Release form
It is produced in the form of a herbal collection, which looks like small yellow-brown pieces of plant material interspersed with yellow, white, green or brown. Characterized by a strong aroma. The water extract is bittersweet.
The medicine is packaged in bags of 50 g or in small bags of 1.5 g. A bag of 50 g or 20 bags of 1.5 g is placed in a cardboard box.
Small bags contain plant raw materials, which are more crushed, almost to a powdery consistency.
Pharmacodynamics and pharmacokinetics
Pharmacodynamics
The effect of Fitogastrol (gastrointestinal collection) on the human body is determined by the properties of the plants included in its composition:
- peppermint leaves stimulate the secretion of gastric juice, increase the efficiency of the digestive process;
- licorice root contains the substance glycerizin , which promotes the healing of ulcers and prevents their occurrence;
- chamomile flowers stimulate regeneration processes;
- the fruits of dill contain a whole complex of biologically active substances (essential oil, flavonoids, carotene, phytoncides, sugars, vitamin C and others), which causes choleretic, antispasmodic, diuretic effects, helps cope with gas formation in the intestines, increases the secretory activity of the gastric glands;
- a complex of biologically active substances contained in the rhizomes of calamus affects the endings of taste buds, causing an increase in appetite , improves the quality of the digestive process, enhances the reflex secretion of gastric juice, increases bile secretion, increases the tone of the gallbladder, and stimulates urination.
Pharmacokinetics
Not studied.
Collection of gastrointestinal Fitogastrol N20 filter bags
Latin name
Phytogastrol
Active ingredient: Calamus rhizomes + Peppermint leaves + Chamomile flowers + Licorice roots + Dill fruits (Acori calami rhizomata + Menthae piperitae folia + Chamomillae recutitae flores + Glycyrrhizae radices + Anethi graveolentis fructus)
Compound
Each gram of the collection contains 200 mg of active ingredients: chamomile flowers, peppermint leaves, dill fruits, calamus rhizomes and licorice roots.
Release form
It is produced in the form of a herbal collection, which looks like small yellow-brown pieces of plant material interspersed with yellow, white, green or brown. Characterized by a strong aroma. The water extract is bittersweet.
The medicine is packaged in bags of 50 g or in small bags of 1.5 g. A bag of 50 g or 20 bags of 1.5 g is placed in a cardboard box.
Small bags contain plant raw materials, which are more crushed, almost to a powdery consistency.
pharmachologic effect
It is a herbal preparation that affects the digestive system. It has antispasmodic, anti-inflammatory, enveloping, choleretic effects and is able to correct the functioning of the gastric glands.
Pharmacodynamics and pharmacokinetics
Pharmacodynamics
The effect of Fitogastrol (gastrointestinal collection) on the human body is determined by the properties of the plants included in its composition:
peppermint leaves stimulate the secretion of gastric juice, increase the efficiency of the digestive process;
licorice root contains the substance glycerizin, which promotes the healing of ulcers and prevents their appearance;
chamomile flowers stimulate regeneration processes;
the fruits of dill contain a whole complex of biologically active substances (essential oil, flavonoids, carotene, phytoncides, sugars, vitamin C and others), which causes choleretic, antispasmodic, diuretic effects, helps cope with gas formation in the intestines, increases the secretory activity of the gastric glands;
a complex of biologically active substances contained in calamus rhizomes affects the endings of taste buds, causing an increase in appetite, improves the quality of the digestive process, enhances the reflex secretion of gastric juice, increases bile secretion, increases the tone of the gallbladder, and stimulates urination.
Pharmacokinetics
Not studied.
Indications for use
Gastric collection Fitogastrol is indicated for various diseases of the digestive tract, for example, colitis, gastritis, functional dyspepsia. Usually used in combination with other medications.
Contraindications
The use of Fitogastrol is contraindicated for:
hypersensitivity to one or more ingredients included in the collection;
calculous cholecystitis;
exacerbation of peptic ulcer of the stomach and duodenum;
treating patients under 12 years of age;
during pregnancy and lactation.
Side effects
Allergy symptoms may appear. In this case, you need to consult your doctor about how to take Fitogastrol in the future and whether it is worth doing.
