high for several days.
A severe course of the disease is observed, as a rule, with predominant damage to the bronchioles. With this form of the disease, such changes are reversible. The disease cannot be started, because bronchitis can become chronic when there is a possibility of a severe course of the disease with severe obstruction and destructive tissue changes that are irreversible.
Diagnosis of bronchitis
Diagnosis is carried out through examination by a doctor, CT scan of the lungs, fluorography and blood and saliva tests.
Treatment of bronchitis
- bed rest, plenty of warm drinks with honey, raspberries, linden blossom;
- bronchodilators;
- expectorants;
- inhalation of expectorants, mucolytics, heated mineral alkaline water, 2% sodium bicarbonate solution, eucalyptus, anise oil using a steam or pocket inhaler;
- antibacterial therapy.
Chronic bronchitis is a diffuse progressive inflammation of the bronchi, not associated with local or generalized lung damage and manifested by cough. It is customary to speak of the chronic nature of the process if the cough continues for at least 3 months. in 1 year for 2 consecutive years. Chronic bronchitis is the most common form of chronic nonspecific lung diseases (CNLD), which tends to become more frequent.
Etiology, pathogenesis.
The disease is associated with prolonged irritation of the bronchi by various harmful factors (smoking, inhalation of air contaminated with dust, smoke, carbon monoxide, sulfur dioxide, nitrogen and other chemical compounds) and recurrent respiratory infection (the main role belongs to respiratory viruses, Pfeiffer's bacillus, pneumococci), less commonly occurs in cystic fibrosis.
Symptoms and course of the disease.
The beginning is gradual. The first symptom is a cough in the morning with mucous sputum. Gradually, the cough begins to occur both at night and during the day, worsening in cold weather, and becomes constant over the years. The amount of sputum increases, it becomes mucopurulent. Shortness of breath appears and progresses. Often difficulty breathing, feeling of lack of air.
There are 4 forms of chronic bronchitis:
- a simple, uncomplicated form of bronchitis occurs with the release of mucous sputum without bronchial obstruction;
- purulent bronchitis, purulent sputum is constantly or periodically released, but bronchial obstruction is not expressed;
- obstructive chronic bronchitis is characterized by persistent obstructive disorders.
- Purulent-obstructive Bronchitis occurs with the release of purulent sputum and obstructive ventilation disorders.
During an exacerbation of any form of chronic bronchitis, bronchospastic syndrome may develop. Frequent exacerbations are typical, especially during periods of cold, damp weather: cough and shortness of breath intensify, the amount of sputum increases, malaise, sweating, and fatigue appear. Body temperature is normal or subfebrile.
Treatment:
In the phase of exacerbation of chronic bronchitis, therapy should be aimed at eliminating the inflammatory process in the bronchi, improving bronchial patency, and restoring impaired general and local immunological reactivity.
- prescribe antibiotics and sulfonamides in courses sufficient to suppress the activity of the infection;
- expectorants, mucolytic and bronchospastic drugs, drinking plenty of fluids;
- if allergic syndromes occur, calcium chloride is prescribed orally and intravenously, and antihistamines.
Patients need systematic maintenance therapy, which is carried out in outpatient treatment courses. The goal of therapy is to combat the progression of pulmonary heart failure, amyloidosis and other possible complications of the disease.
A pulmonologist will diagnose and select the correct treatment.
Why are our pulmonologists better than others?
- The knowledge and experience of the doctors at our clinic allow us to achieve amazing success in the treatment of bronchitis.
- The Health Clinic has the most modern diagnostic equipment, which allows you to make an accurate diagnosis and begin treatment.
- Location in the very center of Moscow, within walking distance of two metro stations.
- Attractive prices
- Convenient time to visit a doctor.
We work to keep you healthy.
Make an appointment by phone: +7(495) 961-27-67
Track. article
Prev. article
Causes of acute bronchitis
The cause of acute bronchitis in adults in the vast majority of cases is an infection: most often viral, less often bacterial, and occasionally fungal. In addition, the disease can be of an allergic nature (due to a high concentration of allergen in the air), develop in the presence of inflammation of the adenoids or chronic foci of infection in the paranasal sinuses, against the background of tonsillitis.
It is worth considering factors that reduce local immunity and contribute to the occurrence of the disease:
- hypothermia;
- smoking;
- alcohol abuse;
- hereditary diseases;
- chronic pathology of the nasopharynx;
- unfavorable climate (dampness, cold);
- air polluted with dust or toxic impurities.
