Alcohol poisoning is a complex of symptoms of poisoning when the main toxic substance is alcohol and its metabolites. In addition to ethyl alcohol, methyl, butyl, isopropyl and other alcohols, the toxic effect of which, as a rule, is even more pronounced, can enter a person.
First of all, in terms of danger, acute alcohol poisoning should be highlighted, which usually occurs due to an overdose of strong alcoholic beverages or the use of alcohol substitutes. True, when taking alcoholic surrogates, poisoning ceases to be purely alcoholic, since the surrogate used as an alcohol substitute contains, in addition to ethyl alcohol, other poisons - usually methyl alcohol, acetone and others. One of the first places in the statistics of household poisonings is occupied by poisoning with surrogates or low-quality alcohol.
Symptoms of alcohol poisoning
Signs of the toxic effects of alcoholic beverages appear gradually. The severity of symptoms of alcohol poisoning changes in accordance with the increase in the concentration of ethyl alcohol in the blood plasma. Poisoning with alcohol surrogates occupies a leading position in the statistics of all intoxications. Moreover, 98% of patients die before hospitalization. A brief description of the alcohol surrogate will help to understand the reason for such a high mortality rate. What are alcohol surrogates? What are the signs of poisoning with such counterfeit alcohol? How to help the victim? What could be the consequences of such intoxication? We will look at the answers to these questions in this article.
What applies to alcohol surrogates?
Poisoning with alcohol substitutes in the international classification of diseases ICD-10 corresponds to codes T51.1 - T52.9. They are divided into two groups: those alcohol substitutes that may contain ethyl alcohol and those that may not contain it. The first group includes: 1. Butyl alcohol. Death occurs after taking just 30 milliliters. 2. Hydrolysis and sulfite alcohols, which are obtained from wood. They are more toxic than ethanol due to the presence of a small amount of methyl alcohol. 3. Denatured alcohol or technical alcohol. Contains some wood alcohol and aldehyde. 4. Colognes and lotions. They may contain up to 60% ethanol. 5. The polish contains several types of toxic alcohols. 6. The stain, together with ethanol, contains dyes, which cause the patient’s skin and mucous membranes to turn blue.
The second group, or they are also called “false surrogates,” is represented by: • methyl alcohol; • ethylene glycol.
Symptoms of poisoning with surrogates containing ethyl alcohol
Clinically, signs of alcohol intoxication are first observed:
- emotional and motor arousal;
- facial redness;
- state of euphoria;
- sweating;
- increased salivation;
- a feeling of mental and physical relaxation.
Then intoxication gives way to symptoms of alcohol intoxication. The skin becomes pale. There is a frequent urge to urinate. The pupils dilate and the mouth feels dry. Increased mental and physical activity is accompanied by a lack of coordination, movements become sweeping. Concentration becomes reduced, speech is slurred. Criticism of one's words and actions is sharply reduced or completely absent.
Symptoms of methanol (wood alcohol) poisoning
Methyl alcohol is quickly absorbed in the digestive system. About 75% of the absorbed poison is excreted in the breath, the rest in the urine. The lethal dose ranges from 50 to 150 milliliters. The main impact of poisoning falls on the nervous system and kidneys. A psychotropic effect occurs (pathological changes in the psyche) and a neurotoxic effect, accompanied, among other things, by damage to the optic nerves and retina. So, when poisoning with alcohol surrogates containing methanol, the following symptoms occur:
- nausea, vomiting;
- intoxication and euphoria are weakly expressed;
- visual impairment: flickering black dots before the eyes, blurred vision, diplopia (double vision) and even blindness;
- outwardly, in such patients the pupils are dilated and react sluggishly to light;
- 1-2 days after poisoning, pain in the abdomen, lower back, aches in the muscles and joints appear;
- the temperature rises to 38⁰;
- dry skin and mucous membranes;
- low blood pressure;
- interruptions in heart function;
- confusion;
- attacks of excitement accompanied by convulsions;
- As the symptoms increase, the victim falls into a coma and paralysis of the limbs develops.
Etiology and pathogenesis
Pathophysiology
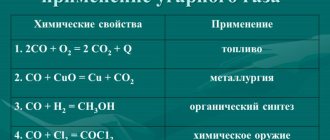
· It is broken down by alcohol dehydrogenase in the liver to formaldehyde and further to formic acid, which is a harmful metabolite.