Fitogastrol, instructions for use (Method and dosage)
A tablespoon of the collection is poured into an enamel or glass container, poured with a glass of boiling water, closed and kept in a boiling water bath for 15 minutes. Then cool for 45 minutes, filter and squeeze. Add water to the infusion so that its volume becomes 200 ml.
Place 2 bags in a glass or enamel bowl, add a glass of boiling water, leave for 15 minutes. Then the bags are squeezed out, and the volume of the solution is adjusted to 200 ml.
You need to drink half a glass half an hour before meals. The reception is repeated three times a day. The duration of the course of treatment is selected by the attending physician individually for each patient, as it depends on the nature of the disease.
Shake it well before drinking part of the solution. The prepared solution can only be stored in the refrigerator and for no longer than 2 days.
Overdose
There have been no reports of overdose.
Interaction
Not known.
Terms of sale
Over the counter.
Storage conditions
Must be stored in original packaging in a cool, dry place.
Best before date
2 years (dry collection), 2 days (prepared aqueous extract).
For children
Not used for treatment in patients under 12 years of age.
During pregnancy and lactation
It is not advisable to prescribe to pregnant and breastfeeding women, since clinical studies have not yet been conducted regarding the safety of the use of Fitogastrol for such categories of patients.
Fitogastrol, instructions for use (Method and dosage)
A tablespoon of the collection is poured into an enamel or glass container, poured with a glass of boiling water, closed and kept in a boiling water bath for 15 minutes. Then cool for 45 minutes, filter and squeeze. Add water to the infusion so that its volume becomes 200 ml.
Place 2 bags in a glass or enamel bowl, add a glass of boiling water, leave for 15 minutes. Then the bags are squeezed out, and the volume of the solution is adjusted to 200 ml.
You need to drink half a glass half an hour before meals. The reception is repeated three times a day. The duration of the course of treatment is selected by the attending physician individually for each patient, as it depends on the nature of the disease.
Shake it well before drinking part of the solution. The prepared solution can only be stored in the refrigerator and for no longer than 2 days.
Fungal infections of the gastrointestinal tract
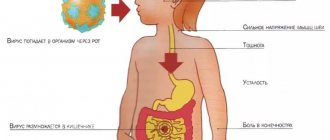
Today, humanity is experiencing an epidemic of opportunistic infections, among which mycoses occupy one of the leading places. According to WHO, in the last decade, about 20% of the world's population suffers from mycoses [1]. Mycoses are infectious diseases whose etiological pathogen is fungi. Most often, people with primary or secondary immunodeficiency conditions suffer from mycosis [2]. Mycosis is an opportunistic infection [3, 4]. Mushrooms are lower plants (more than 100 thousand species), lacking chlorophyll, so their existence requires ready-made organic substances. The vast majority of fungi are saprophytes, a minority of them are parasites of humans and animals. About 500 species of fungi can cause infectious diseases in humans. The yeast-like C. albicans is most often found in humans [5]. Candidiasis is an anthroponotic mycosis characterized by damage to the mucous membranes and skin. Lesions in humans are caused by C. albicans (more than 90% of lesions), C. tropicalis, C. krusei, C. lusitaniae, C. parapsilosis, C. kefyr, C. guilliermondii, etc. [6–8]. At the beginning of the 20th century. candidiasis was observed relatively rarely. Since the beginning of the use of antibiotics and to the present day, the incidence of candidiasis has increased significantly and continues to grow. An unfavorable environmental situation, which has a negative effect on the immune system of the human body, is of no small importance in the development of candidiasis [9]. Candidiasis usually occurs endogenously as a result of dysfunction of the immune system and dysmetabolic disorders in the body. In recent years, candida are the most common causative agents of opportunistic mycoses [4]. When the body is affected by candida, severe visceral forms may develop, often involving the lungs and digestive organs and other body systems. Candidiasis can be systemic in nature and become disseminated (massive growth of the pathogen in the body) and take on the picture of fungal sepsis with damage to all organs (kidneys, heart, spleen, brain), and sometimes with the development of septic shock [10]. More often, this form of candidiasis affects patients with the last stage of cancer and AIDS [11, 12]. Etiology and pathogenesis
