Streptoderma
is a skin infection provoked by streptococcus - the culprit of sore throat, scarlet fever, bronchitis, meningitis, pneumonia. It is characterized by the appearance of areas with bubbles and blisters, as they mature, crusts form, as well as flaky spots, wounds that do not heal for a long time, periodically drying out and oozing again. The incubation period is 7-10 days.
This infection is very popular in warm and humid climates - in the southern regions the number of registered cases is 20% higher than in the Central Federal District and northern regions. Most often, streptoderma occurs in children, but cases are also common in adults. Every 50th child under the age of 7 encounters it.
Causes of streptoderma
Streptococcus is an opportunistic bacteria that is constantly present on the skin. Due to the structural features of the latter, streptococci cannot penetrate inside the skin. But as soon as a wound, abrasion, crack appears, or the immune system weakens, the path is open. In children, streptoderma occurs more often due to immature immunity, in adults when it is weakened after surgery, serious illness or injury. The main causes of streptococcal activity include the following.
- Damage to the skin.
The slightest wound, scratch, abrasion, scratched mosquito bite, not to mention postoperative sutures are the entry point for infection.
- Hormonal disorders.
During normal operation of the endocrine system, hormones are produced in the required quantities, regulating metabolism, growth and development of the body, and overall health. Hormonal imbalance causes negative changes in the skin:
- For thyroid dysfunction
– dryness, peeling, increased sensitivity of the skin;
- For inflammation of the pancreas
– pallor, clearly visible vascular network, long-term non-healing wounds;
- For ovarian or testicular dysfunction
– increased greasiness or dullness of the skin, loss of elasticity.
All of the above factors contribute to frequent skin injury.
- Changes in the acid-base balance of the skin (ph).
The dermis contains sebaceous glands that secrete substances involved in creating a protective barrier. Their relationship with dead cells determines the ph level. In a healthy person it fluctuates in the range of 5.2-5.7 units. With such indicators, a reliable barrier is formed that effectively protects against penetration of pathogenic microorganisms through the skin. At normal pH, cuts and abrasions heal quickly and wounds heal. But a sharp change in the acid-base balance of the skin radically changes the picture. Streptococcus multiplies quickly when the pH level increases to 6-7.5 units.
- Predisposition to allergic dermatitis.
The appearance of rashes, plaques, wounds, itchy spots leads to a violation of the acid-base balance of the skin, its scratching, and loss of integrity. All this creates a favorable environment for the proliferation of streptococcus.
- Chronic diseases.
Disturbances in the gastrointestinal tract, endocrine, cardiovascular systems, unbalanced nutrition, severe and prolonged stress, vitamin deficiency lead to a decrease in immunity. The body simply does not have the strength to protect itself from external influences, including bacterial ones.
Whatever the symptoms of streptoderma, treatment should be comprehensive - that is, aimed at eliminating the focus, blocking streptococcus and strengthening the immune system. With simultaneous exacerbation of chronic diseases, treatment for this profile is prescribed in parallel. It is important to eliminate not only the consequences of streptococcal activity, but also its causes.
Nature and causes of skin lesions
The disease primarily affects smooth areas and skin folds, with lesions prone to peripheral growth. Typically, the disease does not affect the sebaceous and sweat glands, hair follicles. The localization of lesions can be on any part of the body - on the skin of the extremities, face and scalp, torso, groin or gluteal fold, etc.
The infection affects people of all ages, and in adults it occurs most often among workers in the construction, transport, metallurgy and mining industries, for whom it is often considered an occupational disease. Streptococci in an inactive state are present in the bodies of the vast majority of people, but the most common causes of streptoderma in adults are:
- reduced immunity combined with massive transmission of infection from a sick person;
- minor skin injuries that contribute to disruption of its barrier function;
- dysfunction of the central nervous system due to stress or fatigue, leading to decreased immunity, deterioration of tissue trophism and blood circulation;
- the presence of a chronic endocrine disease, which increases the risk of developing purulent-inflammatory processes;
- taking certain medications that reduce the body's resistance to streptococcus;
- disturbances in the composition of the intestinal microflora due to poor nutrition, leading to inhibition of the function of intestinal immune cells;
- failure to comply with personal hygiene rules, which creates favorable conditions for the growth of bacteria.
