ARACHNOIDITIS
(
arachnoiditis
; Greek arachne spider, web + eidos species + -itis; synonym:
arachnomingitis, leptomeningitis externa, chronic fibrosing leptomeningitis, limited adhesive meningopathy
) is a special type of serous meningitis, in which the inflammatory process primarily affects the arachnoid (arachnoid) membrane of the brain or spinal cord brain (arachnoidea) and to a much lesser extent soft. The term “arachnoiditis” was first used by A. T. Tarasenkov (1845). A detailed description of cerebral arachnoiditis was given by Beninghaus (Böninghaus, 1897), calling it “external serous meningitis” (meningitis serosa externa).
Etiology
The most common are infectious and infectious-toxic arachnoiditis associated with influenza, tonsillitis, typhoid, pneumonia, tuberculosis, sepsis, toxoplasmosis, rheumatism, brucellosis, syphilis, mumps, and infectious diseases of the ENT organs. Arachnoiditis often develops after injuries to the skull and spine (including closed ones). Less commonly, arachnoiditis is associated with endocrine and metabolic disorders. It is not always possible to accurately determine the etiology of arachnoiditis.
Many diseases of the central nervous system and spine can be complicated by arachnoiditis, especially often tumors, encephalitis, syringomyelia, epilepsy, osteomyelitis of the skull bones, spondylitis, etc., and reactive arachnoiditis sometimes develops far from the primary pathological focus in the brain.
General information
Arachnoiditis is an infectious disease of the central nervous system and is a serous inflammation of the structures of the arachnoid membrane of the brain or spinal cord. The arachnoid membranes do not have their own vascular system, therefore the lesions are not isolated, and infectious processes spread from the dura or soft meninges, therefore the symptoms of arachnoiditis are conclusively attributed to the serous type of meningitis .
The pathology was described in most detail by the German doctor Benninghaus, and the term was first used in the dissertation of A.T. Tarasenkov, who studied the signs of cerebral inflammation and arachnoiditis in particular. Some scientists call this disease serous meningitis, but according to ICD-10 it is assigned the code G00 and the name bacterial arachnoiditis , G03 - which includes meningitis due to other or unspecified causes, including arachnoiditis , meningitis , leptomeningitis , pachymeningitis , as well as G03 .9 – for unspecified meningitis – spinal arachnoiditis NOS (no additional instructions).
The brain has three membranes: hard, arachnoid and soft. Thanks to the hard one, sinuses are formed for the outflow of venous blood, the soft one provides trophism, and the arachnoid one is necessary for the circulation of cerebrospinal fluid . It is located above the gyri, but does not penetrate the sulci of the brain and separates the subarachnoid and subdural space. Its structure contains arachnoidendothelial cells, as well as bundles of collagen fibrils of varying thickness and quantity.
Histology of the meninges
Pathological anatomy and pathogenesis
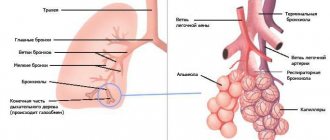
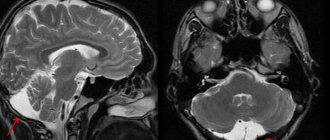
Rice.
1. Arachnoid cysts of the spinal cord (in the left picture - at the top, in the right picture - in the center). The arachnoid membrane with arachnoiditis becomes thickened, dense and acquires a grayish-white color. Adhesions form between it and the soft shell. The same adhesions often occur between the arachnoid and dura mater. The adhesive process leads to the formation of arachnoid cysts (Fig. 1), containing cerebrospinal fluid. If the cyst exists for a long time, its walls gradually become thicker and denser, and it turns into a tumor-like formation. The cyst fluid may become xanthochromic and contain large amounts of protein. The dura mater in the area of the pathological process is tense, swollen, thickened, rich in blood vessels, and loses its luster. Arachnoiditis often leads to occlusion of the cerebrospinal fluid pathways and secondary cerebral hydrops. Spinal arachnoiditis can cause blockage of the subarachnoid space of the spinal canal.
Rice. 2. Rough thickening of the arachnoid membrane with the formation of fibrous cords of various sizes. Rice. 3. Diffuse cellular infiltration of the arachnoid membrane.