The most common causative agent of mycoses, C. albicans, is a normal commensal of the oral cavity, gastrointestinal tract, vagina, and sometimes skin. C. albicans are opportunistic microorganisms with a high level of carriage and a pronounced tendency to increase it: if in the 1920s. carriage on the oral mucosa was 10%, then in the 1960–1970s. increased to 46–52% [13]. Many studies have shown that any violations of the body’s resistance or changes in the normal intestinal microbial cenosis can lead to the development of the disease – candidiasis [14]. The skin and mucous membranes are “open systems” of the macroorganism, constantly in contact with the environment. In turn, Candida spp. widely distributed in nature, they often contaminate soil, water, food, and household surfaces. Frequent human contact with Candida spp. explains the significant prevalence of transient candidiasis in the human population. According to statistics, among the population of European countries, candida is detected in the feces of 65–80%. As an opportunistic representative of the human microflora, fungi do not pose a serious threat to the health of an immunocompetent person [15]. At the same time, against the background of an increase in the number of patients with disorders in antimicrobial resistance systems, a significant increase in the incidence of candidiasis is observed [16]. Many researchers associate the increase in candidiasis with risk factors, which include childhood and old age, therapy with glucocorticosteroids and antibacterial drugs, intensive cytostatic polychemotherapy, diabetes mellitus and other diseases of the endocrine system, AIDS, severe debilitating diseases, impaired trophological status, genetically determined immunodeficiencies [17 -19]. Primary infection of the human body by Candida occurs when passing through the mother's birth canal, as evidenced by the high frequency of Candida isolation in newborns (up to 58%) and the almost complete coincidence of the species composition of Candida in the child and mother. Infection is facilitated by the increased frequency of carriage and vaginal candidiasis in the last third of pregnancy. There is information about the transmission of Candida fungi during breastfeeding [20]. Fungi that parasitize human skin feed on particles of the epidermis, the horny masses of the nail plates, and the products of their life - proteins - cause an allergic reaction. The pathogenicity factor of fungi of the genus Candida is their ability for adhesion and invasion, followed by tissue cytolysis, and then lymphohematogenous dissemination [21]. Candida spp. capable of an invasive process in the mucous membranes, primarily represented by stratified squamous epithelium, less often - single-layer cylindrical. Most often, the invasive mycotic process is observed in the oral cavity, esophagus, stomach and intestines. It has been proven that even without penetration deep into the epithelium, Candida spp. [22] can cause pathology – a non-invasive form of candidiasis. Contact of surface and corpuscular antigens of the fungus with immunocompetent cells of the macroorganism can lead to the production of increased amounts of specific IgE and sensitized lymphocytes, which serves as the pathogenetic basis for mycogenic sensitization. Allergens in Candida albicans are also the primary metabolites - alcohol dehydrogenase and acidic P2 protein. This is potentially dangerous in terms of the development of mycogenic allergic diseases: specific bronchial asthma, atopic dermatitis, urticaria. Resorption in the intestine of metabolic products of fungi of the genus Candida - its plasmacoagulase, proteases, lipophosphorylases, hemolysin and endotoxins can cause specific intoxication and secondary immunodeficiency [23]. Due to interaction with representatives of obligate normobiota and opportunistic microorganisms Candida spp. can induce dysbiosis and mixed infection of mucous membranes. The key factor in the onset of the infectious candidiasis process is the violation of nonspecific and specific resistance of the body both at the local and general levels [23]. Factors of nonspecific resistance traditionally include an adequate balance of desquamation and regeneration of epithelial cells, mucopolysaccharides of mucus, normal microbiota of the mucous membranes (Bifidobacterium spp., Lactobacillus spp., Escherichia coli, Peptostreptococcus spp.), peristaltic activity and the acid-enzyme barrier of the digestive tract. It has been shown, for example, that treatment of patients with drugs containing bifidobacteria significantly reduces the content of Candida fungi in the feces of patients [24]. Nonspecific factors also include secretory IgA, lysozyme, transferrin, and complement components. However, the number and function of polymorphonuclear mononuclear phagocytes are most important, in particular their ability to chemotaxis, attract, kill, and present fungal antigen. It is under conditions of neutropenia that life-threatening forms of candidiasis develop, including visceral lesions (liver, gallbladder, pancreas) [11]. The specific immune response to candidiasis is represented by the production of specific anti-candidiasis antibodies of the classes IgA, IgG, IgM, which inactivate invasion enzymes and endotoxins of the fungus, as well as together with complement components involved in opsonization [25, 26]. The conflict between the pathogenicity factors of the fungus and the factors of antifungal resistance leads to the development of one or another form of candidiasis. The mechanisms of pathogenesis of 2 fundamentally different forms of candidiasis (invasive and non-invasive) formed the basis for the classification of intestinal candidiasis.
