Loss of smell
A person smells through receptors. Molecules of substances carrying aroma enter the receptors, these waves are transmitted along the nerve endings to the brain, where this impulse is processed. Most often, loss of smell occurs in men, much less often in women. With age, the risk increases, and you need to be more careful about your body.
There are different types of loss of smell:
- Hyposmia is an extremely poor perception of smells. Also, with hyposmia, there is an incomplete loss of smell, i.e. only for certain smells.
- Hyperosmia is, on the contrary, excessive sensitivity to odors.
- Cacosmia - perception in this case is turned upside down. Attractive smells seem disgusting.
- Anosmia is the complete loss of olfactory processes. It is formed due to colds, and in some cases even after a stroke.
Loss of smell can occur from birth, due to the fact that the respiratory organs have not had time to form properly. You can also acquire anosmia during your life.
Causes of loss of smell
During the loss of smell, the receptors will not respond to stimuli. The brain does not receive signals and does not distinguish smells. If the problem is in the central nervous system, then the receptors, on the contrary, send impulses to the brain, but the brain does not perceive them. And sometimes it may be that the receptors in the nose recognize and send odors to the brain, but along the way they are blocked.
ARVI and COVID-19
Loss of smell can be a consequence of a common cold, flu or acute respiratory viral infection. In this case, swelling of the mucous membrane occurs, which disrupts not only the breathing process, but also deprives the receptors of their functions - transmitting impulses to the brain.
Not long ago, doctors found out that loss of smell is, in most cases, also a symptom of coronavirus. It appears in 80% of cases on about 3–5 days. Moreover, during this period the person may not experience any other symptoms. It is known that the nasal mucosa is the first to encounter viruses and bacteria, and the immune system begins to work from the nose to destroy as many viral agents as possible. Perhaps damage to the receptors and cells of the mucous membrane occurs precisely because of the “smart” attack of the virus in order to break the defense at the attack stage and easily penetrate the body.
Another opinion is that the sense of smell disappears due to the body’s protective reaction to the virus; the receptors sacrifice themselves to prevent the infection from spreading. The sense of smell returns approximately 2 weeks after complete healing. But there are rare cases when the return is delayed and the sense of smell is fully restored within several months.
According to statistics, in most cases this symptom indicates that the disease will not develop into a particularly acute form with serious consequences. Most often, anosmia develops immediately after the incubation period, 3-4 days after the viral agents have entered the body, but before the appearance of other symptoms - sore throat, cough, fever, rash and chest congestion, weakness and fever.
According to another version, with covid, olfactory receptors are damaged at the level of the nervous system, when the transmission of impulses from the receptors to the brain and back is blocked by viral agents. But why this happens and how the virus acts in the body of a particular person is an area that has not been sufficiently studied.
That is why sleeping pills and sedatives are often prescribed in doctors’ protocols. To support the nervous system that is being attacked.
Also, we can assume that in mild, moderate and severe forms of the disease without critical complications, the return of the sense of smell with proper treatment of coronavirus indicates that the virus is receding, even if other symptoms are partially preserved.
Parkinson's disease, Alzheimer's disease
Loss of smell in such diseases is the most striking symptom. Sometimes it can become the very first and earliest sign of impending irreversible disorders in the brain. Thus, scientists can determine the risk of disease for a person by how he is able to recognize, remember and remember smells.
In this case, we have to say that the loss of smell is exclusively neurological in nature. Atrophic changes in the cerebral cortex, characteristic of these diseases, affect the central part of the olfactory analyzer. According to MRI, degeneration processes affect the primary olfactory cortex, hippocampus, thalamus and hypothalamus. Which inevitably leads not only to disturbances in coordination activity, but also to memory loss and impaired sense of smell.
Other causes of loss of smell
- Allergy. If a person is susceptible to allergic reactions to the smells of flowers or something else, his nasal cavity may become inflamed.
- Injuries. If the nose or brain is injured, the sense of smell may disappear immediately.
- Age. The older a person gets, the processes in his body slow down. This happens with the membranes of the nose. Older people are more likely to experience dryness and atrophy of the nasal mucosa.
- Tumor. If a benign tumor is found, it is removed and the sense of smell gradually returns.
- Polyps. New growths in the nose can interfere with olfactory processes.
- Smoking. Nicotine destroys the nerve endings in the nose, this happens gradually, but can lead to a complete loss of smell.
- Neurosis. Loss of smell can be caused by long-term emotional problems or a lot of stress.
- Burns. Toxic vapors, when inhaled, can burn the nasal mucosa or lubrication with alcohol-containing liquids.