Microscopic examination of the arachnoid membrane reveals fibrosis (Fig. 2) of varying degrees (thickening, coarsening of argyrophilic fibers, collagenization), hyperplasia of the endothelium of the membrane, infiltration of it with lymphoid elements (Fig. 3), proliferation of fibroblasts; vessels from the dura and choroid grow into the arachnoid membrane. In the soft shell there is hyperemia, new formation of blood vessels, inflammatory infiltration, and subsequently fibrosis. In adjacent areas of the brain, secondary changes are found caused by the pressure of meningeal cysts and adhesions, disorders of liquor and blood circulation, as well as the direct transition of the inflammatory process to the substance of the brain. Often severe arachnoiditis is complicated by periventriculitis and ependymitis.
Arachnoiditis in some cases occurs under the influence of exposure to the membranes of the pathogen itself, in others - its toxins. In case of injuries, the main role is played by disorders of blood and liquor circulation in the membranes and subarachnoid space. Dynamic disorders of blood and liquor circulation, swelling of adjacent areas of brain tissue and membranes explain the remissions and deteriorations that characterize the clinical picture of arachnoiditis.
Pathomorphological changes - from mild fibrosis of the arachnoid membrane to the formation of large cysts, numerous rough moorings in which all membranes are involved, and necrosis in the substance of the brain - make clear the varying severity of individual cases and the extremely unequal availability of their therapy.
Clinical picture, prognosis
Arachnoiditis is divided into adhesive (hyperplastic), cystic and adhesive-cystic, limited and diffuse, single-focal and multifocal. There are cerebral arachnoiditis (arachnoiditis cerebralis) and spinal arachnoiditis (arachnoiditis spinalis).
Arachnoiditis can occur with damage to the membranes of the convexital (convex) or basal surfaces of the brain.
The localization of the inflammatory process is the main factor that determines the characteristics of the symptomatology and course of individual forms of arachnoiditis.
According to the course, arachnoiditis is divided into acute, subacute and chronic, and according to pathogenesis - into primary and secondary.
Cerebral arachnoiditis
Cerebral arachnoiditis is characterized by general cerebral and focal symptoms.
General cerebral symptoms of cerebral arachnoiditis: headache, vomiting, dizziness, fundus changes, epileptic seizures, changes in cerebrospinal fluid. Headache is the most common and usually early symptom of cerebral arachnoiditis. In most cases, it is in the nature of a constant headache, aggravated by paroxysms, intensified by physical stress, mental work, anxiety, cold, overheating, random infections and other factors. The intensity of a headache is sometimes influenced by the position of the head. Vomiting usually occurs at the height of a headache attack. Dizziness ranks third in frequency. Changes in the fundus of the eye are found in most patients. Most often they find a more or less pronounced congestive optic nerve papilla, much less often neuritis, and even less often simple atrophy. General epileptic seizures are observed infrequently. Meningeal symptoms are mild or absent altogether.
Focal neurological symptoms vary depending on the location of the process.
Damage to the cranial nerves is a common occurrence in cerebral arachnoiditis of various locations, but they suffer more often and more severely in basilar arachnoiditis. Usually several nerves are affected at the same time.
During puncture, cerebrospinal fluid flows out mostly under increased pressure, it is colorless, the amount of protein in it is normal or reduced, rarely increased, cytosis is usually not increased. Pleocytosis in the range of 3-10 is found in approximately 1/3 of all patients, above 10 - in a few patients.
Many patients experience significant changes in the autonomic nervous system. “Neurotic” complaints are frequent.
Arachnoiditis of the brain begins acutely and subacutely soon after an infection, injury, severe hypothermia or exposure to other hazards that can cause arachnoiditis. But it can begin completely unnoticed by the patient, at various times after exposure to the etiological factor. The severity of the disease is extremely variable. Acute arachnoiditis may end in recovery. Acute arachnoiditis often occurs with low-grade fever. Blood morphology and ROE mostly do not change. Often acute arachnoiditis takes a chronic course. In chronic arachnoiditis, the temperature is usually normal. A typical course of arachnoiditis is with remissions and exacerbations. Severe forms of cerebral cystic adhesive arachnoiditis give the picture of a brain tumor and can be fatal, especially when the process is localized in the posterior cranial fossa.
Adhesive cerebral arachnoiditis can occur without occlusion of the cerebrospinal fluid pathways. The most diverse in its clinical manifestations and especially difficult to diagnose. Persistent headaches that worsen in attacks are often accompanied by vomiting or nausea. Dizziness, decreased performance. History of infection or head injury. Chronic relapsing course. Scattered neurological symptoms. There are no changes in the fundus or only slight blurring of the optic nerve papillae. Craniography often reveals symptoms of cerebral hypertension without destructive changes in the bones of the skull. Cerebrospinal fluid pressure is slightly increased, its protein content is unchanged or slightly increased, slight pleocytosis. A lumbar puncture often brings relief.