In children, streptoderma most often develops in the preschool period and accounts for up to 60% of pustular skin lesions. Bacteria are usually transmitted through household means; the development of infection is facilitated by the presence of small wounds, abrasions or scratches, and insect bites.
Symptoms of streptoderma
In adults and children, foci of streptoderma occur on the face, arms, legs, in the groin or armpit area, behind the ears, between the buttocks, and in the inframammary fold. Localization can be localized - only one outbreak in one place or mass - several outbreaks in different places.
The main symptoms of streptoderma:
- Flaky, round spots from pink to bright red, often with a yellowish crust;
- Families of bubbles (flykten) with an area from several millimeters to two centimeters;
- Severe dry skin – you constantly want to lubricate and moisturize it;
- Enlarged lymph nodes;
- Swelling and pain in the affected areas;
- Itching and fever up to 38;
- General malaise, weakness;
- Headache;
- Aches in muscles and joints;
- Violation of hygiene rules;
- Diaper rash in bedridden patients.
The first three symptoms are characteristic only of streptoderma, the rest are characteristic of most inflammatory diseases of an allergic and endocrine nature.
Stages and forms of streptoderma
The first streptococcal sores appear on the smooth skin of the mouth and nasal cavity. Further, the lesion grows; when scratched, the pathogen remains on the hands and is transferred to other areas of the skin. Streptococcus is very tenacious and contagious. It is transmitted by contact. In adults, it causes the following forms of streptoderma.
- Streptococcal impetigo.
A rapidly growing bubble forms at the site of the initial redness. Then it bursts, and in its place a yellowish crust appears, outlining the affected area.
- Bullous impetigo
. It manifests itself in the form of a rash of blisters with serous-purulent filling. This rash “loves” the legs, feet, and hands. As they ripen, the bubbles burst, the liquid pours out, after which crusts form.
- Jams.
These are redness in the corners of the mouth, in place of which serous-purulent blisters form. After they mature and peel off the crusts, sore, hyperemic marks and cracks remain.
- Tourniol
. This is the name for streptococcal infection of the nail folds, which is expressed in the formation of serous blisters around the nails. Purulent erosions occur at the site of their perforation.
- Diaper rash.
They form in skin folds and begin with small conflicts. Then they grow, occupying vast areas. After the bubbles mature, marks of a characteristic shape and bright pink hue remain in their place.
All of the above forms are superficial and respond well to treatment. The greatest danger is streptococcal ecthyma - a deep form of streptoderma, which affects the deep layers of the skin. After the blisters mature and the crusts die off, erosions form on the skin, leaving behind scars.
Kinds
Streptococcal impetigo
- the most common type, skin rashes on the cheeks, around the mouth, on the lower jaw, in the nose and ears.
Ringworm simplex
- occurs more often in children (on the face).
Bullous impetigo - localization sites: arms, legs, feet, back, abdomen. The maturation of the purulent bladder is slow, painful, and septic complications are possible.
Angular stomatitis, slit-like impetigo, streptoderma of the corners of the mouth or mouth
- a type of disease known to many people.
Streptococcal diaper rash
- occurs on contacting surfaces (in skin folds), mostly in young children and adults with diabetes, obesity, atopic dermatitis, hyperhidrosis.
Tourniol, superficial felon, nail fold impetigo
- inflammation of the periungual plates.
Ecthyma vulgaris
- a large abscess, often in the area of the legs, leaves behind scars.
Dry streptoderma
- similar to ringworm, large rashes leave scars.
Diagnostics
Only a doctor should diagnose and prescribe treatment for streptoderma.
- A dermatovenerologist takes an anamnesis and conducts an external examination.
- A bacteriological examination and bacteriological culture of the contents of the papules are carried out.
- The sensitivity of streptococcus to antibiotics is determined.
- If necessary, additional blood, urine, and stool tests are prescribed.
- Consultation with an endocrinologist may be required.
