Pathogen and causes of development
Filaria are widespread in many tropical and subtropical countries in Africa, Asia, South America, the Caribbean and Oceania. Mosquitoes that carry filariae are: Culex, Anopheles, Aedes, Mansonia.
A series of transformations occur in the mosquito’s body, leading to the formation of the third larval stage, which, when bitten by a mosquito, passes into the human body. The main vector in rural areas is mosquitoes of the genus Anopheles and the genus Culex in urban areas.
Humans are the only natural final host of the parasites that cause lymphatic filariasis, although some monkeys can be infected experimentally. Endemic outbreaks of filariasis can be small, and the risk of infection in sites located several kilometers apart can vary significantly.
Key Facts
- Lymphatic filariasis causes problems with the lymphatic system and can cause abnormal hypertrophy of some parts of the body, causing pain and leading to severe disability and social stigma.
- Lymphatic filariasis threatens 859 million people in 50 countries, who require preventive chemotherapy to prevent the spread of this parasitic infestation.
- Lymphatic filariasis can be eliminated by stopping the spread of infection through annual courses of preventive chemotherapy with safe combination drugs. Since 2000, more than 7.7 billion courses of therapy have been administered to stop the spread of infection.
- As of 2021, 51 million people were infected with lymphatic filariasis, a 74% decrease since 2000, when the WHO Global Program to Eliminate Lymphatic Filariasis was launched.
- Thanks to the success of WHO strategies, 648 million people no longer require preventive chemotherapy.
- The recommended package of basic health interventions can help alleviate the suffering of people living with lymphatic filariasis and prevent further limitations on their physical capabilities.
Lymphatic filariasis, known as elephantiasis, is one of the neglected tropical diseases.
Infestation occurs as a result of transmission of parasites to humans through a mosquito bite. The infection, usually acquired during childhood, causes hidden damage to the lymphatic system. Later in life, painful and severely disfiguring visible symptoms of the disease, lymphedema, elephantiasis, and scrotal swelling occur, which can lead to permanent disability. Such patients suffer not only from physical disabilities, but also from mental, social and financial problems, which contribute to their stigma and poverty.
In 2021, 859 million people in 50 countries lived in areas where preventive therapy is required to prevent the spread of infection.
Initial global estimates of the number of people affected by lymphatic filariasis estimated that 25 million men were living with hydrocele and more than 15 million were living with lymphedema. There are at least 36 million people in the world with such chronic manifestations of the disease. Eliminating lymphatic filariasis can prevent unnecessary suffering and help reduce poverty.
Symptoms and clinical picture
Certain parts of the lymphatic system are preferentially affected by filariasis, namely the lymphatic formations adjacent to the genitals. Apart from this, the parasite is usually localized either in the subcutaneous tissue, or in the lymphatic vessel, or in the vaginal membrane, etc., and these various localizations inevitably cause differences in the clinical picture. The latter is detected primarily by a kind of erysipelas or elephantiasis, lymphangitis, dilation of lymphatic vessels, for example, those of the groin area and especially the scrotum, and finally, edema of the vaginal membrane. Subsequently, the inguinal glands are affected, which usually swell symmetrically and form irregular projections that can reach, in general, the volume of a fist. The skin covering these parts is white, thin, elastic and not fused with the glands; The consistency of the tumor resembles a wen. With the slightest pressure a pit is formed, since in the compressed place the contents of the lymphatic glands are emptied into the abdominal lymphatic vessels, just as happens with some subcutaneous venous tumors, the leveling of which is never complete. These signs make such glandular lesions resemble a reducible hernia of the omentum.
Swelling of the inguinal glands is, if not constant, then at least a very common symptom, rarely observed, however, in other glands, which depends, of course, on the localization of adult filariae mainly in the genital area. The spleen and liver, as well as the thoracic organs and the brain, remain completely intact; But this cannot always be said about the ureters and testicles: if these organs are penetrated by filariae, they swell and become painful, so that urination is often impaired. Urine suddenly changes from completely transparent to cloudy, milky white, resembling a fat emulsion, and often contains fibrinous clots in suspension. The number of cases when urine is simply milky in color is quite limited, since almost always a small amount of blood is added to the chylous admixture, which, depending on the greater or lesser abundance, gives the urine a different color: the color of café au lait, chocolate, dark blue, pink or cherry shade. This coloration, however, can change daily or at different times of the same day and even during the same urination. Urine, in addition, is always more altered after fatigue than after rest.