· Decomposition is slow, about twice as long as ethanol, but faster than formic acid.
· Consequently, it takes 15-20 hours for sufficient formic acid to accumulate to cause hyperventilation (compensation for acidosis) and visual impairment.
Combination of ethanol and methanol
· Both alcohols compete for the same decomposition enzyme, but ethanol has a higher affinity.
· Thus, simultaneous consumption of ethanol will have a positive effect due to the delayed formation of formic acid.
Toxicity
· The most vulnerable structures are the optic nerve and putamen (basal ganglia).
· Consumption of a critical dose causes optic atrophy and/or Parkinson's symptoms, respectively.
· The lethal dose of wood alcohol is up to 1 ml/kg, but this will depend on whether ethanol is taken at the same time.
· If CH3OH is not decomposed, it is excreted unchanged in urine and exhaled air with a half-life of up to 40 hours.
· Folic acid deficiency results in inhibited formic acid degradation.
Symptoms of ethylene glycol poisoning
Ethylene glycol is also quickly absorbed in the digestive tract. About 60% of the poison is broken down in the liver, about 20–30% is excreted by the kidneys. Therefore, it is these organs that will suffer the most, up to the development of their acute failure. In severe poisoning, signs of damage to the nervous system appear. When intoxicated with this alcohol substitute, symptoms develop over periods.
- Early period. It lasts about 12 hours and is characterized by signs of alcohol intoxication while feeling well.
- Toxic damage to the nervous system. There are: nausea, vomiting, headache, thirst, diarrhea, skin and mucous membranes become cyanotic. The pupils are dilated, body temperature rises, difficulty breathing, tachycardia, and psychomotor agitation appear. Loss of consciousness with the development of convulsions is possible.
- The nephro and hepatotoxic period develops 2–5 days from the onset of the disease. A clinical picture of liver and kidney failure is noted. Yellowness of the skin appears, which appears first on the sclera and last of all, the palms turn yellow. Skin itching is characteristic, and darkening of the urine may occur. Renal failure is manifested by a decrease in diuresis up to its absence.
General primary external signs
First of all, motor emotional and arousal arises. As a rule, this is accompanied by liveliness (a characteristic sparkle in the eyes). The initial euphoria is perceived as a pleasant elevation above life's problems. The attitude towards yourself and others changes. This is how a person begins to talk more, and his statements become categorical. When drinking strong drinks, hyperemia (redness) of the skin is observed. This change is usually more pronounced in the upper part of the body, especially on the face; dilation of the pupils is clearly noticeable.
Signs of a mephedrone addict
The following symptoms are typical for a mephidrone addict:
- prolonged insomnia;
- dilated pupils;
- lack of appetite, sometimes for several days;
- deterioration of short-term memory;
- it is difficult for an addict to concentrate on one thing; he can suddenly change the topic of conversation.
At first, the addict manages to successfully hide his new addiction, but very quickly the behavior and appearance of the addict begins to arouse suspicion for the following reasons:
- While on mephedrone, the addict does not want to sleep or eat. If he uses for several days, then his family will clearly suspect something is wrong.
- The addict becomes very active and talkative. He expresses deep interest in each topic, while abruptly jumping from one to another.
- There are also external signs: shiny eyes, a crazy look and dilated pupils. Muscle spasms may begin on the face. Behavior is overly emotional and fussy.
Common secondary signs of poisoning
Subsequently, an increase in the concentration of alcohol when it is absorbed from the stomach into the blood has an increasingly stronger effect on the central nervous system and disrupts the control and regulatory function of the brain. Here symptoms of complete disinhibition are already appearing. A drunk person begins to exhibit instinctive behavior: stupidity appears in judgments, overt sexuality and (or) aggressiveness in behavior. At this same stage of intoxication, awkwardness of movements is observed. Violation of the coordination of motor regulation is caused by the effect of alcohol on the cerebellum. Increased motor activity as ethanol is absorbed quite soon gives way to awkwardness, a “drunk gait” and other characteristic symptoms.