Diagnosis of streptoderma
You shouldn’t rely on chance and herbs, which have been used to treat all kinds of skin diseases since ancient times. In the absence of proper treatment, itchy and bursting sores lead to serious complications, including glomerulonephritis and rheumatism. Timely and high-quality diagnosis allows you to correctly identify the symptoms of streptoderma.
- Visual inspection.
An attentive doctor records all visible manifestations of infection. It is difficult to confuse streptoderma with other skin diseases.
- Anamnesis collection.
Complaints, information about chronic and recent inflammatory infectious diseases, living conditions, contacts with infected people, and bad habits are important.
- Bac sowing.
For scraping, they take the discharge from the wound, inoculate it in a nutrient medium and determine the specific pathogen - streptococcus or not. At the same time, its sensitivity to antibiotics of various groups is revealed. If there are problems with blood vessels, reduced immunity and its obvious deficiency, bacterial culture is contraindicated.
- Additional research.
These include OAC and OAM, detailed blood biochemistry, blood analysis for thyroid hormones, Wasserman reaction, HIV, and helminth testing. The activity of streptococcus is confirmed by high ESR, leukocytosis, and C-reactive protein.
Many doctors make a diagnosis based on the first three points. Rarely does anyone prescribe treatment for streptoderma after a full course of examinations.
Diagnostic methods
To diagnose streptoderma, the doctor does not limit himself to examination and history taking, since external signs of the disease can easily be confused with other skin infections. To obtain accurate data, the patient is prescribed:
- microscopic examination;
- bacterial culture is the most informative research method, which allows not only to detect the causative agent of infection, but also to establish its pathogenicity, and also to check how sensitive it is to antibiotics.
Both tests are prescribed only if the patient has not used antibiotics or other medications. The patient may need to consult an endocrinologist if he has diabetes or is suspected of having this disease.
Treatment of streptoderma
The program and duration of treatment directly depends on the severity and form of the disease. With the right approach, it does not take more than 10 days. These are necessarily local preparations for direct treatment of the affected areas, antibiotics for oral administration, physiotherapy and folk remedies.
Antiseptic treatment of lesions
It is produced using antiseptic agents. They treat the affected areas, disinfecting, preventing the spread of infection and drying the wounds. It is important to apply antiseptic not only to them, but also to surrounding areas. To speed up healing, you can pierce the conflicts with preliminary disinfection of the needle and cauterize the wounds with an antiseptic.
As the latter, such popular remedies as brilliant green, potassium permanganate, fucorcin, hydrogen peroxide, and salicylic alcohol are often used. But, each of them has its own side effects in the form of burning, subsequent dryness and tightness of the skin.
The best option for antiseptic treatment of streptococcal lesions is the pharmaceutical drug Rivanol 0.1%. This is a time-tested disinfectant composition that does not cause discomfort when used even on open wounds. It is worth noting that Rivanol leaves marks on skin and clothing, so it requires careful handling. But it effectively blocks and destroys pathogenic bacteria and quickly restores the skin.
You need to treat conflicts with an antiseptic several times a day. If the skin in their place is roughened, it is recommended to lubricate it with salicylic petroleum jelly. Such procedures will have to be repeated until the skin is completely cleared of traces of streptoderma.
Antibiotic therapy
It is prescribed only based on the results of bacterial culture - you need to find out which antibiotic can suppress the activity of pathogenic microflora. Penicillin drugs are most effective in the fight against streptococcus, but they have their own contraindications and side effects. In addition, in most cases, along with streptococcus, other bacteria also “work” on the skin.
Depending on the severity of the condition and medical history, the doctor prescribes local or systemic treatment.
- Local.
It involves applying antibiotic ointments. This is done 2-3 times a day. The ointment relieves inflammation, suppresses infectious activity and ensures wound healing.
- Systemic.
Along with local medications, antibiotics are prescribed for oral administration for a course of 5 to 14 days. The specific drug and its dosage are determined by the doctor individually. Taking antibiotics is also accompanied by the prescription of antihistamines, means to maintain normal functioning of the gastrointestinal tract, as well as measures to strengthen the immune system.
