Ambulance for children : 8 (812) 327-13-13 More details
High temperature is the most common cause of parental concern about the health of children. Often, measuring body temperature helps determine what is happening to the child - he is simply in a bad mood or the baby is still sick.
Where, with what and how should the temperature be measured?
Body temperature can be measured in a variety of places - in the armpit, in the rectum, in the mouth, in the external auditory canal (by the way, this is not theoretical reasoning - temperature is measured differently in different countries). In Russia, it is customary to measure the temperature under the armpit - this is exactly what should be done, since each option for measuring temperature has its own normal numbers, and your Russian doctor is accustomed to focusing on the armpit temperature. In turn, being in another country, it makes sense to inform the doctor that the temperature was measured under the armpit. Today, along with the usual mercury thermometers, electronic thermometers have become widespread. If you are not a very neat person, it is better to use just such a thermometer - one broken mercury thermometer will not create problems, but if you are used to breaking them regularly, the level of mercury vapor in your apartment can reach levels that are hazardous to health. Many people complain about the electronic thermometer not working correctly - there are several tricks that will help you cope with this problem. First, having bought an electronic thermometer, you should check it by measuring your temperature simultaneously with an electronic and mercury thermometer - the permissible difference should not exceed 0.2 º. Secondly, especially when measuring the temperature of children, the sound of the buzzer should be ignored and the thermometer should be held for another minute - the result will be more reliable. A few words about the so-called ear infrared thermometers: their undoubted advantages include the speed of measurement - only two seconds. However, in this case, at best, you get the temperature of the eardrum - enough to track the temperature dynamics, but may not satisfy your doctor, because the difference between ear and axillary temperatures is not a constant value and accurate conversion is impossible. In the worst (and very common) case, the ear canal is filled with wax - and the numbers on the display of your thermometer will have very little relation to the child’s body temperature. The same can be said about remote infrared thermometers for measuring forehead temperature - their accuracy is also far from ideal. Among the “advanced” new products, you can pay attention to the so-called. “Xiaomi smart children's thermometer - a review of this fashionable device can be found here https://news.rambler.ru/other/38877929-obzor-detskogo-termometra-xiaomi-vse-zhivy/ reviews from real users about convenience and accuracy are not bad. It is not difficult to buy this device today, but everything sold is “gray” supplies, since this device today does not have mandatory certification in accordance with Russian requirements.
Thus, the most accurate is still the good old mercury thermometer. Everyone knows how to use it, however, I would like to dwell on a few points. First, if your child is sweating, you should dry the armpit first. Secondly, when placing the thermometer, you should make sure that its tip is under the armpit and not sticking out. Thirdly, you should keep the thermometer under your arm for at least five minutes. Sometimes these five minutes can become a difficult test for the parent’s psyche - some children categorically do not like the thermometry procedure. In this case, you can use grandma's old method - place the thermometer not from front to back, but from back to front. In this case, the child does not see the thermometer sticking out and often behaves calmer. There is a known method of measuring temperature that does not require a thermometer at all - many parents (and especially grandmothers) often claim that they are able to determine the child’s temperature with an accuracy of tenths by touching it with their hand or lips. I categorically do not recommend using this method - the point is not only that such statements are, to put it mildly, somewhat exaggerated. Unfortunately, this method gives maximum errors precisely when knowing the exact body temperature is especially necessary - with the so-called “pale” fever (we will talk more about this unpleasant condition later).
What temperature is considered elevated in children?
The concept of “normal temperature” in children is relative.
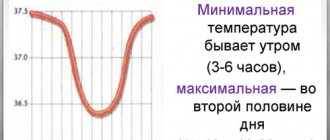
Its indicators are influenced by age, physical activity and emotional state, temperature and humidity of the environment. For example, in infants in the first months of life, a temperature of up to 37.5°C (measured in the axillary region) is considered normal, and in children under three years of age, the upper limit of normal is a temperature of 37.3°C.¹ The thermometer readings are also affected by the location of measurement temperature. In children it can be measured in four places:
- in the rectum (rectal);
- in the mouth (oral);
- in the ear (tympanic);
- in the axillary region (axillary).
For most parents, the usual place for measuring a child’s temperature is the armpit. In this case, the skin under the armpit should be dry. To measure the temperature, the child's hand must be pressed to the chest, placing the thermometer under the armpit.