Severe symptoms of poisoning
The vast majority of symptoms of alcohol poisoning are caused by the neurotoxic effects of ethyl alcohol. General toxicity is much less pronounced in the first hours after consumption. That is why the dangerous symptoms of severe poisoning are of a neuroparalytic nature.
Ethanol molecules, due to their minimal sizes relative to other organic compounds, have a unique penetrating ability. So they easily pass the blood-brain barrier. In this case, damage occurs to both the structure of the neocortex and the impact on the centers of the peripheral autonomic nervous system.
Therefore, severe alcohol poisoning is always accompanied by disruption of the vascular and respiratory centers of the central nervous system. With a serious concentration of neurotoxic poison in the body, depressive symptoms from alcohol clearly appear. Outwardly, this easily manifests itself in speech and motor activity. Speech and movements when reaching a severe stage of intoxication become meaningless and incoherent. Therefore, a drunk person, or in fact seriously poisoned by alcohol, is “not able to cope” and can only move by crawling. As alcohol intoxication increases, alcohol stunner quickly develops. A person loses the ability to perceive reality and respond to irritation. Here, in addition to these obvious dangerous symptoms, an alcoholic coma can develop, with all the ensuing consequences.
What types of alcohol surrogates are there?
Alcohol surrogates include various liquids in which, in addition to ethyl alcohol itself, there are other non-food components (BF glue, denatured alcohol, lotions, colognes, hygiene products, etc.), as well as other highly toxic alcohols (wood alcohol, ethanol, antifreeze, ethylene glycol, brake fluid and other technical fluids). Chronic poisoning of the body with alcoholic beverages is usually observed when alcohol dependence is not only already formed, but also progresses. Here you can read about the consequences of constant alcohol abuse, because this is a topic for a separate article.
Pure alcohol from distillation columns is also used for pharmaceutical and medical purposes and is included in many liquids. Therefore, poisoning is possible not only with liquids for technical purposes, but, for example, with sanitary and hygienic products and perfumes. As an illustration of the latter, inexpensive colognes can be mentioned. Although such products cannot be strictly classified as alcohol surrogates, intoxication from them is very similar in symptoms and consequences.
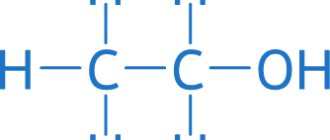
What is methanol and what is the mechanism of its toxic effect on the body?
Methanol is a monohydric alcohol with the chemical formula CH3OH. Widely used in the chemical, gas and pharmaceutical industries, it is part of antifreeze, solvents, glass cleaners, liquid fuels, and gasoline additives. It is a transparent, colorless liquid with a specific odor and taste similar to ethyl alcohol. They can only be distinguished experimentally using hot copper wire. It is immersed in the test liquid. If it is methanol, an unpleasant and pungent odor appears; if it is ethanol, the aroma of rotten apples appears. But it is unlikely that an alcoholic who wants to quickly “improve” his condition will conduct such tests. He will simply drink the obtained “treasure” and thereby doom himself to death. This is the main danger of the substance, since it is difficult to distinguish it from alcoholic beverages by appearance, smell and taste. Even 2% methanol content in the liquid you drink can be toxic. The lethal dose of methanol can vary depending on the individual characteristics of the organism - for one, 30 ml is enough, for another, it can survive even with a much larger amount of methanol taken. There is a known case where a person managed to survive after taking 500 ml of methanol.
For the average person, a dose of 100 ml of methanol is lethal. The lethal concentration in blood plasma is considered to be 1 g/l.
The risk group for methyl alcohol poisoning most often includes chronic alcoholics, into whose bodies it enters due to the use of surrogate drinks or substitution. In addition, persons engaged in the production of products containing methanol, as well as those using methanol-based solvents for washing glass inside cars or closed, small and poorly ventilated rooms, have a significant risk of poisoning through the skin and respiratory tract.
It is not so much methyl alcohol itself that is toxic, but the products of its metabolism - formaldehyde and formic acid. The latter is a powerful inhibitor of tissue respiration and the main cause of metabolic acidosis (a shift in the pH of biological fluids to the acidic side). The main toxic effect is on the nervous, cardiovascular and excretory systems. The insidiousness of methanol is that it is quickly absorbed, but very slowly eliminated from the body. The maximum concentration in the blood is observed 30–60 minutes after consumption, and elimination lasts for 3-5 and even 7 days. Moreover, during this time, methanol can be released by the gastric mucosa and reabsorbed.