- Incorrect structure of the nasal cavity.
- Lack of vitamins (vitamin A) or other substances in the body.
Consequences of loss of smell
Problems in the perception of smells are a big problem that has a great impact on the entire body. Bright and juicy aromas of food trigger the digestive system and stimulate the secretion of gastric juice. If a person cannot smell the food he eats, the gastrointestinal tract will also suffer.
If viruses or harmful substances enter the body through the nose, a defensive reaction is provoked, for example, sneezing. If the receptors do not awaken a defensive reaction when the sense of smell is lost, then harmful substances will continue to freely penetrate deep into the body, causing even more damage.
Olfactory impairment and quality of life
Of course, the loss of function of any of the senses is a significant problem, in some situations equated to disability. To assess the degree of smell impairment and the impact of this problem on the quality of life, special questionnaires were developed. Some patients have been found to become more irritable, have increased levels of anxiety, may have decreased appetite, develop social withdrawal, and are at risk of losing their sense of dangerous odors, such as gas leaks. All this, of course, creates the need to solve these problems.
Restoring the sense of smell
If you have a long-term loss of smell, you should immediately go to the clinic for an appointment with an otolaryngologist. If you treat yourself, you can worsen the current condition.
Recovery can be:
- Surgical.
Such intervention may be required in advanced cases (for example, with a tumor or deviated septum). Then the surgeon performs the operation.
- Medicinal.
The doctor prescribes a list of necessary medications, from nasal rinses to antibiotics, antiviral and antifungal agents.
- Physiotherapeutic.
Treatment may require physical therapy. The doctor prescribes heating or inhalation, and in some cases laser treatment is performed.
- People's
No one has abolished traditional medicine, but in no case should you prescribe decoctions for yourself. The doctor may prescribe a decoction for rinsing the nose from chamomile and oak bark or nasal drops based on aloe juice.
- Complex.
Those. This is the application of all types from physical therapy to surgical.
Methods for treating smell disorders
- rinsing the nose with saline solutions;
- use of hormonal-based sprays to relieve inflammation and swelling (strictly as prescribed by a doctor);
- olfactory training with essential oils.
It should be noted that scientists have not been able to establish a relationship between the use of these products and the restoration of the sense of smell, that is, the effectiveness of these treatment methods for impaired smell in COVID-19 has not been proven. Olfactory training with essential oils can be recommended for those whose sense of smell has been partially restored, but not in cases where the perception of smells has been distorted or other disturbances have occurred. The evidence base for the effectiveness of olfactory training for smell disorders after Covid-19 is weak.
Diagnostic measures
When contacting a doctor, attention is paid to complaints and epidemiological history. If the patient has been in contact with a sick person, and also has nasal congestion and a high temperature, ARVI and acute respiratory infections can be assumed. A person is recommended to undergo a general blood test to accurately determine the nature of the disease: bacterial or viral.
A sudden loss of smell and taste is a sign of coronavirus infection. The patient is advised to undergo tests for the pathogen in the form of a nasal swab.
Allergic rhinitis is diagnosed by a characteristic clinical picture. A smear from the nasopharynx reveals neutrophils and elevated IgE in the blood.
Atrophic rhinitis is diagnosed by an otolaryngologist after an in-person examination. Sometimes an x-ray is recommended. The same diagnostic method is used for sinusitis.
Forecast
The prognosis for the patient depends on what is causing the pathology. If the systems are not irreversibly damaged, but there is simply an obstruction of the nasal passages, due to which aromas do not reach the olfactory center, the prognosis is generally favorable, since in 95% of cases the sense of smell is completely restored after therapy. In case of damage to the olfactory nerve, central nervous system or age-related changes, due to the fact that it is impossible to restore a normal state, the prognosis for the patient will often be poor.
Unilateral anosmia, bilateral – symptoms
Impaired sense of smell can be combined with the following symptoms:
- memory problems;
- double vision;
- difficulty swallowing;
- speech problems;
- runny nose;
- cough;
- general weakness, etc.
A different combination of symptoms helps the doctor differentiate peripheral (impairments at the level of olfactory receptors and nerve fibers) anosmia from central (associated with brain damage at the level of the olfactory center).
In order to distinguish unilateral from bilateral loss of smell, the doctor performs a special test. The otolaryngologist alternately brings substances with a strong odor (vanilla, coffee, etc.) to one or the other nostril. A special olfactory test kit may also be used.
Treatment of anosmia
When deciding how to treat anosmia, each individual case is considered.
If it is anosmia due to a runny nose or allergies, no special treatment is usually required and the problem will go away on its own. Short-term use of vasoconstrictors will help open the nasal passages and make breathing easier.