A child’s axillary temperature is considered normal within the range of 35.8–37.0°C. If the temperature is measured in the rectum or ear, it is usually 0.5–0.6°C higher than the axillary temperature. The temperature in the mouth should be measured no earlier than 30 minutes after eating. It is 0.2–0.3°C larger than the axillary one.
To assess the temperature in children, mercury, galinstan, electronic and infrared thermometers are used. Each type of thermometer has its own advantages and disadvantages. The choice depends on the age of the child and the preferences of the parents. You can read more about thermometers here.
For children under three months of age, a reliable criterion for assessing temperature is the reading of a rectal electronic thermometer when measured for 30–60 seconds.
Thus, elevated temperature in a child can be considered:
- above 37.2°C - with axillary measurement;
- more than 38.0°C - when measured in the rectum or ear;
- more than 37.8°C - when measured in the mouth.
Depending on the degree of temperature increase, there are:
- subfebrile - fluctuations within 37.1–38.0°C;
- moderate febrile - 38.1–39.0°C;
- high febrile - 39.1–41.0°C;
- hyperpyretic - above 41.0°C.
We must remember and know about physical cooling methods
They can only be used for pink fever (skin is pink, moist, hot to the touch). The room should be cool, the air temperature should be 20-22 degrees for a better heat transfer process. You can use a fan, but you should act with caution, since cold air flows in children cause discomfort and crying. It is easier and more convenient to wipe the body with a napkin moistened with cool water, or use a vinegar wrap (1 tablespoon of 9% vinegar per 1 liter of warm water); for school-age children, wipe with vodka or alcohol diluted with water 1:1. These procedures must be carried out 4-5 times, which usually leads to a decrease in temperature by 0.5-1 degrees. Using a shared bath (10-15 minutes) with warm water is very effective. The water temperature should be 2-3 degrees lower than body temperature (for example, 38 at 40). The child’s well-being and mood improves before our eyes after such a procedure.
In case of white fever, physical cooling methods are contraindicated. The patient should be wrapped up, a heating pad can be applied to the legs and a hot drink and papaverine or no-shpu can be given (the dose depends on age), and at a temperature of 39 and above, a lytic mixture can be made or an ambulance should be called.
Medical sector specialist
N.I. Erofeeva
Causes of high temperature in children
The most common causes of high fever in children are infections (viral and bacterial).
Causative agents of infectious diseases contain exogenous pyrogens. When these biologically active substances enter the body, they can increase the temperature. Exogenous pyrogens cause the blood cells and some organs to produce endogenous pyrogens (interferons, interleukins). They rebuild the work of the hypothalamus, the thermoregulation center located in the brain. For this reason, fever occurs - an increase in temperature above 38 ° C in the rectum and above 37.5 ° C in the armpit, during which the body fights infection.
Fever itself is not considered dangerous. It occurs with various diseases, most often with bacterial and various viral infections, for example, ARVI or influenza. Moreover, in the first days of the development of infections, children may only have a high temperature without symptoms. There are also non-infectious causes of high temperature: tooth growth, overheating in the sun. We will only talk about the most common causes of childhood fever. Our short test will also help you better understand the symptoms.
Why is temperature beneficial?
- All biological, especially immune processes are activated. Pathogens lose their ability to reproduce and die.
- Protective reactions are stimulated - the rate of production of antibodies and interferons - internal antiviral agents - increases.
- The neutralization of toxins in the liver is activated.
- The elimination of urine, and with it toxins, is accelerated.
The most favorable temperature range for infections is considered to be 38-39 °C. With this course of the disease, it is enough to ensure that heat transfer corresponds to heat production. This is evidenced by the child’s relatively normal state of health: his skin is pink, warm and moist to the touch. Reducing the temperature is not recommended. Then the body can cope with the infection in the shortest possible time.
ARVI
ARVI is a viral infection affecting the upper respiratory tract. This is the most common cause of fever. ARVI is accompanied by a runny nose, nasal congestion, possible sore throat, change in voice, and cough. Modern international guidelines for doctors call ARVI a “self-limiting disease” and advise only to ease the child’s well-being and monitor the emergence of possible complications. Frequent complications of respiratory viral infections in children under 1.5 years of age are otitis media (inflammation of the middle ear) and laryngitis. Signs of laryngitis - hoarseness, barking cough - often occur at night and in the early morning. When they appear, you must definitely call an ambulance if the attack did not stop after inhalation with saline solution or Borjomi.