Methyl alcohol is metabolized in the liver by the enzyme alcohol dehydrogenase, but more slowly than ethanol. It is this competitive interaction that makes ethyl alcohol the main antidote for methanol poisoning.
The main pathogenetic disorders in the body caused by methanol and the products of its biochemical transformation are manifested in the following phenomena: • Metabolic acidosis (increased acidity of the internal environment). • Decreased oxygen saturation of the blood.
In addition, methanol can accumulate (accumulate) in the body, which can cause chronic poisoning with the systematic intake of even small doses of this toxic substance.
What kind of alcohol are they poisoning with?
In addition to alcohol, which is clearly not intended for ingestion, poisoning with so-called “scorched vodka” often occurs. It can be quite difficult to distinguish licensed and counterfeit vodka by appearance. Moreover, there are numerous cases where similar products were sold in regular stores and even supermarkets of large retail chains.
To protect against this, as well as in an attempt to save money, people are increasingly resorting to moonshine. But even here, not everything is smooth and simple. Moonshine can contain a large amount of harmful impurities in the form of fusel oils. The consequences of consuming such a “homemade” product can also be very, very serious.
In addition to “palenka” and moonshine, the leading positions in the number of cases of poisoning include medical tinctures with alcohol. Alcohol tinctures of pepper and hawthorn are especially popular. Their use as an alternative to food alcohol in any long term leads to rapid social and mental degradation.
Poisoning after food alcohol may not appear immediately and may not be in an acute form; such poisoning can be treated in the usual ways, but if the signs described below are observed, special measures must be taken.
Removing alcohol intoxication
The intervention of a narcologist requires moderate and severe degrees of alcohol poisoning, and in the latter case hospitalization is indicated. To treat intoxication, a detoxification drip with electrolyte solutions is placed to correct fluid deficiency, metabolism, and water-salt balance. Additionally, medications are used to eliminate the consequences of severe intoxication. This:
- hepatoprotectors;
- drugs to improve blood circulation, cognitive abilities, and prevent further hypoxia;
- means for stabilizing blood pressure and heart rate;
- painkillers;
- sedatives.
But it is possible to determine exactly how to relieve alcohol intoxication only after a preliminary assessment of the patient’s condition and clarification of possible contraindications to the use of certain medications. If help is provided at home, an ECG is taken, neurological reflexes are checked, heart and breathing sounds are auscultated, blood pressure, pulse, and saturation are measured.
In the hospital there are much more opportunities to solve the problem of how to relieve the symptoms of acute ethanol poisoning. All necessary medications are administered almost around the clock, and drug treatment is supplemented with hardware cleansing.
Single episodes of moderate intoxication are quite normal for an adult. But if such cases become more frequent, you should consult a doctor as soon as possible. Chronic alcohol intoxication is fraught with very serious consequences. These are not only complications from internal organs, but also irreversible personality changes. This condition requires complex, long-term treatment, and we are talking not only about the use of medications, but also about psychotherapy, physiotherapy and other methods of getting rid of alcohol addiction.
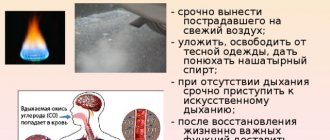
Emergency care for poisoning with alcohol substitutes
If poisoning with alcohol substitutes is suspected, emergency care will depend on the initial condition of the patient. If the patient is unconscious, then he must be laid on a flat, hard surface, turn his head to the side to avoid aspiration of vomit and call an ambulance. If respiratory and cardiac activity is impaired, first call an ambulance, and then perform indirect cardiac massage and artificial respiration.
When the victim is conscious, first aid consists of the following:
- take sorbent;
- saline laxative;
- drink an enveloping decoction, for example, jelly;
- emergency hospitalization in a hospital.
Treatment of poisoning with alcohol surrogates in a hospital:
- Gastric lavage through a tube. In case of methanol intoxication, it is repeated for 3 days. They give sorbents.