Clinical forms
For practical purposes, it is necessary to distinguish 3 forms of damage: – invasive diffuse;
– focal (secondary to duodenal ulcer, nonspecific ulcerative colitis); – non-invasive (so-called candidiasis dysbiosis) [27]. Quite often, candidiasis of the digestive system occurs in the form of a mixed infection: Candida-bacterial, Candida-herpetic, Candida-protozoal, which makes the clinical picture of the disease quite variable. The frequency of mixed infection in intestinal dysbiosis with increased proliferation of fungi of the genus Candida, according to some data, is 63%. Moreover, an association with a significant number of bacteria with the so-called proteolytic main metabolic pathway (opportunistic pathogens) is more often found: Escherichia coli, Ristella, Clostridium perfringens, Klebsiella, Morganella, Bacteroides, Staphylococcus aureus, Pseudomonas aeruginosa [28]. Among all localizations of candidiasis of the digestive tract, oropharyngeal localization
ranks first [29].
Candidal stomatitis in newborns is a common disease. In the first days after birth, the baby’s mucous membranes are resistant to fungi. Subsequently, insufficient secretion of IgA and a gradual decrease in antimicrobial immunity transmitted from the mother lead to high morbidity [30, 31]. Oral (oropharyngeal) candidiasis is a widespread mycosis in people suffering from various forms of immunodeficiency, primarily AIDS and hematological malignancies, and the gastrointestinal localization of candidiasis in patients with AIDS can be a source of candidemia, which in such patients with other localizations of candidiasis occurs in only 1% of cases [ 32, 33]. A common mycosis of the digestive tract is esophageal candidiasis,
which is recorded both in immunocompetent and (much more often) in immunocompromised individuals [34].
Candidal esophagitis in general hospitals occurs in 1.3-2.8% of patients, in transplant departments - in 4%, with disseminated carcinomatosis - in 2.8-6.7%. This disease often occurs without subjective complaints and is detected by chance during “continuous” studies of the population in 1–7% of cases. Sometimes patients note pain and discomfort when passing solid and liquid food, dysphagia, and hypersalivation. According to the depth of the lesion, 4 types are endoscopically distinguished - from mild edema, hyperemia, single white plaques < 1 mm in diameter to massive inflammation, deformation and bleeding of the mucosa, ulceration, even perforation. A comparative assessment of various methods for diagnosing esophageal candidiasis showed that in 95% of cases, candidiasis was detected by analyzing scrapings and only in 39% by analyzing biopsy material [35]. Gastric mycoses,
including candidiasis, are rarely noted in the absence of any other pathology of somatic or bacterial etiology [36–38].
Their share among all cases of candidiasis of the upper digestive tract is only 5.2%. Much more often (up to 17–30%) Candida spp. found in biopsy samples of gastroduodenal ulcers, as well as in chronic gastritis [39]. However, only the findings of pseudomycelial structures of the fungus, and not individual non-budding cells, during a morphological study of cytological and/or histological preparations stained according to the Romanovsky-Giemsa method or the PAS method, reliably confirm the diagnosis of gastric candidiasis. In recent years, Candida spp. often isolated in association with Helicobacter pylori, and standard anti-Helicobacter therapy increases the incidence of gastric candidiasis [40]. The vast majority of Candida spp. isolated from patients (65.6%) had high or moderate virulence. When isolated from the gastric juice of patients with gastroduodenal diseases, the association of Candida spp. and Helicobacter pylori, a more severe course of the disease can be assumed, and the planned antibacterial therapy must be carried out in conjunction with antifungal therapy [39]. Intestinal candidiasis
as an isolated form of the disease is rare.