The daily amount of urine is normal, and it is acidic and in cases of chyluria, in addition to fibrinous clots and protein, contains varying amounts of fat, from 25 to 46% or more. Under the microscope, organized elements are found, more or less changed red blood cells, lymphatic cells resembling lymph corpuscles, white blood cells and, finally, fatty cells that change the color of the urine, giving it a red and cloudy appearance. Finally, parasites are found here, especially if there is hematuria; Filaria germs can most often be found in the blood, although this does not happen at any time, but only in the evening. Starting in the evening, their number increases until midnight, after which it gradually falls, and in the morning they are no longer found.
The general state of health, despite the abundant content of filaria in the blood, most often remains satisfactory, so that one is even surprised at the good appearance of the patients. The latter do not feel anything and complain of almost nothing, unless there is hematuria or lymphorrhagia: in this latter case they become pale, sad, broken, complain of palpitations and digestive disorders, lose their strength and quickly get tired.
Fever, which is often intense and occurs in the form of attacks (at least at the beginning of the disease and in warm climates), is rare in our climate and is less severe if there is no hematochyluria or erysipelas, dermatitis or inflammation of the serous membranes . Poor nutrition in subjects suffering from filariasis predisposes to inflammatory lesions that are difficult to tolerate.
According to the information available regarding the development of the pathogenic parasite, filariasis represents two successive phases. The first phase is characterized by erysipelas or swelling of the lymphatic vessels, usually occurring first in the scrotum or genital area, or by edema of the scrotum, a limited lesion of the lymphatic vessels caused by the female filariae.
Having completed its development, this parasite mainly “builds a strong nest” in the lymphatic vessels and glands of the groin area; these vessels dilate and gradually merge into a varicose mass, reaching its maximum volume only after a year or several years. The varicose veins spread from the superficial inguinal glands to the deep ones, reaching the iliac and lumbar glands, then extending up to the thoracic duct, so that, thanks to the presence of the female filaria in the scrotum or groin, a significant part of the lymphatic system and all the blood. This is the second phase of the disease.
Filariasis (filariasis) in humans
V. G. Elibekov , maxillofacial surgeon, doctor of the highest qualification category, head of the maxillofacial surgical department of Municipal Budgetary Institution “City Hospital No. 1”, Novorossiysk
A. A. Polishchuk maxillofacial surgeon, dental surgeon, resident doctor, doctor of the second qualification category, maxillofacial surgical department of Municipal Budgetary Institution “City Hospital No. 1”, Novorossiysk
E. I. Potemkin Ph.D., maxillofacial surgeon, resident doctor of the maxillofacial surgical department of Municipal Budgetary Institution “City Hospital No. 1”, Novorossiysk
The expansion of ties between the Russian Federation and developing countries, the increase in the flow of tourists and specialists working abroad in hot climate zones, causes an increase in the number of people at risk of contracting tropical parasitic diseases and their importation into the territory of the Russian Federation.
Filariasis is a tropical helminthiasis caused by roundworms - filariae. Filariasis is characterized by a long incubation period, slow development of the disease and its long chronic course. Filariasis is contracted through the bites of blood-sucking insects.
Recently, cases of filariasis have been reported in the Krasnodar Territory. The causative agent of filariasis belongs to the class of roundworms Nematoda, order Spirurina, suborder Spiruromorpha, family Filarioidea, genus Dirofilaria. In total, several species of worms have been described, of which D. repens and D. immitis are the most common. They are the sources of the disease in most cases. The causative agents of the invasion, D. repens and D. immitis, are obligate parasites of the carnivorous families: canines and cats. D. tenuis affects raccoons, D. ursi occurs in brown bears and the Amur tiger, D. subdermata affects porcupines, D. lutrae and D. spectans - North American and Brazilian otters, D. striata - wild cats. This helminthic disease is most common in the countries of Southeast Asia and Africa. The development of the disease goes through an incubation period, which usually lasts several months. The clinic manifests itself with the formation of a small compaction in the area of dirofilaria introduction. Sometimes a slight and unnoticeable swelling develops in the area where the helminth is located. One of the features of this parasite is migration throughout the body of the host (carrier). During the day, dirofilaria is capable of migrating throughout the body up to 25-30 cm! Increased migration occurs when the skin is exposed to UHF currents during physiotherapy, as well as after warming with compresses or warming ointments.