Herpesvirus infections
Herpes virus infections are caused by herpes simplex viruses types 1 and 2. The onset of herpetic infection in children is often accompanied by a temperature of 39–40°C and stomatitis (painful rashes on the oral mucosa, Fig. 1). This makes eating difficult and causes the child to refuse food.
Figure 1. Manifestations of stomatitis. Source: mrfiza / Depositphotos
Herpetic stomatitis most often occurs in children under three years of age. They are especially difficult for babies in the first month of life. In this case, small blisters may appear on a reddened base on the skin, mucous membranes of the mouth and eyes.
In children in the first month of life, herpes is often accompanied by inflammation of the brain and meninges (meningoencephalitis), since this virus “loves” to settle and multiply in the nervous tissue.
A type of herpes infection is EBV infection (caused by the Epstein-Barr virus or herpesvirus type 4). According to statistics, about 50% of children under the age of 5 years have already suffered from this infection.2 Fever, enlargement of all groups of lymph nodes (especially cervical), inflammation of the tonsils and the appearance of rashes after the use of penicillin antibiotics are its typical symptoms.
Childhood infections with rash
Children's infections with the presence of a rash are also called “infectious exanthemas.” Based on the nature of the rash, the doctor will make a diagnosis and determine the cause of the child’s fever. Infectious exanthemas include chicken pox, measles, sudden exanthema, scarlet fever.
Chicken pox
Chickenpox is a highly contagious disease with airborne transmission. It is caused by herpes virus type 3 (Varicella Zoster). The chickenpox rash is characterized by swollen pale pink spots with a vesicle in the center, its size is 1-3 mm. The main difference between this rash is that at the same time there may be spots, blisters and crusts on the body, since some are just appearing, while others are already passing.
The rashes are localized on the scalp, face, neck, torso, and limbs (Fig. 2); there may be elements of the rash on the mucous membranes of the mouth, throat, genitals, and sometimes in the eye area. After a few days, the blisters dry out and form crusts, which eventually break off on their own.
Figure 2. Chickenpox rash in a child. Source: pavsie / Depositphotos
The rash may be accompanied by itching. When combing them or tearing off the crusts, small scars form on the skin.
In most cases, chickenpox in children is relatively mild. The severity of chickenpox depends on the severity and duration of the fever. In severe cases, it lasts up to 14 days. Complications such as pneumonia and encephalitis (inflammation of the brain) are possible.
Measles
Measles is an extremely contagious viral infection. It is also called “childhood plague.”3 Despite mandatory immunization, the measles epidemiological situation in Russia cannot be considered favorable, since there is not a sufficient number of vaccinated people.4
The infection begins with respiratory symptoms against a background of high temperature: runny nose, sneezing, dry cough, swelling and inflammation of the eye mucosa, photophobia. From the second day of illness, small white spots with redness at the edges (Filatov-Belsky-Koplik spots) can be seen on the mucous membrane of the cheeks. On days 4–5 of the illness, a characteristic rash appears on the face, neck and behind the ears in the form of pink and red spots, which gradually spread from top to bottom and tend to merge (Fig. 3). Then they peel off, accompanied by light brown pigmentation. Measles is dangerous due to its complications. This can be pneumonia, otitis media, encephalitis with subsequent disability.
Figure 3. Measles: rash on the face, torso and arms (second day of the rash period). Source: PHIL CDC
Sudden exanthema
Sudden exanthema (infantile roseola, pseudorubella, sixth disease, three-day fever) is an infection caused by herpesviruses types 6 and 7. Children aged six months to two years are most vulnerable. As the disease progresses, rashes appear: small pink spots with maximum localization in the torso area. They turn pale when pressed and may itch. Before the appearance of roseola, a temperature of 38–40 ° C is noted without symptoms, and the posterior cervical and mandibular lymph nodes may enlarge.
Scarlet fever
Scarlet fever is a bacterial infection in which, in addition to fever, a sore throat develops and a rash appears, which is caused by the absorption of the pathogen's toxin, beta-hemolytic streptococcus. Scarlet fever rashes are bright red, 1–2 mm in diameter, slightly rough to the touch. Characteristic features include a “strawberry tongue” (with emphasized papillae) and pallor of the nasolabial triangle. In the axillary and inguinal folds, the color of the rash is more saturated.