If a tumor is found in the nasal cavity, surgery may be required to remove it.
If you smoke, you should stop smoking.
Unfortunately, anosmia is not always treatable, especially if the cause is age.
General measures for the treatment of anosmia include: physiotherapeutic procedures, breathing “gymnastics” (special training and exercises), and drug therapy.
Features and treatment of anosmia with coronavirus
Anosmia is a major neurological symptom and one of the earliest and most frequently reported indicators of COVID-19. Statistics show that it detects the disease more accurately than other known symptoms such as fever and cough.
Anosmia with Covid occurs due to a temporary loss of function of nerve cells in the olfactory epithelium. The duration of anosmia during coronavirus usually lasts several weeks, after which the sense of smell recovers on its own. This is much faster than the months it may take to recover from anosmia caused by other viral infections.
There is no one clear answer to the question of how to treat anosmia after coronavirus. As already mentioned, in the vast majority of cases, the perception of odors returns on its own. However, you can stimulate it with the measures listed above.
All this is available in our ENT clinic in Chertanovo. We have developed programs that include conservative therapy and physical therapy for the treatment of anosmia after Covid and not related to it.
Diagnosis of anosmia
At the appointment, the otorhinolaryngologist clarifies a detailed history of the disease. It is important to provide information as completely as possible to exclude factors such as head injury, smoking, medication, chronic diseases, etc. The doctor will also examine the nasal cavity using a special instrument called a video endoscope to see if a polyp or other growth is affecting the sense of smell.
Additional tests and examinations, such as computed tomography or magnetic resonance imaging, may be needed to determine the cause of anosmia.
How does our sense of smell work?
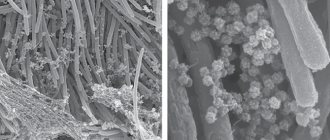
Deep in the nasal cavity, millions of sensory neurons are located in tissue called the olfactory epithelium. The tips of these cells contain proteins called receptors that bind odor molecules. Receptors are like locks, and passing odor molecules are like keys. Humans have about 450 different types of olfactory receptors. (For comparison, dogs have about twice as many.)
The complexity of receptors and their interactions with odor molecules is what allows us to detect a wide variety of odors. And what we think of as a single smell is actually a combination of many molecules acting on many receptors, creating a complex neural code that we can identify as the smell of a rose or freshly cut grass.
This neural code begins with the olfactory sensory receptors in the nose. Once an odor molecule binds to a receptor, it initiates an electrical signal that travels from sensory neurons to the olfactory bulb, a structure at the base of the forebrain that transmits the signal to other areas of the brain for further processing.
Symptoms of a sense of smell disorder occur when one of the links in this chain is affected. This may be a malfunction of the olfactory sensory receptors or the part of the brain responsible for smell.
Causes of anosmia
Nasal congestion due to a cold, allergies, sinus infection, or poor air quality are the most common causes of anosmia. Other provoking factors:
- Nasal polyps are small, benign growths in the sinuses that block the nasal passage.
- Trauma to the nose or head.
- Viral infections (this includes anosmia due to coronavirus).
- Exposure to toxic chemicals such as pesticides or solvents.
- Certain medications, including antibiotics, antidepressants, anti-inflammatory drugs, heart medications, and others.
- Drug use.
- Tobacco abuse. Smoking can dull your senses, including your sense of smell.
- Elderly age. Like vision and hearing, the sense of smell can weaken with age. In fact, the sense of smell is most acute before the age of 60, after which it begins to decline.
- Certain diseases such as Alzheimer's disease, Parkinson's disease, multiple sclerosis, congenital pathologies, hormonal disorders.
- Radiation therapy to the head and neck.
What diseases does it occur in?
Often, loss of smell accompanies the course of acute respiratory viral infections and acute respiratory infections. At the same time, the nasal mucosa swells, making it difficult for patients to breathe. If you remove the congestion, sensitivity will be restored. The same mechanism of loss of smell is characteristic of allergic rhinitis and sinusitis.
Much more people are concerned about why the nose breathes and odors are not felt. This happens when nerve fibers or receptors are damaged. The symptom occurs with chronic atrophic rhinitis, uncontrolled use of vasoconstrictor drops for the common cold, taking ACE inhibitors or estrogens, as well as heavy metal poisoning. This is also observed with influenza and coronavirus infection.
Damage to the areas of the brain responsible for smell is quite rare. This happens with degenerative pathologies of the nervous system (Alzheimer’s disease, multiple sclerosis), head injuries, and also against the background of complications after brain surgery.