It is not recommended to purchase and take antibiotics locally and orally on your own - streptococcus is not sensitive to all drugs. What worked well once may turn out to be ineffective or ineffective now.
Immunomodulators
In case of a protracted course of the disease, the doctor will prescribe drugs with an immunomodulating effect. Usually these are intramuscular injections such as pyrogenal, neovir, levamisole. They significantly increase the body's resistance and help quickly defeat infection.
In case of a standard, not advanced course of streptoderma, vitamins of groups A, B, C, E and P are prescribed in parallel with the main course of treatment.
Physiotherapy
UV irradiation helps suppress the activity of pathogenic microflora. Ultraviolet light has a detrimental effect on streptococcus, quickly drying the affected areas and promoting skin regeneration.
Traditional methods
As an addition to the main course of treatment, it is recommended to make lotions and treat the affected areas with infusion of oak bark, sage, chamomile, and string. This should be done after antiseptic treatment (but not immediately, but at least after 15-20 minutes) and in between applying antibiotic ointment. The above compositions have a pronounced anti-inflammatory, antiseptic, and wound-healing effect.
External therapy for pyoderma in children
Pyoderma is the most common skin disease in all age groups. Bacterial skin infections are an interdisciplinary problem; they are encountered in the practice of surgeons, therapists, pediatricians, and gynecologists. Despite the obvious successes in the development of methods for treating pyoderma, in pediatric practice certain difficulties may arise in developing a treatment algorithm due to the structural features of children's skin and the spread of sensitization to many drugs. In addition, the widespread use of antibiotic therapy has led to the spread of multi-drug resistance.
In this regard, drugs for external use that are sufficiently effective and tolerable are attracting special attention. These include fusidic acid [1].
The drug belongs to drugs with a bacteriostatic type of action; in high doses it exhibits a bactericidal effect against the most sensitive microorganisms. Fusidic acid inhibits protein synthesis in a microbial cell at the ribosome level; it interacts with the so-called microbial cell elongation factor (elongation factor G, in prokaryotes - protein type 2), which is necessary for the process of translocation on the ribosome during the formation of peptide bonds. Under the influence of fusidic acid, a complex of the elongation factor with organic phosphates of the cell is formed, the function of the elongation factor, the hydrolysis of guanosine phosphates are disrupted, and the process of lengthening the peptide bond and protein synthesis stops. Fusidic acid does not interfere with protein synthesis in eukaryotic cells. Bacterial resistance to fusidic acid develops quite rarely and slowly and, despite long-term use of drugs, has no clinical significance. Among methicillin-sensitive and methicillin-resistant staphylococci, strains resistant to fusidic acid are registered in various countries in the range of 1–6%. In Russia, as a rule, sensitive strains are isolated. In recent years, the drug has become of primary importance in the treatment of infections of staphylococcal and streptococcal etiology, as it is effective against most multidrug-resistant strains.
Previously presented observations showed the effectiveness of fusidic acid in pyoderma [1], and in combination with topical glucocorticoids in allergic dermatoses, accompanied by a significant spread of pathogenic microflora [2–5]. Evidence has been provided of the safety of the use of drugs containing fusidic acid [4, 5].
In clinical practice, drugs containing fusidic acid are used: Fucidin ointment and cream, as well as combined with topical steroids: Fucicort ointment and cream (with the addition of betamethasone valerate), Fucidin G cream (with the addition of hydrocortisone).
The purpose of this study was to study the clinical effectiveness and safety of drugs containing fusidic acid in pediatric practice.
Materials and methods
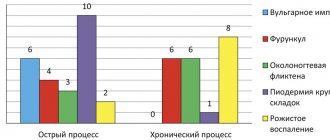
We observed 56 children aged 4 to 14 years, including 32 girls and 24 boys. Diffuse streptoderma was diagnosed in 12 patients, vulgar impetigo - in 11 (in 6 children - developed against the background of allergic dermatitis, in 5 - against the background of toxiderma), atopic dermatitis complicated by streptostaphyloderma - in 33 patients.