Convexital arachnoiditis of the central sulcus (Rolandic) area. Epileptic Jacksonian seizures of a motor or sensory nature, hemiparesis of varying severity, migraine-like headaches. There are usually no symptoms of cerebral hypertension. With extensive diffuse arachnoiditis of the convex surface of the hemispheres, cerebral dropsy may develop, and then symptoms of increased intracranial pressure appear, which are unusual for convexital A. Electroencephalography shows diffuse changes in the biocurrents of the brain.
Basilar arachnoiditis includes optochiasmal arachnoiditis, arachnoiditis of the posterior cranial fossa, and arachnoiditis of the cerebellopontine angle.
With optochiasmal arachnoiditis, the process threatens the patient with blindness. Visual acuity in one or both eyes decreases. Hemianopsia is observed, often bitemporal; atrophy of the optic nerve, less often congestion in the fundus, anosmia. In some cases, the motor nerves of the eyes are affected. Headaches are most often localized in the forehead, bridge of the nose, and orbits.
Arachnoiditis of the posterior cranial fossa is a relatively common and very severe form of cerebral arachnoiditis. The clinical picture resembles a cerebellar tumor, but the symptoms here grow much faster. General cerebral phenomena sharply prevail over focal ones. Often the VI, VII, VIII pairs of cranial nerves are significantly affected. Congestion in the fundus. The inflammatory process often causes fusion of the median opening of the IV ventricle (Magendie) and the lateral opening of the IV ventricle (Lushka), occlusion of the cerebrospinal fluid ducts, internal cerebral hydrocele with dilatation of all ventricles and the cerebral (Sylvian) aqueduct. Pain sensations are localized in the occipital region, radiating to the neck and upper back. Headaches worsen in attacks and are often accompanied by vomiting.
Cerebellopontine angle arachnoiditis usually manifests first with damage to the VIII nerve, peripheral facial palsy, or trigeminal neuralgia (neuritis). Symptoms of suffering from all three of these nerves may occur simultaneously. Later, cerebellar symptoms and bilateral pyramidal signs, mostly mildly expressed, appear. Arachnoiditis of the cerebellopontine angle is often associated with an infectious process in the ear.
Spinal arachnoiditis
Just like cerebral, spinal arachnoiditis can be adhesive, cystic, adhesive-cystic, diffuse or limited, single-focal or disseminated.
With diffuse spinal arachnoiditis, the clinical picture is very polymorphic and consists of radicular and conduction symptoms associated with damage to the spinal cord, its membranes and roots at various levels. The disease is mostly progressive: motor, sensory and pelvic disorders gradually increase. The cerebrospinal fluid is changed according to the type of protein-cell dissociation, but the protein content is not sharply increased. More or less significant remissions may be observed under the influence of treatment or spontaneous, affecting all manifestations of the disease or only some.
Limited adhesive arachnoiditis can exist for many years without causing any clinical symptoms, but it often produces radicular phenomena, causing the clinical picture of persistent radiculitis (sciatica, intercostal neuralgia, cauditis, etc.). Radicular-spinal arachnoiditis is often observed, in the clinical picture of which there is a combination of radicular phenomena and compression of the brain substance.
Cystic spinal arachnoiditis clinically resembles a spinal cord tumor. Intense radicular pain and paresthesia, appearing on one side of the body, quickly move to the other side. They are followed by conduction disorders of movement and sensitivity, disruption of the pelvic organs. Spinal compression syndrome gradually develops, which owes its origin to pseudotumor.
Arachnoiditis in children accounts for about 3-4% of diseases of the nervous system. Arachnoiditis develops as a complication of influenza, pneumonia, childhood infections, and in many cases with inflammatory diseases of the paranasal sinuses and otitis media. There is also primary viral arachnoiditis. Sometimes traumatic arachnoiditis occurs. Neurological symptoms are determined by the predominant localization of the inflammatory process. In children with convexital arachnoiditis, focal seizures often occur (more often than in adults), which can become generalized; in some cases, paresis of the facial nerve of the central type, asymmetry of tendon reflexes, and hypoesthesia are detected.