Usually it is a continuation of candidiasis of the stomach and upper digestive tract. Intestinal candidiasis is often accompanied by diarrhea. There are diarrhea of various etiologies [40] with concomitant release of Candida and candidal diarrhea (CD), in which Candida is the only excreted pathogen. The main predisposing risk factor for KD, especially in hospitalized patients, is antibiotic therapy. Other risk factors: endocrine disorders, immune dysfunctions, neoplasms, steroid therapy; The elderly age of patients also plays a role [41]. In patients with CD, C. albicans is most often isolated, followed by C. krusei, C. tropicalis, C. kefyr, C. stellatoidea, C. guilliermondii, C. parapsilosis, C. lusitaniae [41]. In cases where Candida is a component of the normal intestinal biota, its growth and reproduction are suppressed by intestinal microorganisms, where the fungus is present in stable quantities and does not multiply [35]. When the bacteriobiota is suppressed by antibiotics, yeast multiply with the formation of growth tubes and the appearance of mycelial structures. According to T.V. Tolkacheva et al. [13], the frequency of isolation of yeast fungi from the intestines of immunocompromised patients remains high, reaching 63–65% in the last 2 years. The ratio of detection rates of C. albicans and non-albicans strains is 52.5%. Among the latter, C. krusei (40%), C. glabrata (28%) and C. kefyr (15.6%) dominate [42]. An increase in the frequency of occurrence of an association of 2 species of Candida non-albicans and an expansion of the species spectrum of yeast fungi colonizing the intestines of patients with hemoblastosis were noted. Candidiasis of the large intestine is a rare disease; it is more often recorded in association with other intestinal pathogens of a bacterial nature [43]. In recent years, it has been hypothesized that chronic intestinal candidiasis may be an etiological factor in the formation of chronic fatigue syndrome [44]. Signs of mycogenic sensitization are detected in 10.4% of patients with intestinal dysbiosis with excessive growth of Candida fungi. The diagnosis is established in the presence of the following criteria, such as: flatulence, abdominal discomfort, changes in stool consistency and frequency, signs of moderate intoxication and a tendency to exacerbation of allergic diseases. Fungal infection of the biliary system
is facilitated by previous biliary dyskinesia, dyspancreatism, giardiasis, cholestasis, hypotension of the gallbladder and other lesions.
Under these conditions, favorable conditions are created for the proliferation of fungi and other microorganisms. The cause of candidiasis cholecystitis can be stones in the bile ducts, which are often a “reservoir” for fungi; some authors even call them “fungal bodies” or “candidiasis stones”. Mycoses of the biliary tract are more common than is commonly believed. Diagnosis
Diagnosis of candidiasis using purely clinical methods is impossible due to the fact that its clinical manifestations do not have absolute specificity. In the vast majority of cases, modern clinical and laboratory instruments allow for high-quality examination and help the clinician make a diagnosis, as well as prescribe effective treatment for infections caused by fungi. In recent years, endoscopic technologies have expanded the possibilities for diagnosing fungal esophagitis and gastritis. During esophagogastroduodenoscopy, attention is paid to hyperemia and ulceration of the mucous membrane, the presence of white deposits and films, narrowing of the lumen of the esophagus, and accumulation of mucus [45]. During this procedure, it is imperative to take material for microbiological examination, since the etiology of these manifestations is not always fungal. Moreover, the information content of plaque research is higher than that of biopsy specimens (95% compared to 39%). Video information endoscopic studies with digital recording and image analysis are especially promising. A clear distinction between unchanged and pathological tissues and analysis of histochemical processes in the mucous membrane of the digestive tract are possible using endoscopic spectroscopy and fluorescence endoscopy [46]. Video and colonoscopy, chromoendoscopy against the background of “medicinal” sleep using Diantek technology are distinguished by high quality research, painless manipulations and the absence of stress and fear in patients [8]. It should, however, be emphasized that invasive manipulations with inflamed gastrointestinal mucosa are unsafe, can promote fungal and bacterial dissemination, and sometimes lead to injury and perforation of the wall of the esophagus or stomach. Endoscopic ultrasonography with Doppler mapping and contrast enhancement of tissue and vascular structures is promising; it allows detailed differentiation of all layers of the wall of the digestive tract. Non-invasive methods - virtual endoscopy, which allows obtaining a 3-dimensional image, magnetic resonance imaging - have a great future [47]. Studying gastroduodenal motility