The location of the skin seal also changes during migration, and no traces remain at its old location. Hyperemia of the skin and pain are usually not observed. An infected person may or may not feel the migration of the helminth itself - it all depends on the location of the parasite. Local manifestations in the form of a compaction or nodule are most often mistaken for neoplasms: atheromas, lipomas, cysts, most often an abscess. A patient with filariasis comes to the table of a surgeon, who, during the operation, detects and removes dirofilaria in the node. It should be taken into account that dirofilaria often likes to affect the organs of vision; during migration it enters the area of the upper or lower eyelid.
Subcutaneous filariasis in humans was first described in 1867 in Italy. The first case in Russia was diagnosed by A.P. Vladychensky in 1915. The nematode was isolated from a tumor located between the inner wall of the orbit and the eyeball. Although most helminthic infestations are characterized by eosinophilia in a general blood test, with filariasis the number of blood eosinophils remains unchanged, since dirofilaria does not cause sensitization of the body, and therefore the presence of this helminthiasis cannot be suspected.
Treatment of filariasis is surgical. Sometimes in the literature there are recommendations for taking anthelmintic drugs, but the effectiveness of such treatment is questionable.
This is not the first case of detection in the department of maxillofacial surgery of the Municipal Budgetary Institution “City Hospital No. 1” in Novorossiysk, as was previously reported in the journal “Dental South” (No. 4 (39), 2006. Authors: Head of the Department of Maxillofacial Surgery Elibekov V.G. , resident doctor Polishchuk A. A.; “A rare case of filariasis”).
On July 09, 2012, patient Ch., 59 years old, was delivered to our department from the hospital of the State Budgetary Infectious Healthcare Infectious Hospital No. 3 DZ KK, Novorossiysk, with a referral diagnosis of phlegmon of the right maxillary region. The patient was admitted to the Infectious Diseases Hospital with suspected trichenosis. The patient complained of swelling of the right half of the face, skin itching, and swelling in the parotid-masticatory area on the right. The patient explained during the interview that the swelling initially appeared in the right cheek area and moved to the zygomatic area on the right; at the time of examination, it was localized in the parotid-masticatory region at the level of the right earlobe. Upon examination, moderate swelling of the entire right half of the face is determined with the presence of a space-occupying formation in the tissues of the parotid-masticatory region on the right with a diameter of up to 1.5-2.0 cm, which rises above the level of surrounding tissues up to 0.5 cm. The skin over the formation is slightly hyperemic, palpation slightly painful. Within a radius of 1.5–2.0 cm, the tissues are slightly infiltrated, and fluctuation is also detected.
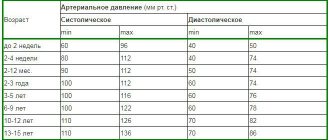
Blood test dated 07/10/12: Er - 4.03; Lake. - 6.4; Tr - 225; Hb - 127 g/l; P - 1, S - 62, L - 27, E - 10, M - 3. Urine analysis dated 07/10/12: color - s/f, beat. weight - 1010, complete transparency, reaction - acidic, salts - +, epithelium 2-4 in point of view; Lake. — 7-8 in point of view (Fig. 1-2).
Rice. 1
Rice. 2
Taking into account the patient's complaints, medical history and clinical data, a diagnosis was made: abscess of the parotid-masticatory region on the right. The patient underwent surgery: opening of the abscess under local anesthesia. During the operation, a worm and purulent exudate were identified. The find was sent to the laboratory, from where the answer was received - microfilaria (dirofilaria). The postoperative period is calm. The patient was discharged from the department with recovery. For informational purposes, photographic facts are provided below that allow a more complete understanding of the causative agent of the disease (Fig. 1, 2).