Causes of bronchitis
Acute infectious bronchitis most often occurs in children; its cause is viruses (influenza, parainfluenza, measles, respiratory syncytial virus, etc.). Less commonly, the causative agent of infection is bacteria (staphylococcus, pneumococcus, streptococcus, etc.), they are usually associated with a viral infection.
Non-infectious bronchitis occurs more often in adults; it develops against the background of:
- inhalation of smoke, dust, toxic gases;
- exposure to hot steam or very cold air;
- living in unfavorable climatic conditions;
- allergic reactions.
The cause of chronic bronchitis is most often the combined effect of infections, non-infectious factors and a weakening of the body's defenses.
Very often, chronic inflammation of the bronchi occurs after acute:
- in smokers;
- in persons who abuse alcohol;
- for those working in hazardous industries: in the mining industry, in contact with dust containing cadmium and silicon, miners, builders in contact with cement, workers in the metallurgical and pulp and paper industries, railway workers, workers involved in grain and cotton processing;
- in patients with concomitant diseases (for example, heart disease, chronic nasopharyngeal infections).
Types of acute bronchitis
Depending on the nature of the inflammation, acute bronchitis can be:
- catarrhal (accompanied by an increased amount of bronchial mucus);
- fibrinous (with the formation of thick, sticky and difficult to separate sputum);
- mucopurulent/purulent (with copious amounts of mucus and discharge of pus);
- hemorrhagic (with streaks of blood in the sputum due to hemorrhages in the bronchial mucosa in severe forms of the disease).
According to the prevalence of the inflammatory process, acute bronchitis in adults is usually divided into focal, in which inflammation is localized in a limited area of the bronchi, and diffuse, covering most of the bronchial tree.
How to treat acute bronchitis
When the first signs of the disease appear (if no more than 48 hours have passed since its onset), antiviral drugs may be prescribed. Treatment of acute bronchitis with antibiotics is usually not practiced. It can be justified only if whooping cough is suspected and bacterial complications are confirmed. How to treat acute bronchitis in the presence of an intense cough? In this situation, to reduce the risk of side effects, the mechanism of action of the drug and the presence of contraindications should be taken into account. For a dry hacking cough, antitussives can be used. When coughing is accompanied by the discharge of viscous sputum, mucolytics are prescribed to improve the discharge of mucus from the respiratory tract. You can rely on herbal preparations, such as cough medicines Doctor MOM®.
There are also general recommendations that are relevant for the treatment of acute bronchitis of any nature:
- compliance with bed or semi-bed rest (depending on the patient’s condition);
- consumption of large amounts of warm fortified liquid (up to 2–2.5 liters per day). However, you should avoid drinks containing caffeine and alcohol, as they dehydrate the body and worsen inflammation. Decoctions of rose hips, raspberries and linden blossoms, fruit drinks and heated mineral water will bring benefits;
- to give up smoking;
- protecting the patient from irritating factors: dust, smoke, strong odors and toxic fumes;
- regular ventilation of the room and maintaining an optimal level of humidity in it (50-70%). To humidify the air, you can use both special climate control devices and improvised means, for example, a wet towel hung on a radiator.
In acute bronchitis, mucolytic agents are used to treat cough and facilitate mucus discharge, which thin the mucus and facilitate its removal. For example, you can use Doctor MOM® herbal cough syrup, which contains extracts of 10 medicinal herbs and has a complex effect: secretolytic (increases the secretion of protective mucus), mucolytic (reduces the viscosity of sputum), expectorant (removes phlegm), bronchodilator (relaxes the bronchi) and anti-inflammatory . The syrup is suitable for adults and children over 3 years of age. Ignoring the symptoms and inadequate treatment of acute bronchitis in adults can lead to the disease becoming chronic and the development of very serious complications.
The best medicine for bronchitis
Research has found that bronchitis most often affects people with weakened immune systems and those exposed to significant risk factors.
The risk of disease is reduced if you follow a balanced diet that provides the body with essential nutrients - proteins, fats, carbohydrates, minerals and vitamins. Their deficiency weakens the body's protective functions. An active, mobile lifestyle also increases resistance to respiratory diseases.
Figure 4 - The best cure for bronchitis is exercise
Bronchitis is often caused by viral infections. Vaccination helps to significantly reduce the risk of infection by viruses. Some vaccinations are given during childhood, while others are seasonal, such as the flu vaccine, which is given before the highest flu season. Even if a vaccinated person gets sick, in this case the disease is much milder and does not cause consequences.
Quitting smoking and alcohol abuse, which suppresses the effect of certain vitamins, disrupts metabolism, impairs heat exchange, also has a beneficial effect on the prevention of bronchitis and other respiratory diseases.
Video: School of Doctor Komarovsky. About bronchitis.