using scintigraphy and electrogastrography is also important for diagnosis and prescribing additional medications, since impaired motor function of the stomach and “stagnation” in the gastrointestinal tract create conditions for the proliferation of fungi and bacteria. Colonoscopy makes it possible to assess the condition of the intestinal mucosa, the presence of white plaque, ulcerative defects, etc. In the future, methods based on new scientific and practical research will be introduced in gastroenterology: enzyme immunoassay of fecal antigens, PCR and even genetic testing [5, 47]. Laboratory confirmation of a fungal disease of the gastrointestinal tract is possible through microscopy and/or cultural examination of swabs from the mucous membranes of the oral cavity and esophagus, the contents of the stomach and intestines, pathological films, plaque, etc. Quantitative assessment of fungi in biosubstrates should be carried out in comparison with clinical symptoms, taking into account the presence background diseases, mixed infections, etc. [48]. For example, the detection of single Candida colonies on the mucous membranes is not a basis for diagnosing candidiasis in immunocompetent patients. In stool, the number of colonies (more than 105–106) acquires diagnostic significance. Culture results are interpreted differently, with a lower diagnostic threshold, in immunosuppressed individuals, neutropenic patients with AIDS, and in intensive care units [49, 50]. You should also pay attention to the ability of mushrooms to vegetate and form mycelium, since this is one of the laboratory signs that confirm the diagnosis of candidiasis. Histological (Gomori-Grokkot staining, PAS reaction) and cytological (Romanovsky-Giemsa staining) studies of biopsy specimens can detect tissue forms of fungi. Many authors consider these methods to be the most reliable. In addition, mycelium and pseudomycelium in tissues confirm the presence of an invasive form of fungal infection of the gastrointestinal tract [51]. Microbiological examination of portions of bile obtained through multifractional duodenal intubation makes it possible to differentiate fungal from bacterial or functional pathology of the duodenum, gallbladder, biliary tract and liver.
Conclusion
Thus, today candidiasis is the most common type of fungal infection. People with weakened immune systems should take any manifestations of candidiasis seriously and consult a doctor at the first sign of the disease for treatment.
Analogs
Level 4 ATX code matches: Verona
Phibs
Gastrikumel
Thyroidea Compositum
Berlition
Thiolepta
Gastric collection
Espa-Lipon
Brewer's yeast
Lipoic acid
Rosehip syrup
Octolipen
Thioctacid
Thiogamma
Figurin
Analogues of Fitogastrol:
- Actovegin;
- Aloe juice;
- Aloe Extract.
Fitogastrol price, where to buy
Fitogastrol can be bought for about 75 rubles in Russian pharmacies or for 25 hryvnia in Ukrainian pharmacies.
- Online pharmacies in RussiaRussia
- Online pharmacies in UkraineUkraine
ZdravCity
- Fitogastrol (Gastrointestinal collection) PharmaColor 2g filter pack.
20 pcs. JSC Krasnogorskleksredstva 106 rub. order
Pharmacy Dialogue
- Phytogastrol collection (Gastrointestinal) (form 2g No. 20) Krasnogorskleksredstva
90 rub. order
- Phytogastrol collection (Gastrointestinal) (50g) Krasnogorskleksredstva
75 rub. order
show more
Pharmacy24
- Phytogastrol collection 1.5 g in sachets No. 20 PrAT "Liktravi", m.
Zhytomyr, Ukraine 33 UAH. order
Medicinal mixtures are mixtures of several types of crushed, less often whole, plant materials. The composition of the collection includes various parts of plants: roots, bark, grass, leaves, flowers, fruits, seeds. Multicomponent medicinal herbal infusions have long been used in medical practice, which is explained by the effectiveness and gentleness of their action, the absence, as a rule, of unwanted side effects during long-term use, as well as the ease of preparation. Russia has a sufficient raw material base for many types of medicinal plants, experience in their production and clinical use. Medicinal herbal preparations are the most popular and widely used form of processing of medicinal plant materials.
Compositions from medicinal plant materials, sometimes with the addition of minerals, have been used in medicine all over the world since ancient times. Herbs are especially popular in oriental medicine: Chinese, Tibetan, etc. The recipes for these herbs are distinguished by the complexity of their composition, with a large number of components belonging to various morphological groups of raw materials. In Russian folk medicine, herbs were used less widely, since preference was given to individual medicinal plants.
Multicomponent mixtures from medicinal plant raw materials have valuable advantages over other herbal medicines: the ability to provide the main pharmacological effect in combination with a complex effect on the patient’s body as a whole, gentleness of action and the absence, as a rule, of undesirable side effects. They are quite simple to industrially produce and relatively cheap.