- Antidote treatment in both cases is the same: five percent ethanol is administered intravenously. For mild poisoning, 30% ethyl alcohol can be taken orally.
- In case of ethylene glycol poisoning, calcium gluconate is administered to neutralize the breakdown products of the toxic substance.
- Forced diuresis is carried out, which is based on the drip administration of large amounts of solutions and diuretics in the absence of renal dysfunction.
- Removal of toxins from the blood is also carried out by hemodialysis.
- Glucose with novocaine, prednisolone, and vitamins B and C are administered.
- In case of methanol poisoning, spinal punctures are performed.
- In severe cases of ethylene glycol toxicity, a kidney transplant may be necessary.
Additional Information
Find out:
- What substances available for everyday use contain ethylene glycol, and what properties does it have? What does ethylene glycol poisoning , what symptoms does it cause and how effectively is it treated. What antidote exists for intoxication and how accessible is it for use?
- What are the common sources of fluoride poisoning and why are children at risk? What symptoms indicate intoxication, and what needs to be done at home to provide first aid if you feel unwell.
- After consuming what foods can histamine poisoning , and how dangerous this condition is.
- Due to an overdose of which drugs iron poisoning and how effectively it is treated.
- Common sources of lead intoxication , and what irreversible consequences poisoning can lead to.
- Is it possible to get intoxicated after exceeding the dose of calcium antagonists , and does this affect human health?
Types of coma after alcohol
In case of alcohol poisoning, three stages of coma are distinguished in accordance with the degree of severity.
- Superficial coma, symptoms: constricted pupils, there is a reaction to light. When trying to bring the patient to ammonia, he reacts with defensive movements of his hands and a corresponding grimace, but does not come to his senses. To quickly bring the patient to consciousness, it is recommended to perform gastric lavage using a gastric tube; usually the prognosis is favorable.
- Moderate severity, coma. Unlike the superficial one, there is a pronounced sign - relaxation of muscle tone. The patient reacts poorly to inhalation of ammonia vapor. There is no restoration of consciousness after gastric lavage. These symptoms require hospitalization to the toxicology department.
- Deep coma. Tendon reflexes are completely absent. The pupils do not react to light, may be narrowed or wide with impaired breathing, and convulsions occur. There is no reaction to ammonia or pain sensitivity. Emergency immediate hospitalization to the toxicology department is indicated.
A comatose state from acute alcohol poisoning manifests itself externally in the following: the face becomes bluish and hypertrophied, the skin is sticky and cold, the pulse is weakened, thread-like, and breathing is intermittent and shallow. Such a critical condition of the patient requires the help of a resuscitator.
The likelihood of developing an alcoholic coma is especially high when an average-weight person, who usually rarely drinks, consumes the following dose of alcohol at one time or in a short period of time: 150-180 pure undiluted alcohol, or in terms of vodka 420-450 g, while creating alcohol concentration 0.3% or more.
Of course, if the indicated signs of alcohol poisoning are observed without first aid, alcohol poisoning can lead to death. What to do in case of alcohol poisoning, of course, provide first aid as quickly as possible. The lethal dose of alcohol is not constant and averages 5-13 grams of 96% alcohol per kilogram of weight. In alcoholics at the second stage, due to acquired tolerance to alcohol, the lethal dose is significantly increased compared to light drinkers and non-drinkers. Alcohol poisoning can result in the death of the victim, which occurs as a result of disruption of the cardiovascular system, respiratory arrest, hypothermia and other reasons.
Combination of mephedrone with other drugs
In an effort to enhance and diversify the sensations, drug creators often combine several substances in a dose of mephedrone. No one can predict the consequences of such experiments.
Mephedrone and cocaine
A potent drug combined with synthetic salt is a harsh mixture that can destroy your health in the first dose and form a strong addiction. Most often, these experiments very quickly lead to a mental hospital or even early death from an overdose.
Mephedrone and alcohol
At parties, young people often combine these two dangerous substances, the consequences of combining which can be disastrous. Some do this purposefully - to prolong the effect of the drug. But this poses a serious risk of overdose or death from general intoxication of the body.