Two children suffering from diffuse streptoderma were previously prescribed synthomycin emulsion, but no therapeutic effect was noted. Patients suffering from vulgar impetigo had previously received antihistamines and desensitizing agents internally, and topical glucocorticoids externally, without any significant effect. All patients suffering from atopic dermatitis had previously received repeated courses of antihistamines, desensitizing agents orally and parenterally, externally - topical glucocorticoids, aniline dyes - with a short-term therapeutic effect. Ten patients had not previously received any therapy.
In all cases there were characteristic external clinical signs of the listed diseases. Patients with vulgar impetigo and atopic dermatitis complained of itching in the lesions.
Patients suffering from diffuse streptoderma were prescribed Fucidin G cream for lesions on the face, and Fucidin ointment for other areas of the skin (torso, arms, legs).
Patients suffering from vulgar impetigo and atopic dermatitis received antihistamines and desensitizing agents. Fucidin G cream was prescribed externally for lesions on the face, and Fucicort ointment was prescribed for other areas of the skin (torso, arms, legs).
During therapy, the tolerability and effectiveness of treatment, as well as peripheral blood and urine parameters were assessed.
results
Direct application of external agents containing fusidic acid was not accompanied by negative emotions or anxiety in children throughout the entire course of therapy.
By the end of the 3rd day from the start of therapy, all patients showed regression of pyococcal rashes and a decrease in subjective sensations. On the 10th day of therapy, all patients suffering from diffuse streptoderma and vulgar impetigo showed recovery. Significant improvement was noted in 16 patients suffering from atopic dermatitis, and improvement in 17.
All the children we observed tolerated the treatment well; no adverse reactions or adverse events were noted. No negative effects of therapy on peripheral blood and urine parameters were noted.
Discussion
The presented results confirm the high effectiveness and safety of fusidic acid for pustular skin lesions. The use of various dosage forms containing fusidic acid was characterized by high compliance.
In all cases of diffuse streptoderma, recovery was achieved as a result of monotherapy.
The use of combination drugs in complex therapy has made it possible to achieve recovery in vulgar impetigo and pronounced positive results in such severe chronic dermatosis as atopic dermatitis.
For pediatric practice, the ability to choose different dosage forms of the drug is especially important. Thus, Fucidin ointment was effective when prescribed to lesions of diffuse streptoderma on the torso, arms, and legs. The use of a non-halogenated topical steroid with a high level of safety - hydrocortisone in combination with fusidic acid (Fucidin G cream) made it possible to achieve positive results when prescribed to lesions on the face of children with diffuse streptoderma, vulgar impetigo, and atopic dermatitis. For severe itching that accompanied atopic dermatitis on lesions on the torso, arms, and legs, the use of Fucicort ointment was effective.
The course of treatment was 10 days; to achieve therapeutic results, no additional administration of antibacterial drugs orally or parenterally was required.
On the other hand, the achieved therapeutic effect indirectly proves the absence of resistance of staphylococcal and streptococcal skin microflora to fusidic acid.
Good tolerability of both monotherapy and complex treatment using fusidic acid was noted.
Conclusion
Analysis of literature data and our own observations indicate the high safety and effectiveness of external products containing fusidic acid. In pediatric practice, it is advisable to use various dosage forms, taking into account the clinical picture and localization of the process.
conclusions
- For primary and secondary pyoderma in children, the use of drugs containing fusidic acid is effective and safe.
- For diffuse streptoderma, monotherapy with fusidic acid preparations is effective; for vulgar impetigo and atopic dermatitis, complex therapy using antihistamines and desensitizing agents is effective.
- Depending on the clinical manifestations and localization of lesions, the appropriate dosage form should be selected. Thus, it is advisable to use Fucidin G cream for lesions on the face; for lesions on the torso, arms, legs - Fucidin ointment for pyoderma; for atopic dermatitis - Fucicort ointment.
Literature
- Schofer H., Simonsen L. Fusidic acid in dermatology: an updated review // Eur. J. Dermatol. 2010, Jan-Feb; 20 (1), p. 6–15.
- Veselova L.V., Khamaganova I.V., Savina M.I. Treatment of allergic dermatoses // Doctor. 2007, no. 2, p. 35–38.
