Rabies is a viral infection that causes severe and progressive damage to the brain and spinal cord. It is worth understanding that rabies is a deadly disease if measures are not taken in time.
Previously, regarding this infection, there was an opinion that it could be treated if, immediately after the pathogen entered the human blood, 40 injections were given to him in the stomach. It was these 40 injections that were always the main horror story for everyone, especially for children who constantly played with street and street animals. Moreover, they usually said that these injections were extremely painful.
Article on the topic Worms, rabies, bacteria. What can you get infected from a dog?
The essence of the disease
Rabies is present in almost all countries, with the only exceptions being Japan, New Zealand, Great Britain, Australia and Antarctica. The source in 99% of cases is dogs, foxes, bats, wolves, cats and small rodents.
The disease is transmitted by a bite or salivation; aerosol transmission is less likely. As doctors note, more often we are talking about the transmission of the virus through saliva from an infected animal.
The incubation period ranges from 10 days to 3 months, it all depends on where the person was bitten. The disease will take longer to develop if bitten on the limbs or torso. The development of pathology occurs in several stages. Among the first signs of rabies in humans are itching, discomfort, pain in and around the bite site. An increase in temperature, sweating, loss of appetite, and a feeling of tightness in the chest area are also possible. Insomnia, increasing anxiety, and melancholy add to the problem. In addition, increased sensitivity to light, sounds, etc. develops. One of the most striking symptoms is called hydrophobia, when even when thinking about water (especially when trying to drink), a convulsive syndrome begins. The result of the disease is paralysis and death.
Be careful, evil crow! How I got the rabies vaccination Read more
Conquering rabies
Alexey Vodovozov, doctor, scientific editor of the ABC medical magazine
“Popular Mechanics” No. 12, 2012
Even 150 years ago, a person bitten by a rabid animal was doomed. Today, scientists are improving weapons in the war against an ancient and extremely dangerous enemy - the rabies virus.
Know the enemy by sight
The causative agent of rabies ( Rabies virus
) belongs to the family of rhabdoviruses (Rhabdoviridae), containing a single-stranded linear RNA molecule, genus
Lyssavirus
. In shape it resembles a bullet with a length of about 180 and a diameter of 75 nm. Currently, seven genotypes are known.Rabies virus under a transmission electron microscope (36,700x magnification). In the computer image in red
the protein shell of the virus is shown - the capsid, and
in yellow
- the additional lipoprotein shellInsidious virus
The rabies virus has tropism (affinity) for nervous tissue, just as influenza viruses have affinity for the epithelium of the respiratory tract. It penetrates the peripheral nerves and moves at a speed of approximately 3 mm/h to the central parts of the nervous system. Then, through a neurogenic route, it spreads to other organs, mainly to the salivary glands.
The likelihood of the disease depends on the location and severity of the bites: when bitten by rabid animals on the face and neck, rabies develops on average in 90% of cases, in the hands - in 63%, and in the thighs and arms above the elbow - only in 23% of cases.
Sources of infection
The main wild animals - sources of infection - are wolves, foxes, jackals, raccoon dogs, badgers, skunks, and bats. Among domestic animals, cats and dogs are dangerous, and it is the latter that account for the maximum number of confirmed cases of rabies transmission to humans. Most sick animals die within 7–10 days, the only exception described is the yellow fox-shaped mongoose Cynictis penicillata
, capable of carrying the virus without developing a clinical picture of infection for several years.
The most characteristic and reliable sign of the presence of a virus in a human or animal body is the detection of so-called Negri bodies, specific inclusions in the cytoplasm of neurons with a diameter of about 10 nm. However, in 20% of patients Negri bodies cannot be found, so their absence does not exclude the diagnosis of rabies.
The first, but extremely important step towards the fight against rabies was taken by the brilliant French chemist and microbiologist Louis Pasteur. He began developing a vaccine against this disease in 1880, after he had to observe the agony of a five-year-old girl bitten by a rabid dog.
Rabbits and dogs
Although rabies was first described in the 1st century BC. Roman Cornelius Celsus, almost 2000 years later, very little was known about this disease. It was not until 1903, eight years after Pasteur's death, that the French physician Pierre Remlenger discovered that rabies was caused by a submicroscopic life form - a filterable virus.