After the rash resolves, slight peeling appears on the skin in the form of “thin layers” on the fingers and toes. 2–5 weeks after scarlet fever resolves, complications such as rheumatism, glomerulonephritis, and psoriasis are possible.
Enteroviral infections
About 100 varieties of viruses are known (Enterovirus, Coxsackie, ECHO, etc.), which cause outbreaks of diseases mainly in the summer-autumn period, during summer holidays at sea.
Signs of enterovirus infection vary among different types of enteroviruses. Enteroviral fever occurs like the flu, when there is a sharp fever and muscle pain, headache, nausea, vomiting, and diarrhea may appear. In some cases, herpangina develops - painful blisters appear on the oral mucosa.
With some types of enterovirus infections, a characteristic rash appears on the palms, soles and oral mucosa (hand-foot-mouth syndrome or viral pemphigus).
The intestinal form of enterovirus infections is accompanied by watery diarrhea up to 5–10 times a day, abdominal pain, and infrequent vomiting. In children under one year of age, this form of infection can cause dehydration.
Epidemic myalgia is also a manifestation of enterovirus infection. It is characterized by pain in the chest and abdomen, aggravated by breathing and coughing.
The most severe manifestations of enterovirus infections can be meningitis and encephalitis - brain damage with vomiting, convulsions, weakness in the limbs, and impaired consciousness.
Tick-borne encephalitis
Tick-borne encephalitis is a severe viral disease that occurs in areas inhabited by ixodid ticks (Siberia, the Far East, central Russia, Ukraine).
Infection occurs as a result of infection with the virus after being bitten or crushed by a tick. It is possible to get infected by consuming unboiled milk from cows, goats and sheep.
Clinical manifestations of the disease begin on average after two weeks, accompanied by a temperature of 38–40°C, headache, muscle aches, photophobia, discomfort in the eye area, oculomotor disorders, movement disorders, convulsions, and possible loss of consciousness.
Tick-borne encephalitis can cause irreversible health problems. To prevent the disease in endemic areas, immunoprophylaxis with a vaccine and specific immunoglobulin is used.
Bacterial infections
Among the pathogens in children, the most important are Escherichia coli, beta-hemolytic streptococcus, staphylococcus, pneumococcus, Haemophilus influenzae, salmonella, and enterobacter. These pathogens cause bacterial pneumonia, infections of the skin and subcutaneous tissue, genitourinary tract, and intestines. The most common cause of a high fever in an asymptomatic child is a bacterial urinary tract infection.
Non-infectious causes of high fever
Non-infectious causes of high fever are less common. They can be presented:
- Reactions to various medications and vaccines. Among such drugs, antibiotics and sulfonamides are in the first place, as well as vaccines against whooping cough, measles and influenza, pneumococcus, and tuberculosis.
- Autoimmune diseases: lupus erythematosus, vasculitis, juvenile arthritis, ulcerative colitis (inflammatory bowel disease).
- Dysfunction of the central nervous system against the background of traumatic brain and birth injuries, cerebral hemorrhages, prolonged psycho-emotional stress.
- Teeth growth.
- Overheating in the sun.
In some cases, the cause of high temperature is malignant tumors (leukemia, lymphoma).
How to care for a sick child at home
For a child with a fever, it is important to create a comfortable environment at home. You should not dress him warmly or wrap him up (except during periods of severe chills); he should be ventilated: the temperature in the room should be 20–22°C.
An ill child becomes lethargic or restless and refuses to eat or drink, which can lead to dehydration with a fever. Therefore, it is important to give your baby water as often as possible. To do this, it is better to use warm or cool compotes, fruit drinks, diluted juices, jelly, and weak tea. Children under two years old should drink about 1 liter of liquid per day, older children - 1.5–2 liters. If your baby is breastfed, you need to put him to the breast more often.
At high temperatures, it is important to maintain a drinking regime. Photo: lia_russy / Depositphotos
An indicator of adequate drinking is passing light-colored urine every 4 hours. It is necessary to monitor the child so as not to miss important symptoms and consult a doctor in a timely manner. Walking and washing a feverish baby should not be done in cases where it makes the child feel uncomfortable.
When to lower the temperature
Fever itself is not a disease, but a protective reaction of the body, which is aimed at fighting viruses and bacteria.
The numbers on the thermometer are not always considered a criterion for the use of antipyretics.