- Alsterholm M., Flytstrom I., Bergbrant IM, Faergemann J. Fusidic acid-resistant Staphylococcus aureus in impetigo contagiosa and secondarily infected atopic dermatitis // Acta Derm Venereol. 2010; 90(1), p. 52–57.
- Fernandes P., Pereira D. Efforts to support the development of fusidic acid in the United States // Clin Infect Dis. 2011, 52, suppl. 7, s. 542–546.
- Rortveit S., Skutlaberg DH, Langeland N., Rortveit G. Impetigo in a population over 8.5 years: incidence, fusidic acid resistance and molecular characteristics // J Antimicrob Chemother. 2011, vol. 66(6), p. 1360–1364.
I. V. Khamaganova, Doctor of Medical Sciences, Professor
GBOU VPO RNIMU im. N. I. Pirogova Ministry of Health and Social Development of Russia, Moscow
Contact information about the author for correspondence
Factors influencing the effectiveness of treatment
The effectiveness of treatment is influenced by many factors.
- Patient age
. Elderly people have weakened immunity and quite a few chronic diseases, which significantly complicates treatment.
- Form and severity of the disease.
The later the patient consults a doctor, the longer and more serious the treatment.
- Contraindications
. Be sure to inform your doctor about existing pathologies and confirmed allergens, and also study the instructions for the prescribed medications. An allergic reaction to one of the components can only worsen the condition.
- Maintaining hygiene rules.
A daily change of underwear and bed linen is recommended every 2-3 days with washing of the latter at a temperature of 90C and mandatory ironing.
- Linen and clothing are made only from natural fabrics.
They absorb moisture well and do not promote sweating.
- Diet.
Flour products, sweets, spicy and fatty foods contribute to the proliferation of streptococcus. Eliminate everything that can cause an allergy - its exacerbation will aggravate an already unpleasant condition.
- No stress.
The infection takes a lot of energy. Try to lie down, move less (this is only for 10 days), do not conflict and do not react to provocations - you will cope with everything after recovery.
If you have streptoderma, you will have to follow not only the rules of personal hygiene, but also public hygiene. To avoid the spread of infection, exclude any contact (take sick leave), try to isolate yourself in a separate room at home, use only personal utensils and a towel. Streptococcus is transmitted very quickly and takes root well in a new carrier.
Prevention of streptoderma
Prevention of streptodemia in children and adults is based on compliance with the following four points.
- Hygiene comes first.
Regularly washing your hands with soap and washing your face is taught from the cradle, but, unfortunately, not everyone makes this rule a habit. Resorcinol, sulfur, and tar soap are recommended for hands and face. Showers should be regular, a sauna or bath at least once a week, or more often. It is necessary to wash your hands before and after eating, using the toilet, contacting pets, and returning from the street. Under no circumstances should there be dirt under the nails - it is often hidden by a spectacular manicure.
- Healthy lifestyle
If you cannot play sports or exercise, spend as much time as possible in the fresh air and ventilate the room more often. Hardening is very effective in strengthening the immune system, but you need to get used to it gradually.
- Complete nutrition.
It should be sufficient, but not excessive in calories, regular and frequent (at least 3 times a day). Include more vegetables, legumes, fruits, meat, fish, and dairy products in your diet.
- Treatment of damaged skin.
At the slightest cut, abrasion, or abrasion, treat it as quickly as possible with an antiseptic: chlorhexidine, brilliant green, or better yet, Rivanol 0.1%. The latter does not pinch, does not burn and restores the skin well, just be careful - it leaves yellow marks.
- Control of chronic diseases.
Do not delay visiting a doctor if there is another exacerbation of an ulcer, cholecystitis, pancreatitis, diabetes, etc. Advanced varicose veins also greatly reduce the immune system and lead to a decrease in the protective barrier of the skin.
Do you have translucent, itchy yellowish blisters or sticky spots around your mouth? No amount of baby oil, powder, or brilliant green can do this. Streptoderma requires a serious professional approach to treatment. Using only traditional methods can only lead to complications. Treat the first sores with an antiseptic, for example, Rivanol (it should definitely be in your home medicine cabinet), and immediately see a doctor.