How viruses reproduce
To enter a cell, the rabies virus uses the endosomal transport system: the cell itself must capture it and draw the vesicle formed from the cell membrane - the endosome, the “inner body” - into the cytoplasm. Activation of this process occurs after the virus binds to special receptor proteins on the cell membrane. The resulting endosome disintegrates over time, the viral particle releases RNA, and then everything goes according to the standard scenario.
Pasteur, without this information, was nevertheless not going to give up: to create a vaccine, he chose a workaround - to find a container for the “poison” and turn it into an antidote. It was reliably known that something transmitted from a sick animal to another animal or person along with infected saliva affects the nervous system. During the experiments, it was found that the disease had a very long incubation period, but this only spurred Pasteur and his colleagues, since it meant that doctors had the opportunity to influence the slowly developing pathological process - the “poison” needed to reach the spinal nerves through the peripheral nerves. , and then the brain.
Then experiments began on rabbits in order to obtain the most lethal rabies “poison” in large quantities. After dozens of transfers of brain tissue from a sick animal to the brain of a healthy one, from that to the next, etc., scientists managed to achieve that a standard extract from the brain killed a rabbit in exactly seven days instead of the usual 16–21. Now it was necessary to find a way to weaken the rabies pathogen (the method of creating vaccines - weakening the pathogen - was also Pasteur’s discovery). And they found a way: drying rabbit brain tissue soaked in the virus for two weeks over moisture-absorbing alkali.
After administering a suspension of the resulting drug, the dog infected with rabies not only recovered, but also became completely immune to rabies, no matter how much “poison” was injected into it.
Viruses and bacteria
Doctors fight bacterial infections quite successfully. It's not that simple with viruses.
Fickle Enemy
Antibiotics and vaccines are doing their job, and sanitation and epidemiology are excellent. Viruses are much more difficult to fight. Suffice it to recall the flu, which the world's population suffers from with enviable regularity, despite all the achievements of science and the availability of vaccines and antiviral drugs.
This is primarily due to the ability of viruses to change in the most unpredictable ways. Some, like influenza pathogens, change the proteins of their shell like gloves, so it is still not possible to develop high-precision weapons against them.
In the fight against diseases, success came when a weak double was discovered in the virus, which did not kill a person, but left behind powerful cross-immunity. Deliberate infection with a weaker strain made it possible to protect against a deadly one. The classic case from which the history of vaccination began is natural and cowpox, then a similar story was repeated with polio. In the summer of 2012, there was hope that a similar scenario would help control rabies.
Plant viruses
Plant viruses were first described in 1892 by the Russian scientist D.I. Ivanovsky. He called them “bacteria that pass through the Chamberland filter, which, however, are not able to grow on artificial substrates.” The term “filterable virus” (lat. virus)
- poison) appeared in 1898, a year after the isolation of the foot-and-mouth disease virus - a disease of cattle, and the first virus causing a human disease - yellow fever - was discovered in 1901.
Having finally made sure that vaccinated dogs were not affected by the same seven-day laboratory “poison,” the researchers conducted a cruel experiment: they introduced their rabid relatives to the vaccinated dogs. The bitten mongrels did not get sick!
40 injections in the stomach
Then it was the people's turn. But where to find volunteers? Driven to despair, Pasteur was ready to sacrifice himself for the sake of science, but, fortunately, His Majesty Chance intervened.
On July 6, 1885, a tearful woman appeared on the threshold of Pasteur’s Paris laboratory, holding the hand of her nine-year-old son, Joseph Meister. Three days earlier, the boy was bitten by a rabid dog, inflicting 14 open wounds on him. The consequences were quite predictable: at that time it was already known that death in such cases was almost inevitable. However, the boy's father had heard a lot about Pasteur's work and insisted on bringing the child from Alsace to Paris. After serious hesitation, Pasteur injected the little patient with an experimental drug, and Joseph became the first person in history to be saved from rabies.
From the laboratory diary of Louis Pasteur, 1885
“The death of this child seemed inevitable, so I decided, not without serious doubts and anxiety, which is well understandable, to try on Joseph Meister the method that I had found successful in treating dogs. As a result, 60 hours after the bites, in the presence of doctors Villepeau and Grandchet, young Meister was vaccinated with half a syringe of an extract from the spinal cord of a rabbit that died of rabies, previously treated with dry air for 15 days. I made a total of 13 injections, one every day, gradually introducing an increasingly lethal dose. Three months later I examined the boy and found him completely healthy.”