An antipyretic should be given in cases where:
- the child feels unwell, cannot sleep, is capricious, and complains of a severe headache;
- there is a chill, the child is trembling, the skin has become pale, with a marbled tint;
- there are diseases of the nervous system, metabolic and heart diseases;
- child under one year old, premature;
- against the background of elevated temperature, the baby developed convulsions (or such a condition was observed in the past).
“There is no universal number on a thermometer before which the fever should not be reduced. It is more correct to focus on the baby’s well-being: if his temperature is 39.3°C, but he is already feeling hot and sweaty, you don’t have to give an antipyretic, the temperature will drop on its own. If it’s 37.2°C, but he’s shaking a lot with chills, don’t wait for any conventional numbers, give the drug. Remember that there is no goal to bring the temperature down to 36.6: it was 40.3, it became 38.9, but the child came to life, he felt better - this is a good sign and a sufficient effect.” An excerpt from the book by pediatrician Sergei Butria “Child's Health. How to learn to cope with illness and your own panic.”
How to reduce a child's temperature
The best choice of antipyretics for children is paracetamol or ibuprofen. Suspension or syrup forms of these drugs are more acceptable for children. It is also possible to use the products in rectal suppositories, especially if the child is vomiting.
Parents should carefully read the instructions for medications and monitor the dosage of medications. Thus, a single dose of paracetamol is 10–15 mg per 1 kg of child weight. The maximum permissible frequency is 4 times a day. Ibuprofen can be given no more than three times a day. Single dose: 5–10 mg per 1 kg of body weight.
Antipyretics do not need to be given regularly throughout the entire period of fever, especially against the background of antibiotics. It is not recommended to use 2 drugs at the same time and reduce the temperature to normal levels. If “white fever” occurs, when the skin is pale and the child’s hands and feet are cold to the touch, you can rub your palms and soles.
How to take antipyretics correctly?
Antipyretic drugs , mainly paracetamol (Efferalgan, Paracet, Panadol, Cefekon, Tylenol) and ibufen (ibuprofen, Nurofen, MIG 400), also have anti-inflammatory and analgesic effects, but have a number of side effects (including toxic ones). You should remember this and use them correctly: no more than 4 times a day, every 6 hours, if possible after meals, with plenty of water. It is best to alternate antipyretics (if you used paracetamol this month, then next month it is better to use ibufen, or change medications every other day). Many people think that paracetamol does not help. This is primarily due to the dosage, which must be clarified with a doctor. In addition, antipyretics should be taken only at a temperature above 38.5-39 in the first three days of ARI, since taking these drugs at a lower temperature stops the production of its own interferon, lysozyme and turns off other immune mechanisms, which sometimes contributes to the development of complications. Children under one year of age who are under the supervision of a neurologist and who have a history of seizures or recent traumatic brain injury should be given an antipyretic at a temperature of 37.5. In addition, the antipyretic can also be taken at low temperatures; if the child does not tolerate it well (severe lethargy, headache), then in this case it is better to reduce the dose.
What to do if medications don't help
Sometimes parents are faced with a situation where taking one antipyretic does not have an effect. If, 2 hours after taking the medicine at the required dose, the temperature has not decreased, another antipyretic drug should be given.
“You can combine means. For example, give the child an antipyretic, an antispasmodic and some antiallergic drugs. An antispasmodic will dilate peripheral blood vessels, an antihistamine will relieve swelling, and an antipyretic will reduce the temperature. These are the three drugs that are included in the injection that the emergency doctor gives. If a child has a high temperature, it is advisable to alternate ibuprofen and paracetamol so as not to exceed the daily dosage. First give ibuprofen, after 4-6 hours paracetamol, then again after this interval ibuprofen and so on.”
Kovalchuk Maria Sergeevna
expert
UZ "GSSMP Minsk"
30 minutes after taking paracetamol or ibuprofen, you can wipe down with water at room temperature. In this case, the skin should dry on its own. A decrease in temperature of 1–1.5 degrees is enough to stop the procedure.
If no effect occurs, you should call an ambulance (Fig. 4).
Figure 4. What to do if a child has a high temperature. Source: MedPortal
When to call a doctor or ambulance
The reasons for being examined by a doctor in the near future should be:
- Child's age is up to 6 months.
- Risks of dehydration: diarrhea, vomiting, inability to maintain adequate drinking regimen.
- The appearance of a rash on the skin, which may indicate a certain disease or an allergic reaction to drug therapy.