Treatment with multicomponent medicinal herbal mixtures is usually more effective than with single plants. When compiling the collection, it is necessary to take into account the individual characteristics of the patient and the presence of concomitant diseases. When choosing a collection, you need to know your blood pressure and take into account the main trend of its changes. For example, when choosing a collection for a patient with cholecystitis with arterial hypertension, it is necessary that the collection includes plants not only with a choleretic effect, but also with a hypotensive effect, otherwise the treatment may provoke a hypertensive crisis and worsen the general condition. In addition, one should take into account the tendency to constipation or diarrhea; Accordingly, the effect should be of a laxative or astringent nature. The effect of medicinal plant materials largely depends on the dose. Rhubarb root, for example, in large doses is used as a laxative, and in small doses, on the contrary, it has a strengthening effect. Various doses of spicy-bitter raw materials stimulate or inhibit the secretion of gastric juice. Some plants act on the muscles of the uterus and can be dangerous during pregnancy. Herbal infusions and remedies are not recommended to be taken during menstruation. Medicinal plant materials have a versatile effect. This explains the fact that in recipes with different purposes, the same components are often found, but in different quantities and different combinations. Only a doctor can foresee the unwanted side effects of medicinal plants after a comprehensive examination of the patient.
Depending on the types of raw materials included in the collection, infusions or decoctions are prepared on its basis. If the collection includes fragrant essential oil plants, then an infusion is usually prepared from them. Boiling is not allowed, since essential oils are volatile substances that evaporate along with water. Medicinal mixtures contain various biologically active compounds, which, simultaneously with the treatment of the underlying disease, additionally enrich the body with various vitamins, mineral compounds and other plant components that help increase the body's resistance, have a beneficial effect on the central nervous system, improve hematopoiesis, neutralize toxins and accelerate their removal from the body. body. In this case, the influence on physiological processes is carried out by natural, more acceptable organic substances for the body. Allergic complications when treated with medicinal herbal preparations are observed much less frequently than when using other medications (for example, of chemical origin). The versatile effects of plant biologically active substances often achieve their goals. Thus, when prescribing a complex collection for liver diseases, immortelle substances increase the secretion of bile, gastric and pancreatic juice, increase the tone of the gallbladder, and change the chemical composition of bile. Substances contained in corn silk have a beneficial effect on metabolism and improve bile secretion. Barberry substances reduce and relieve pain, which is due to the presence of the alkaloid berberine, which has an antispasmodic effect. For the same purpose, a peppermint leaf is often added to such a collection.
In addition to organic substances, the collections contain macro- and microelements that are involved in metabolism and are in functional interaction with enzymes, vitamins, hormones and other biologically active substances. Manganese, copper, zinc, cobalt in microdoses stimulate the production of antibodies and increase the body's resistance. Copper, iron, zinc, cobalt reduce the permeability of biological membranes. When treating a patient with multicomponent medicinal preparations, proteins, amino acids, carbohydrates, lipids, enzymes, vitamins, organic acids, alcohols, aldehydes and ketones, esters of phosphoric acid and other acids, phytosterols, resins and tannins, glycosides, terpenoids, coumarins are introduced into the body , amides and amines, betaines, choline and choline esters, purines and pyrimidines, alkaloids, bitter substances and many others.
The most popular medicinal herbal infusions are: antimicrobial, gastrointestinal, urological, thoracic, sedative, choleretic, antisclerotic, antispasmodic, carminative, diuretic, antiasthmatic.
Diseases of the gastrointestinal tract are quite widespread, accounting for 35–37% of the total morbidity of the population. The most common among them are gastritis, peptic ulcer, enterocolitis. Therapy for inflammatory and destructive diseases of the gastrointestinal tract is aimed at correcting disorders of gastric secretion, motor function of the stomach and intestines, intestinal digestion, and also involves influencing the altered mucous membrane of the stomach and intestines. The use of synthetic drugs does not always have the desired effect in this pathology; In addition, the development of adverse reactions and complications is possible. In such cases, as well as for the prevention of exacerbations of chronic diseases of the gastrointestinal tract, herbal preparations are very promising. The gastrointestinal collection is a combined preparation of plant origin, containing five types of herbal medicinal raw materials. The infusion of the collection has antispasmodic, anti-inflammatory, choleretic, sedative, and regenerative effects. The effect is determined by the essential oil, polysaccharides, and flavonoids contained in chamomile flowers; essential oil from mint leaves, the main components of which are menthol, flavonoids, vitamins; essential oil from dill fruits.