People from all over the world flocked to Paris - Algerians, Australians, Americans, Russians, and often they knew only one word in French: “Pasteur”. Despite such success, the discoverer of a vaccine against a deadly disease had to hear the word “killer” addressed to him. The fact is that not all those bitten survived after vaccination. In vain Pasteur tried to explain that they contacted too late - some two weeks after the animal attack, and some even a month and a half later. In 1887, at a meeting of the Academy of Medicine, colleagues directly accused Pasteur of simply killing people with pieces of rabbit brains. The scientist, who devoted all his strength to science, could not stand it - on October 23 he suffered a second stroke, from which he never recovered until his death in 1895.
Pasteur's legacy
On the memorial plaque of the house in which Pasteur's first laboratory was located, his discoveries are listed: the enzymatic nature of fermentation, the refutation of the hypothesis of the spontaneous generation of microorganisms, the development of ideas about artificial immunity, the creation of vaccines against chicken cholera, anthrax and rabies. Pasteurization and other “little things” were not included in this list
But ordinary people supported him. By subscription, over a year and a half, residents of many countries around the world collected 2.5 million francs, with which the Pasteur Institute was created, officially opened on November 14, 1888. On its territory there is a museum and tomb of the researcher who saved humanity from a deadly infection. The date of Pasteur's death, September 28, was chosen by the World Health Organization (WHO) for the annual World Rabies Day.
For a long time, the vaccine was administered under the skin of the anterior abdominal wall, and up to 40 injections were required to complete the full course. A modern immunotherapy drug is administered intramuscularly into the shoulder; six visits to the emergency room are sufficient.
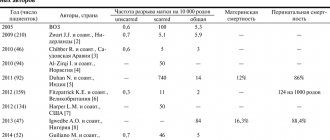
Milwaukee Miracle
During the 20th century, the situation with rabies was clear: if the victim was not vaccinated on time or did not receive the vaccine at all, the matter ended tragically. According to WHO estimates, 50–55 thousand people die every year in the world after attacks by rabid animals, 95% of them occur in Africa and Asia.
The possibility of fully treating the infection was only discussed in the 21st century. This was connected with the case of American Gina Gies, who for the first time in the history of medicine did not receive a vaccine, but survived after the onset of rabies symptoms. On September 12, 2004, 15-year-old Gina caught a bat that bit her on the finger. The parents did not consult a doctor, considering the wound to be trivial, but after 37 days the girl developed a clinical picture of infection: a rise in temperature to 39°C, tremors, double vision, difficulty speaking - all signs of damage to the central nervous system. Gina was referred to Children's Hospital of Wisconsin, and to the laboratories of the Centers for Disease Control and Prevention .
, CDC) in Atlanta confirmed rabies.
The parents were offered to try an experimental treatment method on the girl. Having received consent, doctors used ketamine and midazolam to put the patient into an artificial coma, essentially turning off her brain. She also received antiviral therapy with a combination of ribavirin and amantadine. Doctors kept her in this condition until her immune system began to produce enough antibodies to cope with the virus. This took six days.
A month later, tests confirmed that there was no virus in the girl’s body. Moreover, brain functions were minimally impaired - she graduated from school, and a year later received a driver's license. Currently, Gina has graduated from college and intends to continue her studies at the university. It is not surprising that she sees biology or veterinary medicine as her future profession, and plans to specialize in the field of rabies.
The treatment protocol that was used on the girl was called the “Milwaukee” or “Wisconsin” protocol. They have repeatedly tried to reproduce it in other medical institutions... but, alas, without much success. The first version of the protocol was tested on 25 patients, of which only two survived. The second version, which removed ribavirin but added drugs to prevent vasospasm, was used in ten patients and prevented the death of two of them.
During epidemiological investigations, it turned out that patients who were cured using the Milwaukee Protocol were bitten by bats. It is this fact that has allowed some scientists to suggest that in fact the treatment method has nothing to do with it, but the point is precisely in these mammals, or rather, in the fact that they are infected with a different strain of the virus, less dangerous to humans.
The Bat Riddle
In 2012, this assumption received the first confirmation. In American Journal of Tropical Medicine and Hygiene
an article appeared by a group of CDC experts, American military virologists and epidemiologists from the Peruvian Ministry of Health. The results of their research produced the effect of a bomb exploding: in the Peruvian jungle they were able to discover people who had antibodies to the rabies virus in their blood. These people have never been given any vaccines, moreover, they don’t even remember being sick with anything serious. This means that rabies is not 100% fatal!