First aid for alcohol poisoning
First of all, if you suspect, let alone observe, signs of alcohol poisoning, even subtle symptoms with a fair amount of alcohol consumed, you should call an ambulance. To call an ambulance, you need to dial 03 from a landline phone or 112 from a mobile phone and be prepared to provide the address where the patient is located.
What else can be done when alcohol poisoning is obvious. If the patient is conscious, but there is lethargy, severe weakness, drowsiness on the face, ammonia vapor is allowed to inhale. To do this, a gauze or cotton swab soaked in ammonia is brought to the nasal opening; an accessible method of providing assistance in case of poisoning is to prepare a non-concentrated solution of soda (1 teaspoon per liter) in cold water and give it to drink, then gently press with a spoon on the root of the tongue , thereby causing vomiting.
If the poisoned person is able to swallow, the poisoned person should be given up to twenty tablets of activated carbon at a time. You can give an anti-hangover drink, for example, “Cheerfulness”, up to three sachets per mug, or drink hot, strong tea. But these measures are possible if the poisoned person can control his actions.
If a person who has consumed a lot of alcohol has lost consciousness, it is important, before the ambulance doctors arrive, to carefully monitor that his tongue is not stuck, that nothing restricts his breathing, except that the poisoned person cannot choke on his own vomit. If you lose consciousness from poisoning, it is contraindicated to rinse your stomach; the person may choke. Ethyl alcohol causes vasodilation, which means that the body affected by poisoning loses heat quickly. As a result, hypothermia may occur.
It is important to take warming measures: move the patient to a warm place or at least wrap him well. Place the poisoned person on his side, partially on his stomach so that his head is lowered, then possible vomit will not enter the respiratory tract. If cardiac activity stops and breathing stops, resuscitation measures are immediately started to maintain vital processes until doctors arrive.
Mephedrone addiction
Dependence on a synthetic drug develops quite quickly. Even if you use it rarely, mental cravings will occur after 6-8 doses.
Stages of mephedrone addiction:
- Initial use of the drug . If the addict decides to continue the “high”, then the need for the substance will appear after 2-3 doses.
- Getting used to a substance on a physical level . A gradual weakening of the effect, which entails an increase in dosage.
- Sustained dependence , severe withdrawal symptoms in the absence of the drug. The appearance of depression, constant anxiety and insomnia.
- The final . The drug becomes the meaning of life. The maximum lifespan of mephedone addicts is 5 years. Death most often occurs due to cardiac arrest.
Overdose
Since the composition of the drug may change, an overdose is possible even when taking the usual dose. And also the body may simply not withstand the constant struggle for life and give up the next time you use mephedrone.
Mephedrone withdrawal
Withdrawal syndrome from mef manifests itself in the following symptoms:
- sweating, fever (from heat to chills);
- insomnia;
- lack of appetite;
- strong thirst;
- blood from the nose or mouth;
- nausea and vomiting;
- seizures, convulsions;
- heart rhythm disturbances;
- unusual “chemical” body odor.
Consequences of poisoning with alcohol surrogates
Despite the fact that the course of poisoning with alcohol substitutes containing ethyl alcohol is more favorable, the consequences can be very serious. The prognosis is determined by the amount of counterfeit alcohol consumed, and, to a greater extent, by the timeliness of the medical care provided. If the patient suffered from chronic alcoholism, the poisoning is more severe and there are more deaths than in those who did not have alcohol dependence.
When intoxicated with methanol, complete loss of vision is possible, which is not restored after the poison is removed from the body. Ethylene glycol-based surrogates lead to kidney failure. Such patients mostly die.
The problem of poisoning with alcohol surrogates, unfortunately, remains relevant today. Many people are faced with this disease, so knowing the signs of such intoxication will help not only provide timely emergency assistance to the victim, but also save his life!
Prognosis for recovery
The most optimistic prognosis is when drinking ethyl alcohol. However, the outcome largely depends on the dose of alcohol and timely assistance provided. With regular alcohol consumption, liver destruction, gastrointestinal diseases, neurological and mental disorders are inevitable. The most severe consequences are poisoning with methyl alcohol or ethylene glycol. These are blindness, cirrhosis of the liver, gastritis, ulcers, kidney failure. Disability or even death of a person are common consequences of using a surrogate. In order not to endanger your life, you should drink only high-quality and licensed alcohol.