Inflammatory diseases of the bronchi are now widespread and are one of the most common causes of loss of performance. Antibiotic therapy used for their treatment often leads to the development of allergies, the formation of resistance of microorganisms with loss of sensitivity to antibiotics during subsequent courses of treatment, the development of dysbiosis and an increase in the number of fungal diseases. Experience in the clinical use of chest collection demonstrates its effectiveness and feasibility of use in infectious and inflammatory processes in the bronchi as an auxiliary or alternative medicine, free of unwanted side effects. The medicinal effect of the collection is due to the antibacterial effect of chamomile flowers, wild rosemary shoots, calendula flowers, the expectorant and enveloping effect of licorice roots, violet grass and wild rosemary shoots, the anti-inflammatory and antispasmodic effects of licorice roots, chamomile flowers, calendula and mint leaves.
Recently, there has been a significant increase in the prevalence of conditions caused by increased physical or mental stress, exposure to adverse environmental factors, growing information loads, and stress. In such conditions, chronic fatigue develops, which leads to the development of insomnia, increased nervous excitability, irritability, neurasthenia, cardiovascular neuroses, tachycardia, hysteria, migraine, vegetative-vascular dystonia, menopausal disorders, and arterial hypertension. There are a lot of medicinal plants that have a sedative effect. The sedative, antispasmodic, hypotensive effect of the sedative collection is due to the medicinal herbs included in it. The effect is determined by the essential oils, saponins, tannins, and alkaloids contained in motherwort herb; peppermint leaves contain menthol; in rhizomes with valerian roots - ester of borneol and isovaleric acid, free valeric and other organic acids, alkaloids (valerine and hatinin), tannins, sugars; licorice roots contain licurazide, triterpenes, glycyrrhizic acid and flavonoids; thyme herb contains essential oil, tannins and bitter substances; in oregano herb - thymol, flavonoids, tannins; in hop cones – essential oil, organic acids, alkaloids, flavonoids, lupulin; in the sweet clover herb - coumarins, melitoside, polysaccharides.
The preparation of infusions and decoctions from collections of medicinal plants is not fundamentally different from the preparation of these preparations from the raw materials of individual medicinal plants. Specific instructions for preparing infusions and decoctions from collections usually give the following ratio: 1–2 tablespoons of the mixture per 200 ml of water.
In all cases, to completely extract the active substances, much more water is taken than when preparing similar medicines in a pharmacy. Therefore, the prepared medicine is most often taken not with spoons, but in 1/3–1/2 cups. If the infusion or decoction is prepared daily, it is not subject to microbial contamination and can be stored at room temperature throughout the day. For larger quantities, it should be stored in the refrigerator, but no more than two days.
Usually, when treating with medicinal plants, improvement occurs within a few days, but a lasting effect can be achieved only with long-term and regular use of medicinal herbs. The absence of a positive effect within 2–3 weeks is usually grounds for replacing the collection. The course of treatment with the fees should be determined by the attending physician with constant monitoring of the patient’s health.
When treating chronic patients with plant herbs, they are taken for a long time. To avoid getting used to them and reducing the effectiveness of the therapeutic effect, it is recommended to take a break for 1-2 weeks after each course of treatment (1.0–1.5 months). For the same reasons, it is advisable, after 2-3 courses of treatment with one of the preparations, to switch to treatment with another, which has a similar effect.
Information about the authors: Samylina Irina Aleksandrovna – Doctor of Pharmaceutical Sciences, Professor, Corresponding Member of the Russian Academy of Medical Sciences, Director of the Research Institute of Pharmacy; Head of the Department of Pharmacognosy MMA named after. THEM. Sechenov. Tel.; Sorokina Alla Anatolyevna – Doctor of Pharmaceutical Sciences, Professor of the Department of Pharmacognosy of the MMA named after. THEM. Sechenov. Tel.; Pyatigorskaya Natalya Valerievna – candidate of pharmaceutical sciences, associate professor, deputy director of the Research Institute of Pharmacy for scientific work. Tel.