“From this area of the Peruvian Amazon jungle, there have been numerous reports of exposure to vampire bats and cases of rabies in humans and domestic animals over the past 20 years,” lead study author Dr. Amy Gilbert, who works in the CDC's Rabies Research Program, explains to PM. . “The villages and farms that we examined are located in places very remote from civilization—the nearest hospital, for example, is two days away, and in some areas movement is only possible by boats on water.”
In a survey of residents, 63 out of 92 people reported bat bites to scientists. Blood samples were taken from these people, as well as from local vampire bats. The test results were unexpected: seven samples contained antibodies that neutralize the rabies virus.
The presence of antibodies could be explained by the administration of anti-rabies (lat. rabies
- rabies) vaccine, but, as it turned out, only one in seven people received such a vaccine. The rest suffered from rabies not only without death, but even without any serious symptoms. In two Peruvian villages, more survivors of this infection were found than described in the entire medical literature! Not surprisingly, Gilbert's group spent two years rechecking their findings before deciding to publish them.
“It is likely that there is a unique set of circumstances where the local population is regularly exposed to a particular non-lethal strain of the rabies virus,” says Dr Gilbert. “In this case, natural vaccination occurs, which is confirmed by fairly high titers of antibodies. However, this still requires additional confirmation and clarification.”
Her point of view is shared by her Russian colleagues. Virologist Alexander Ivanov from the Laboratory of Molecular Bases of Action of Physiologically Active Compounds, Institute of Molecular Biology named after. V.A. Engelhardt, whom PM asked to comment on the discovery of CDC experts, emphasized that these results, strange at first glance, may have a completely scientific explanation: “Based on the available data, it can be assumed that local residents were infected with variants of the virus, which in a number of ways causes had low replicative activity (the ability to reproduce) and low pathogenicity (“toxicity”). In my opinion, this may be due to several factors. First, each virus has a huge number of variants due to its relatively high variability. Infectious disease experts suggest that even for a successful transition from bats to other species, the rabies virus must undergo several specific mutations. If this is true, then many strains of the virus carried by bats may be of little danger to humans. Secondly, mutations in the genome of the virus affect its recognition by the immune system, as well as the ability of the virus to block the immune response to infection. At the same time, it is those variants of the rabies virus that are able to evade the innate immune system that have increased pathogenicity. Thus, these facts really suggest the existence in the bat population of such strains of the rabies virus that are promptly recognized and destroyed by the human immune system without causing fatal consequences.”
But in no case - this is emphasized by all experts, including the authors of the study - should one refuse to administer an anti-rabies vaccine when bitten by wild animals. Firstly, it may indeed turn out that another version of the virus lives in bats, a weaker one, and the luck of Peruvian peasants does not extend to strains transmitted by dog or raccoon bites. Secondly, the results and conclusions of this study may turn out to be erroneous, so there is no point in taking further risks.
How to cope with pathology
Today, more progressive methods are used to treat rabies than twenty years ago. For example, the vaccine has become smaller in scale. “For rabies, the CoCAV vaccine is administered. It is administered if there was salivation or a bite from an unknown animal, as well as if a person was bitten by a known animal, which then died within 10 days. If the animal that bitten is vaccinated, then, in principle, you can simply observe it and the person does not need to be vaccinated. This vaccine is given on the first, third, seventh, fourteenth, thirtieth and ninetieth days,” says Sofia Rusanova, an infectious disease doctor at Infectious Diseases Clinical Hospital No. 1.
Article on the topic
Dogs can be biters. How to insure yourself against rabies
Modern rabies vaccination is considered an effective remedy; it is presented in the form of powder for injection. The drug is administered intramuscularly. This vaccination should be given to those who often come into contact with wild animals, and also work with sick four-legged animals, for example, veterinarians. In some cases, such a vaccine is given when a person has scratches or bites made by a sick animal, when the animal’s saliva comes into contact directly with the human mucosa, if the animal that bit the person died after a few days, if the wounds were caused by a wild animal. Particular attention should be paid to this issue.
If the vaccination is done for preventive purposes, and the person has completed all treatment regimens, then the effect will last 3 years. After vaccination, a number of certain rules must be followed. So, you should not drink alcohol in any form or quantity, otherwise nervous attacks, epilepsy, and increased sensitivity to external stimuli are possible. Also, during the first day you should not come into contact with water and care should be taken to ensure that there is no overheating or hypothermia. You should also avoid prolonged exposure to direct sunlight.