Patient P., 52 years old. East. b-ni No. 4407. She was hospitalized on March 25, 2013 for planned indications with a diagnosis of fibroma of the temporal region on the left. Upon examination, a volumetric increase in the tissues of the temporal region on the left is observed. Palpation reveals a dense, stiff, painless, round formation in the tissue thickness of about 2.0 cm. The skin over it is not changed in color, is not tense, and is not fused. On March 26, 2013, an operation was performed: removal of the formation under local anesthesia. The formation was located in the subcutaneous fat, its base tightly fused to the fascia of the temporal muscle. The tests performed during the outpatient examination were within normal limits. PGI No. 3891 dated 03/27/13 - helminthic infestation. Encapsulated bodies of parasites with a perifocal granulomatous reaction.
Conclusion
In connection with the increasing incidence of filariasis, here are several examples of hospitalization of patients affected by this disease. The purpose of this article is to familiarize colleagues with the clinical picture of filariasis, as well as to warn against incorrect diagnosis and treatment of this category of patients. Patients with filariasis are treated by various specialists: dermatologists (neurodermatitis, skin itching of unknown etiology), infectious disease specialists, therapists, ophthalmologists.
In particular, the patient mentioned in the article repeatedly contacted various specialists and was taken by ambulance with suspected angioedema. She was suspected of having trichinosis! We hope that the experience of our department will be useful to medical workers for the correct diagnosis and treatment of this disease.
- Avdyukhina T.I., Postnova V.F., Abrosimova L.M. et al. Dirofilariasis (D. repens) in the Russian Federation and some CIS countries: the situation and the trend of its change // Med. parasitol. - 2003. - No. 4. - P. 4448.
- Guide to Medicine. Diagnostics and therapy: In 2 vols.: Transl. from English / Ed. R. Bercow, E. Fletcher. - M.: Mir, 1997. - T. 1. - XXXIV + 1045 pp., ill. — P. 142.
- Bronstein A.M., Supryaga V.G. et al. Human dirofilariasis in the Moscow region // Medical Parasitology. - 2003. - No. 4.
- Grigorieva M.V. et al. Diagnosis and treatment of dirofilariasis of the testicular membranes in children // Bulletin of Infectol. and parasitol. - 2003; www.infectology/spb/ra; ISSN 16099877.
- Grigorieva M.V., Supryaga V.G. Features of diagnosis of cutaneous dirofilariasis // Problem of infection in clinical medicine. - St. Petersburg: Russian Military Medical Academy, 2002. - P. 342-343.
- Bronstein A. M., Supryaga V. G. et al. Human dirofilariasis caused by Dirofilaria (Nochtiella) repens is a new “emerging” infection in the Moscow region // Collection of abstracts for the conference dedicated to the 80th anniversary of the Department of Tropical Medicine and Epidemiology of the Russian State Medical University. - M., 2003.
- Vozianova Zh. I. Infectious and parasitic diseases: In 3 volumes - K.: Health, 2001. - T. 2. - P. 501-502.
- Grigorieva M.V., Dvorovenko E.V. Dirofilariasis of the testicular membranes under the guise of the syndrome of swollen and hyperemic scrotum // Pediatric surgery. - 2003. - No. 2. - P. 15.
- Yatskova G.N., Khropova M.L., Motorina G.A., Losikhin E.I. On the incidence of dirofilariasis in the Lipetsk region // Hygienic science and practice in addressing issues of ensuring sanitary and epidemiological well-being of the population in the Central regions of Russia: Scientific. works of the Federal Scientific Center of Hygiene named after. F. F. Erisman / Ed. acad. RAMS prof. A. I. Potapova. - Lipetsk, 2003. - Issue. 8. - pp. 552-554.
- Avdyukhina T.I., Lysenko A.Ya., Supryaga V.G. et al. // Bulletin of Ophthalmology. 1999. No. 3. P. 36-39.
- Postnova V.F., Abrosimova L.M., Kovtunov A.I. et al. // Medical parasitology. 1996. No. 4.
- Epshtein Sh. I., Lychmanov N. G. // Medical parasitology. 1954. No. 2. P. 175-176.
- Journal "Emergency Medicine" No. 1-2 (32-33), 2011. A case of diagnosing dirofilariasis using sonography Authors: Efimenko S. G., Lysenko V. V., Kharkov Medical Academy of Postgraduate Education, Kharkov City Emergency and Emergency Hospital medical care.