Basilar arachnoiditis is common, occurring with damage to the cranial nerves, signs of intracranial hypertension, impaired coordination, and in some patients with endocrine disorders.
Spinal arachnoiditis is rare in children.
Symptoms of arachnoiditis
Before talking about the symptoms that are characteristic of arachnoiditis, it should be noted that the signs of the disease depend on the location and are divided into three types - cerebral, spinal and cerebrospinal.
Cerebral arachnoiditis is primarily characterized by severe inflammation in the lining of the human brain, as well as the following symptoms:
- urinating too much;
- Convulsions, and in some cases severe seizures;
- Hearing disorders;
- Increased body temperature;
- Sleep problems;
- Memory and attention decrease;
- Partial or complete loss of the sense of smell;
- General weakness of the body, as well as excessive fatigue during physical or mental stress;
- Acrocyanosis (skin acquires some unusual blue tint);
- Constant dizziness, which is accompanied by excruciating pain in the head.
In situations where spinal arachnoiditis is present, almost the same symptoms are observed, but there are others, for example, a person is bothered by frequent pain in the lumbar region, as well as near the spinal region.
In addition, the patient is bothered by tingling in the extremities of the body, temporary paralysis, and sometimes numbness of the legs. In the most severe cases, a person feels disturbances in the genital organs, in particular, the level of potency decreases. The cerebrospinal type of the disease combines symptoms that are characteristic of both spinal and cerebral arachnoiditis.
Diagnosis
In the diagnosis of cerebral arachnoiditis, neurological symptoms, the development and course of the disease, the state of the cerebrospinal fluid, its pressure, pneumoencephalography data (especially defects in filling the subarachnoid space with air) are of primary importance.
The general diagnosis of cerebral arachnoiditis should be supplemented by an indication of the nature of the process, its localization and etiology (if known), the presence or absence of occlusion of the cerebrospinal fluid pathways. Diagnosis of cerebral arachnoiditis requires a comprehensive and detailed examination of the patient, which must necessarily include examination of vision, fundus, hearing, blood pressure dynamics, craniography (see). In all unclear cases, patients are subject to dispensary observation or inpatient examination. Many patients are cured, and then the diagnosis of arachnoiditis is removed. In some cases, we have to talk about residual effects after suffering cerebral arachnoiditis.
Differential diagnosis of cerebral arachnoiditis
have to be carried out: with a brain tumor, multiple sclerosis, cerebral atherosclerosis, chronic diseases of the ENT organs, cervical osteochondrosis, migraine, neurasthenia, post-infectious or post-traumatic asthenia. Particularly important is the differential diagnosis with a brain tumor, since the latter requires the earliest possible recognition. In some cases, cerebral arachnoiditis may accompany a tumor.
Differential diagnosis of spinal arachnoiditis
with a tumor is very difficult, in many cases it is impossible before surgery. There are a number of points to consider that can to some extent clarify the true nature of suffering. Disorders of the pelvic organs are usually less intense than with a tumor. Radicular phenomena are more scattered; many roots may be interested, and these are not always roots located adjacent to each other. Nonne-Fruen compression syndrome (xanthochromia, protein-cell dissociation, high cerebrospinal fluid pressure at the beginning of lumbar puncture) is not so clearly expressed. Queckenstedt's test (see Cerebrospinal fluid) does not increase fluid flow. Pleocytosis can be detected in the cerebrospinal fluid, the degree of which varies during lumbar punctures performed during different periods of the disease.
X-ray diagnosis of arachnoiditis
X-ray detection of arachnoiditis is possible in cases where, due to the inflammatory process, adhesions appear between the arachnoid and choroid (adhesive arachnoiditis), disrupting the circulation of cerebrospinal fluid, and local expansion of the arachnoid space (cystic arachnoiditis). To recognize and differentiate arachnoiditis from a tumor process, a comprehensive examination of the patient and comparison of the results of clinical, neurological and radiological studies are necessary.
Cerebral arachnoiditis can be diagnosed with a contrast study of the brain - pneumoencephalography (see Encephalography).
As a rule, there are no changes in craniograms. In case of arachnoiditis of the convex surface of the brain, in accordance with the localization and prevalence of adhesions of the arachnoid membrane, pneumoencephalograms reveal the absence of air in the subarachnoid fissures or uneven filling of dilated and deformed subarachnoid spaces with air. With arachnoiditis of the base of the brain, depending on the location of the adhesions on pneumoencephalograms, there may be no air in the base cisterns or, on the contrary, the cisterns may be overfilled with air and deformed. Arachnoiditis of the posterior cranial fossa, along with obliteration of the subarachnoid cisterns, sometimes causes occlusive hydrocephalus, which is determined on pneumoencephalograms by enlargement of the cavities of the ventricles of the brain.