When dealing with animals, especially unfamiliar ones, you should understand which bites are the most dangerous. “The most dangerous bites are on the hands, face, neck, and stomach. Everything that is close to the solar plexus. But there is no such thing as “dangerous” or “safe.” All this is very dangerous, since rabies cannot be treated, it can only be prevented. In some cases, rabies immunoglobulin is also administered in addition to the vaccine. Especially if these are dangerous bites,” says Sofia Rusanova.
How do you know if your cat or dog has rabies? More details
Consequences of ignoring doctors' recommendations
The duration of the effect of any vaccine on health and the body is a 10-day period. In the process of exposure to such solutions, there is a possibility of any side effects. Traditionally, the consequences are as follows:
- gastric problems (nausea, vomiting, diarrhea, flatulence, pain),
- allergic reactions (rash, swelling, itching, hyperemia),
- headache and dizziness, migraine and other manifestations of weakness;
- apathy, drowsiness, increased aggressiveness and other mental disorders and abnormalities.
If a patient begins to combine rabies injections and alcohol, he risks experiencing increased symptoms of this phenomenon. Thus, an exacerbation of any chronic diseases may occur, and general weakness and malaise may appear. Or, conversely, alcoholic drinks will mask the dangerous manifestations of the disease and will interfere with timely diagnosis and treatment.
Precautionary measures
In order not to worry about the consequences, it is better to prevent the development of the disease. “Under no circumstances should you touch any hedgehogs, foxes or other animals running past. And if we take animals to the country, we need to vaccinate them. Cat, dog, rabbits and other pets. All warm-blooded animals should be vaccinated. Only snakes and other reptiles do not get rabies. And it is important to understand that after vaccination you cannot immediately go to the country with the animal, since the protective level in animals is formed no earlier than 14 days after vaccination. You will have to stay at home with animals to develop immunity,” says the infectious disease specialist.
Therefore, it is worth calculating and thinking through everything in advance in order to avoid infection, because the price of the issue is life. And not only the pet, but also your own, because any infection that enters the body leaves a mark on it.
"40 INJECTIONS IN THE ABDOMEN"
When it comes to rabies, people generally fall into three groups.
Some people know about the disease and understand the consequences. Others have heard something like this and vaguely remember that after being bitten by a stray dog, there are 40 injections in the stomach. And there are those who know nothing about rabies and think that this is a characteristic of people with a bad character. But no one is safe from encountering a rabid animal, and your own life and that of your loved ones may depend on what exactly you know about this disease. First of all, children. They are the ones who strive to pet any cat. Or they are touched by a hedgehog that curls up so funny in the palm of their hand. They hand-feed a squirrel with nuts or chase a fox that has sneaked into their summer cottage.
However, there are also plenty of adults who become familiar with unfamiliar animals. Many people do not even suspect that you can become infected with rabies, even if a sick animal simply licked you.
WHAT NEXT?
The incubation period of the disease is on average 30–50 days. The first stage of rabies begins with general malaise, headache, and a slight increase in body temperature. After a few (1–3) days, the patient enters the second stage – excitement. Restlessness, anxiety and attacks of hydrophobia characteristic of this stage appear, manifested by an unbearable aversion to a glass of water approaching the patient’s lips. At the sight of a glass, the patient experiences a reflexive, sharply painful spasm of the muscles of the larynx and pharynx. No less indicative are the symptoms of aerophobia - laryngopharyngeal spasm from a stream of cold air directed at the patient’s face. Increased salivation is almost always observed. This period usually lasts 2–3 days. Then the third stage of the disease begins, the beginning of which is characterized by calmness - fear and attacks of hydrophobia disappear. After an imaginary improvement, body temperature rises sharply to 40–42°C, paralysis of the limbs, impaired consciousness and convulsions occur. Death occurs from paralysis of the respiratory muscles or cardiac arrest. Thus, the total duration of clinical manifestations lasts from 3 to 7 days. In some cases, all this may not happen, and the disease very quickly progresses to the stage of paralysis (death occurs within 24 hours after the first manifestations).