- Magazine “Dental South”, No. 4 (39), 2006. Authors: Head of the Department of Maxillofacial Surgery Elibekov V.G., Resident Doctor Polishchuk A.A. A rare case of filariasis.
Pathological anatomy
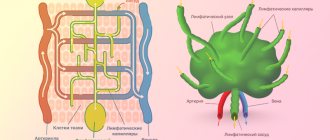
Pathological changes in filariasis are observed in various organs, which, however, are closely related to each other, namely, in the lymphatic vessels and glands, in the serous cavities and in the blood.
The lymphatic vessels and glands of the scrotum, inguinal, iliac and lumbar regions are the favorite location of the filaria. However, filaria can occur in other areas, especially in the vessels of the shoulder and forearm.
The origin of the changes caused by filaria is quite clear: the parasite, its embryos and eggs, which it lays in the lymph, clog the lymphatic trunks and cause varicose veins. Due to this, the lymph stagnates in the loops of the subcutaneous tissue, and then in the skin, which it irritates, and the result is a thickening and compaction of these parts, with or without the formation of lymphorrhagic effusion.
The amount of liquid in these effusions varies during the day from several grams to several hundred grams. It is white in color and alkaline, opaque, milky and coagulates when exposed to air. It contains many yellowish, strongly refracting light bodies, smaller in size than red blood cells, more voluminous white, nuclear and granular bodies, reminiscent of white blood cells, and, finally, many fatty grains suspended in a clear serous fluid. The chemical composition of the effusion: fibrin, albumin, fats and various salts.
Gland tumors in a fresh state also contain almost the same fluid. Under certain conditions, the latter is also found in some serous cavities, namely, in the vaginal membrane, in the cavity of the peritoneum and pleura. Chylous hydrocele of the testicle, almost always of parasitic origin, is usually symmetrical in nature and can reach the volume of a large pear. In chylous ascites, which is less often parasitic in nature, the effusion in the peritoneal cavity consists of a fluid resembling an almond emulsion and originating from the lymphatic vessels. Peritoneal effusion is rarely accompanied by pleural effusion, which then has the same properties. In all these effusions, filariae embryos may be found. Internal organs, with the exception of the testicles and kidneys, are most often not affected by filariasis.
Of all parts of the body, the blood is the place where filaria germs are predominantly found. This embryo, shaped like a small snake, moves quickly. Its body has a cylindrical shape, transparent, and the length (0.44 mm) significantly exceeds the thickness (0.003 mm). Its head end has an oblong or slightly elongated shape and is sometimes equipped with a point pellucida, which represents the oral opening, although it is difficult to distinguish the rudiment of the esophagus; the rear or caudal end, becoming thinner and thinner, ends pointedly. The movements of the parasite in the blood released from the vessel slow down and gradually stop.
The blood usually contains many filariae, since 30-40 of them are found in one drop.
Diagnostics
The following signs are used to diagnose filariasis: elephantine thickening of the tissue, mainly on the scrotum, soft swelling at the site of the inguinal glands with or without dilatation of the lymphatic vessels, hematochyluria and the presence of filariae in the blood. The first signs make the diagnosis probable, while the latter itself finally resolves the issue.
If there is elephantine degeneration of the genitals or even limbs, it is necessary to examine whether the blood at night does not contain filariae, since the presence of parasites can clarify the nature of the disease. The same must be done for endemic hematochyluria, which is caused by two different parasites: filaria and distomum haematobium. But if each of these parasites, localized in the kidneys or bladder, causes hematochyluria, then only one of them, namely, filaria, leads to swelling of the glands, dilation of the lymphatic trunks and chili-shaped effusions. Thus, the combination of these signs with hematochyluria is an important indication in favor of the existence of filariasis.
Microscopic examination of the blood makes it possible to avoid confusing parasitic swellings of the glands with hernias, wen, and erectile swellings of the inguinal veins. Equally important is the examination of urine, ascitic or other effusion for the content of parasites and determination of the type of the latter.
Treatment
Diethylcarbamazine (DEC) is the drug of choice for the treatment of lymphatic filariasis. This drug has strong parasiticidal activity against microfilariae, sometimes it also affects mature forms of the parasite. When used at a dose of 6 mg/kg body weight per day for 14 days, it significantly reduces the number of microfilariae. Treatment with diethylcarbamazine should begin with a low dose of 50 mg once a day, the next day increase to 150 mg per day in 3 divided doses, on the 3rd day - 300 mg per day in 3 divided doses, and from the 4th day you can use full dose. This reduces the risk of an increased allergic reaction to decaying microfilariae.