- High fever without symptoms for three days.
- Deterioration of the child’s well-being and resumption of fever after temporary improvement. In this condition, there are likely risks of complications from viral infections.
It is necessary to call an ambulance if you observe:
- fever in children under three months, since the risk of severe infections at this age is high;
- convulsions;
- atypical sleep or atypical prolonged crying, agitation;
- uncontrollable vomiting, profuse diarrhea for more than 1-2 hours, signs of dehydration: dry diapers, dry tongue, sunken eyes;
- intermittent, difficult or too infrequent breathing;
- a rash on the skin that does not turn pale when pressed, similar to hemorrhages;
- stomach pain and severe headache;
- bulging fontanel;
- inability to press your chin to your chest (a symptom of meningitis).
If the high temperature does not go down or increases, despite all the measures taken (drinking plenty of fluids, taking two antipyretics, wiping with water), calling an ambulance is also necessary.
How long does the temperature last?
Now we will try to answer the question regarding how long a child’s temperature lasts during ARVI and some other diseases, and we will also find out what determines the duration of recovery.
The duration of the disease, in which the baby has a fever for more than 6 days, can be determined by several factors1,2.
- Symptoms and form of the disease . For example, purulent tonsillitis occurs in a more severe form than catarrhal and is accompanied by elevated temperature.
- The immune system . If it is strong, then even with a severe viral infection, the baby’s condition can stabilize in about 3-4 days.
- Age . The smaller the child, the longer his recovery from ARVI will be.
We draw your attention to the fact that only a doctor can identify the cause of a child’s elevated body temperature and prescribe the necessary treatment. Before the doctor arrives, provide your baby with plenty of fluids, calm him down and put him to bed.
Up to contents
What is better not to do
No matter how severe a fever may be, parents should always remember that some medications can cause more harm than the disease itself. Aspirin is not recommended for antipyretics for children under 12 years of age, especially for chickenpox and influenza. This is due to the likelihood of developing Reye's syndrome, a rare life-threatening condition that causes cerebral edema and acute liver failure. Children under 12 years of age should not be given analgin in tablets, only in the form of an injection.
Nimesulide preparations, which have proven themselves as antipyretics in adults, are prohibited for use in children under 12 years of age due to the risk of toxic effects. The same applies to analgin.
Antibiotics and sulfa drugs can only be prescribed by a doctor. They are only effective against bacterial infections, and most causes of fevers in children are related to viruses.
A big misconception among parents is the use of all kinds of immunomodulators and antiviral drugs in children with ARVI. The use of specific antiviral drugs is justified only for influenza and some herpetic infections.
You should not apply cold objects to the body of a feverish child, as this provokes vasospasm. Rubbing with vinegar and alcohol solutions is also not necessary due to the possibility of toxic substances being absorbed through the skin. With “white fever”, when the skin becomes pale, the extremities are cold to the touch, there is chills, rubbing is undesirable, as it can increase vascular spasm.
Kovalchuk Maria Sergeevna
Emergency doctor
Wipe your child with water at room temperature, or even a little warmer - 20-25°C. Do not use hot or cold water and do not add anything to it, neither vinegar nor alcohol. Wipe your neck, armpits, groin folds, under the knees and palms. Let the water dry and repeat wiping several more times. When the water evaporates, heat exchanges with the environment and the child’s temperature decreases without pills.
RINZASIP® for children – a multi-component remedy for alleviating the symptoms of ARVI and influenza
To reduce the severity of negative symptoms of the infectious-inflammatory process and the subsequent progression of colds, a complex drug RINZASIP® was created for children from 6 years of age6. This product, produced in the form of a powder for preparing a raspberry hot drink*, contains 3 active ingredients: paracetamol (280 mg), ascorbic acid (100 mg) and pheniramine (10 mg)6.
Paracetamol has a good antipyretic and analgesic effect, pheniramine has antiallergic properties, relieves swelling and hyperemia of the mucous membrane, helps eliminate nasal congestion, and vitamin C (ascorbic acid) regulates redox processes, supports immunity and increases the body's resistance to infection6.
The powders, packaged in sachets, have a pleasant taste. RINZASIP® for children can be given to a child from 6 years of age to normalize the condition of colds, toothaches, headaches, and rhinitis of allergic origin6. Taking a complex drug at the earliest stages of colds and flu helps prevent their development and alleviates the condition of the little patient.
Up to contents