Answers to some frequently asked questions
Very often, patients ask doctors about the effectiveness of the vaccine, its compatibility with other drugs and alcohol, as well as adverse reactions from the body and the rules for administering injections. Among the questions. The ones that most often concern patients include:
- How long is the incubation period of the disease and when will you need to get vaccinated to avoid getting sick? The asymptomatic period of the disease can last from several days to a year. It all depends on the supporting function of the body, the amount of virus that has entered it and the favorable environment for its reproduction. To save yourself from the disease, a person should be vaccinated in the first days after the bite incident. Otherwise, immunization will be ineffective.
- Is there a need for vaccination if a vaccinated dog bites? If the fact of immunization of an animal is documented and it has no symptoms of the disease, then vaccination is not necessary. You just need to treat the wound with an antiseptic and, if necessary, consult a doctor.
- Does a person injured by an unvaccinated domestic cat need vaccination? Doctors insist on vaccinating all people who have suffered from pet bites, regardless of how they were kept, age or breed characteristics.
- A child was bitten by a dog on the street. Should he be vaccinated? Definitely yes! In any case, it is always better to play it safe than to risk the baby’s life.
- Is it necessary to observe post-vaccination quarantine? After vaccination, the patient does not need isolation, but experts prefer to monitor him for another 2 weeks after the procedure. Also, you should not appear in very crowded places due to the risk of infection. Naturally, you should not deny yourself walks, but only if they do not take place in severe frost or heat.
- When can you wash after vaccination? The introduction of an anti-rabies drug does not include a ban on water procedures, with the exception of swimming in natural bodies of water. Since a vaccinated person has a weakened immune system, it is better for him to avoid crowded places.
- Can I drink alcohol after immunization? Absolutely no! Alcohol is not compatible with the vaccine suspension, so after its administration it will not be possible to drink even minimal amounts of drinks containing alcohol. This prohibition arose as a result of the fact that alcohol significantly reduces the likelihood of a full and adequate immune response, since it itself is an immunosuppressant. You should not drink alcohol for 2-6 months after the injection.
- Is course interruption serious? How will this affect the immune system? The established vaccination schedule cannot be interrupted. If this happens, it is important to remember that vaccine therapy is now ineffective. The course can be continued only if a person missed one day. In other scenarios, the patient should consult a doctor.
Read. What are the mandatory vaccinations for employees of educational institutions?
BITES ARE DIFFERENT
The likelihood of an unfortunate outcome from rabies depends significantly on the extent of the infection, since this determines the dose of the virus received and the speed of its spread. For example, biting two fingers increases the risk of disease by about twice as much as when only one finger is bitten. Well, if the whole palm is bitten, then the risk will be even higher.
An equally important factor is the location of the bite. The more nerve endings are affected, the more viruses are introduced, and the “closer” the place is to the brain, the more difficult it is to build a protective barrier. Therefore, the most dangerous bites are on the face or neck, since these places are both well innervated and located very close to the brain. Next come the hands, genitals, feet, shoulders and forearms.
Island of Calm
In terms of combating rabies, the experience of the British is interesting. There is no rabies in England: sick animals were exterminated back in the 20s of the last century, and healthy ones were vaccinated. In addition, owners were prohibited from keeping dogs on chains. In such a situation, the animal is more likely to be bitten by a rabid animal, because it cannot escape. Also, a chained dog is generally more aggressive and bites more often. Since the country is surrounded by water on all sides, animals with hydrophobia cannot reach it. All animals imported into the territory undergo strict quarantine. Sometimes, however, in England bats are found with the rabies virus, so those who often “communicate” with them are vaccinated.
WHAT IS IT?
Rabies is a fatal viral disease of warm-blooded animals, which includes humans. The symptoms are unpleasant and characteristic: hydrophobia, which is why rabies is often called hydrophobia, aerophobia, increased excitability of the patient, sometimes turning into violence.
The main source of infection is the bite of a sick animal. But even “mad” saliva that accidentally gets on damaged skin or mucous membrane is dangerous. Having penetrated the body, the virus strives to enter nerve cells, through which it begins to quickly spread towards the brain and spinal cord.
Rabies carriers are both wild animals (most often foxes, but also wolves, raccoons, badgers, bats, skunks, hedgehogs and even squirrels) and domestic animals (dogs, cats, horses, pigs, small and cattle). Stray dogs are the most dangerous for humans, especially in spring and summer.
The animal becomes “mad” and, therefore, dangerous to others even before the first signs of illness appear. It can be identified by its characteristic signs - excessive salivation and lacrimation, increased excitability and a strange unsteady gait.