A drug with similar effects, which is mainly used in mass programs aimed at eradicating filariasis, is ivermectin, administered as a single dose of 150 mg per kg once a year. Albendazole is also effective in a dose of 2 times 400 mg for 10 days.
Improvement or inhibition of the progression of filariasis can be achieved by:
• hygiene;
• carrying out antibacterial treatment of superinfections;
• physiotherapy appointments;
• performing special exercises to improve lymph circulation;
• surgical removal of hydrocele.
WHO activities
In resolution WHA50.29, the World Health Assembly called on Member States to eliminate lymphatic filariasis as a public health problem. In response, WHO launched the Global Program for the Elimination of Lymphatic Filariasis (GPELP) in 2000.
The WHO strategy is based on two main components:
- stopping the spread of infection by providing large-scale annual treatment to all eligible people in areas where infection is widespread; And
- alleviating the suffering caused by lymphatic filariasis by providing the recommended package of basic health measures.
In 2021, the GPELF set the following targets included in the Roadmap for Control of Neglected Tropical Diseases:
- 80% of endemic countries meet the criteria for evidence of elimination of lymphatic filariasis as a public health problem, both in terms of stable infection rates below target thresholds for at least four years after the end of mass drug administration (MDT), and in the provision of all areas with identified by patients with a basic range of care services;
- 100% of endemic countries carry out surveillance at the end of the MFS or after confirmation of elimination; And
- The total population requiring MPL has been reduced to zero.
Extensive treatment (preventative chemotherapy)
Elimination of lymphatic filariasis can be achieved by stopping the spread of infection using prophylactic chemotherapy. WHO recommends mass drug administration (MDT) as a preventive chemotherapy strategy for eliminating lymphatic filariasis. The MPL consists of providing an annual dose of medicines to all people at risk. The drugs used have limited effect on adult parasites, but are effective in reducing the density of microfilariae in the bloodstream and preventing transmission of parasites to mosquitoes.
The recommended MPL regimen depends on the prevalence of other endemic filarial infestations along with lymphatic filariasis. WHO recommends the following MPL regimens:
- albendazole only (400 mg) twice a year in areas with endemic loiasis;
- ivermectin (200 mcg/kg) with albendazole (400 mg) in countries where onchocerciasis is common;
- diethylcarbamazine citrate (DEC) (6 mg/kg) and albendazole (400 mg) in countries without onchocerciasis.
Recent evidence suggests that a combination of all three drugs can reliably clear almost all microfilariae from the bloodstream of infected people in a few weeks, compared with years required with a conventional two-drug combination.
WHO currently recommends the following MPL regimen in countries without onchocerciasis:
- ivermectin (200 mcg/kg) in combination with diethylcarbamazine citrate (DEC) (6 mg/kg) and, under certain conditions, albendazole (400 mg).
The impact of MPL depends on the effectiveness of the regimen and the level of coverage (the proportion of the entire population receiving the drugs). The two-part MPL interrupts the transmission cycle of the parasite by repeating annually for at least 4–6 years and effectively covering the entire population at risk. In some special circumstances, salt enriched with DEC is also used to interrupt the parasite transmission cycle.
At the start of the GPELF, 81 countries were considered endemic for lymphatic filariasis. Subsequently revised epidemiological data concluded that 10 of these countries did not require preventive chemotherapy. Between 2000 and 2021, 8.2 billion treatments were administered to more than 923 million people at least once in 68 countries, significantly reducing the spread of infection in many places. Where infection prevalence fell below threshold levels, the population requiring MPT fell by 43% (648 million people). The total economic benefit from the program between 2000 and 2007 is conservatively estimated at $24 billion. It is estimated that treatment provided up to 2015 prevented at least US$100.5 billion in economic losses that could have been incurred over the lifetimes of the groups of people receiving treatment.