Spinal arachnoiditis cannot be recognized from radiographs of the spine. To identify it, a contrast study of the spinal cord is performed (see Myelography). With adhesive arachnoiditis, the contrast agent is retained in areas corresponding to the level of the lesion. On myelograms this is displayed in the form of accumulations of contrast material in the form of drops, streaks, spots with clear and often sinuous outlines. In cases where adhesions cause a complete block to the passage of the contrast agent, it is very difficult to distinguish spinal arachnoiditis from a tumor using myelograms.
Contrast X-ray studies of the brain and spinal cord are important when choosing a method of surgical treatment of arachnoiditis and for assessing the results of the operation.
Treatment
Treatment of cerebral arachnoiditis can be conservative or surgical. Diffuse hyperplastic arachnoiditis without occlusion of the cerebrospinal fluid ducts, without significant hypertensive phenomena and epileptic seizures should be treated conservatively, and cystic or adhesive-cystic arachnoiditis with a clinical picture of a brain tumor should be subjected to surgical treatment. Therapy for cerebral arachnoiditis should be individualized, comprehensive, planned and systematic. The pathomorphological essence of the process is such that one cannot count on easy success. Conservative therapy includes disinfectants, anti-inflammatory, absorbent, and dehydrating agents. In case of arachnoiditis associated with an infectious focus in the ENT organs or bones of the skull, simultaneous treatment (conservative or surgical) of this disease is necessary. Cerebral arachnoiditis without occlusion of the cerebrospinal fluid pathways and severe focal symptoms often respond well to therapy.
Heat is also applied to the head (if the patient tolerates it well), iodine galvanization according to Bourguignon, collar massage, mustard plasters to the calves, to the back of the head, and collar area. For severe headaches - analgesics. Drugs cannot be prescribed. In many cases of arachnoiditis, subarachnoid air administration is helpful. Deep radiotherapy reduces pain, weakens the inflammatory process and reduces the secretion of cerebrospinal fluid. Surgery often gives good results. Drug treatment must also be carried out after surgery.
Treatment of spinal cystic arachnoiditis with conservative methods is usually ineffective, but surgical intervention gives good results. Adhesive arachnoiditis is subject to conservative treatment (medications, as in cerebral arachnoiditis, physiotherapy, mud resorts, subarachnoid air injections; in many cases, deep radiotherapy brings good results).
Surgical treatment of arachnoiditis
The main purpose of operations for arachnoiditis is to remove or disconnect membrane adhesions, scars, cysts that put pressure on the brain tissue or cause disturbances in the circulation of cerebrospinal fluid.
Indications for surgery
Indications for surgery for arachnoiditis of the convexital surface of the cerebral hemispheres are frequent focal epileptic seizures that are not eliminated by drug therapy, especially in cystic forms of arachnoiditis. Typically, the high prevalence of damage to the membranes and brain tissue in arachnoiditis requires establishing the exact localization of the lesion.
The indication for surgery for arachnoiditis of the posterior cranial fossa is the presence of occlusion of the cerebrospinal fluid ducts with increasing hypertensive-hydrocephalic phenomena and focal symptoms of damage to the cerebellopontine angle, cerebellum, and brain stem.
In optochiasmal arachnoiditis, the main indication for surgery is a progressive decline in visual acuity or narrowing of visual fields.
Surgeries for spinal arachnoiditis are indicated in the presence of spinal cord compression, as well as in increasing motor, sensory disturbances and radicular pain associated with a limited adhesive process or the formation of cysts.
Surgical interventions for arachnoiditis are indicated when conservative therapy is ineffective in the chronic or residual stage of the inflammatory process.
Prognosis for arachnoiditis
In most cases, patients with arachnoiditis receive the third disability group. However, if they have severe visual impairment and frequent epileptic seizures, they may be assigned a second disability group.
The first disability group includes patients with opticochiasmatic arachnoiditis, which caused complete blindness. Work in transport, at heights, near fire, in noisy rooms, in unfavorable climatic conditions, and with toxic substances is contraindicated for patients with arachnoiditis.