Rabies virus (Neuroryctes rabid) belongs to the group of myxoviruses of the Lyssavirus genus of the Rhabdoviridae family. It is unstable in the external environment: it dies when heated to 560C in 15 minutes, when boiled - in 2 minutes. Sensitive to many disinfectants. However, it is resistant to both low temperatures and antibiotics
Mad countries
In terms of the rabies epidemic situation, Vietnam, the Philippines, Laos, India, Indonesia, China, everyone’s favorite Thailand and South America are severe.
I strongly recommend that you get vaccinated against rabies before traveling to these countries! According to the Ministry of Agriculture, in 2014, veterinarians registered 1,964 cases of rabies among animals in our country. Sick:
- 1023 foxes
- 421 domestic dogs
- 316 domestic cats
- 10 ferrets
- 9 martens and arctic foxes each
- 4 each of muskrat and corsac (steppe fox)
- 3 hedgehogs
- 2 bears and a badger each
- 1 boar, rat and hamster
- and some other animals.
Over the past 5 years, 52 people have died from rabies in Russia.
Author: Olga Georginova Published: June 17, 2016
NOT IN ENGLAND, BUT WE HAVE
Some countries do not have rabies at all - for example, Sweden, Norway, Finland, Great Britain, New Zealand, Australia, Ireland and Iceland. But overall, things are worse now than in the middle of the 20th century. The main reason is considered to be an unsuccessful experiment to resettle the raccoon dog in Europe. There were hopes that this predator would displace the more dangerous wolves and foxes. But in fact, it turned out that the raccoon dog is a “company” animal and coexists well with those with whom it was supposed to fight, and tolerates rabies several times better.
In Russia everything is not fun at all. Cases of the disease are recorded every year in Moscow and the Moscow region. According to Regnum news agency, the largest number of identified cases was recorded in the Lipetsk, Belgorod, Tambov, Penza regions and in the Republic of Tatarstan. The situation regarding rabies remains difficult in the Republic of Udmurtia, in the Volgograd, Bryansk and Saratov regions. This is primarily due to the cessation of anti-epidemic measures, which were successfully carried out in the USSR, when meat with a vaccine was scattered in foci of infection so that wolves and foxes, eating meat, would be automatically vaccinated. The growing number of sterilized, but, unfortunately, unvaccinated stray dogs also contributes to the widespread spread of rabies.
RACE RACE, GRAND PRIZE – MOZ
Rabies is a rare case when vaccinations are given not for prevention, but for treatment. The virus travels along the nerves to the brain for quite a long time (about 2 weeks), that is, there is a real opportunity during this time to form immunity with the help of a vaccine. In addition, vaccination can slow the spread of the virus. I note that the likelihood of illness increases sharply with a delay in vaccination: for example, a week’s delay in vaccination increases the likelihood of death by five times!
AND FOR PREVENTION
People at risk (veterinarians, dog handlers, hunters) need to be vaccinated in advance, according to a special scheme, with the first revaccination after 12 months and then every 5 years.
Preventive vaccination for those traveling abroad consists of three doses administered according to a schedule of 0–7–21 (or 28) days. It turns out that if you are vaccinated against rabies, you should do this no later than a month before your trip. This vaccination protects against rabies for three years.
Side effects for all vaccines are approximately the same: swelling and hardening at the injection site, enlarged lymph nodes, general malaise, weakness, headache, sleep and appetite disturbances, fever. Sometimes allergies to vaccine components occur. However, it seems to me that this is still a small price to pay to be alive, healthy and travel to the “crazy” countries of Southeast Asia.
Types of Rabies Vaccines
According to legislative acts, vaccination against a pathological process can be done in almost every medical institution. In rural areas, after contact with a stray animal, it is necessary to contact a rural outpatient clinic or first aid station. In large cities, you can protect yourself from infection in a clinic, emergency room, infectious diseases department, or surgery.
As of today, there are several options for vaccines used against rabies:
- dry inactivated rabies vaccine;
- the domestic vaccine under the trade name “Kokav” is a purified anti-rabies drug from a culture of the pathogen;
- the Indian vaccine “Indirab” is distinguished by its availability;
- the more expensive German vaccine Rabipur;
- Russian vaccine "Kav", containing small doses of an immune solution, and therefore very often used.
In addition to vaccines, the modern market offers patients rabies immunoglobulin as an addition to the main drug. It is highly purified and can be human as well as equine.