Currently 17 countries and territories (Wallis and Futuna, Vanuatu, Vietnam, Egypt, Yemen, Cambodia, Kiribati, Malawi, Maldives, Marshall Islands, Niue, Cook Islands, Palau, Thailand, Togo, Tonga and Sri Lanka ) are recognized as countries that have eliminated lymphatic filariasis as a public health problem. An additional five countries have successfully implemented recommended strategies, stopped mass treatment, and are being monitored to confirm disease elimination. Preventative chemotherapy is still required in 50 countries, and at the end of 2021, 10 of them had not all endemic areas covered with MPL.
Patient management
Case management and disability prevention are vital to improving population health and are essential services that a health system must provide to be sustainable. Surgical interventions can provide relief for most patients with hydrocele. Clinical severity and progression of the disease, including attacks of acute inflammation, can be alleviated and prevented by simple measures of hygiene, skin care, exercise, and elevation of affected limbs. People with lymphedema require ongoing care throughout their lives, both to control the symptoms of the disease and to prevent its progression.
The GPELF aims to ensure access to a minimum package of health interventions for every person with chronic lymphatic filariasis in all areas where the disease is prevalent, thereby helping to alleviate suffering and improve the quality of life of these people.
The 2030 targets will be successfully achieved if patients have access to the following minimum package of health measures:
- treatment of attacks of adenolymphangitis (ADL);
- guidance on simple measures to manage lymphedema to prevent disease progression and debilitating inflammatory attacks of ADL;
- surgical operations for hydrocele;
- treating infected people with antifilarial drugs.
Vector control
Mosquito control is another complementary strategy supported by WHO. It is used to reduce transmission rates of lymphatic filariasis and other mosquito-borne infections. Depending on the type of parasite that is carrying the parasite, measures such as using insecticide-treated bed nets, indoor spraying with residual insecticides, or taking personal protective measures can help protect people from infection. The use of insecticide-treated nets in areas where Anopheles is the main vector of filariasis increases the impact on transmission during and after MFP. Experience has shown that vector control in some areas has contributed to the elimination of lymphatic filariasis in the absence of large-scale preventive chemotherapy.
Forecast
The prognosis for filariasis is less unfavorable than one might think, judging by the significant number of filariae in the blood: these parasites change the blood little and do not affect important organs, on the proper functioning of which the body’s vital functions depend. The embryonic state of parasites and their inability to achieve full development in the human body make them relatively little dangerous, especially since some of them die if they are not excreted from the body after a certain time. The severity and outcome of filariasis is therefore determined solely by the number of adult filariae contained in the lymphatic system and the latter's predisposition to inflammatory lesions. By continuously flooding the blood with their embryos, adult filariae support the disease, so therapeutic efforts should be directed towards eliminating these adults.
Death, in fact, is rarely a direct consequence of filariasis, but is mostly the result of inflammatory lesions of the glands, lymphatic vessels or subcutaneous tissue.
The information presented in this article is intended for informational purposes only and cannot replace professional advice and qualified medical care. If you have the slightest suspicion that you have this disease, be sure to consult your doctor!
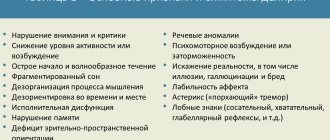
Symptoms
Invasion of lymphatic filariasis causes asymptomatic, acute and chronic conditions. Most infestations are asymptomatic and occur without external signs, thereby facilitating the transmission of the parasite. Such asymptomatic infestations still cause damage to the lymphatic system and kidneys and affect the body's immune system.
When lymphatic filariasis becomes chronic, lymphoedema (swelling of tissue) or elephantiasis (thickening of the skin/tissue) of the extremities and hydrocele (swelling of the scrotum) develop. The breasts and genitals are often affected. Such body deformities often cause social stigma, worsen mental health, and lead to loss of income opportunities and increased medical costs for patients and their caregivers. The socio-economic burden of exclusion and poverty is very high.
Against the background of chronic lymphedema or elephantiasis, acute attacks of local inflammation of the skin, lymph nodes and lymphatic vessels often occur. Some of these attacks are caused by the body's immune response to the parasite. Most of them are caused by a secondary bacterial skin infection, which develops due to a partial loss of the body's protective abilities as a result of disturbances in the functioning of the lymphatic system. These acute attacks are debilitating and debilitating, can last for weeks, and are a major cause of loss of income for people with lymphatic filariasis.