Article for the “bio/mol/text” competition: The impact of tobacco smoking on human health is a favorite topic of journalists. There are thousands of brochures, articles and books about how harmful smoking is and how to get rid of nicotine addiction. As a rule, their authors limit themselves to considering the psychological aspect or focus the reader’s attention exclusively on the severe medical consequences of smoking. And as a rule, no one describes the mechanism of development of nicotine addiction or the interaction of tobacco with the body at the molecular level. This article attempts to address this deficiency in the literature on smoking.
Note!
This work was published in the “best review article” category of the “bio/mol/text” competition 2015.
The sponsor of the nomination “Best article on the mechanisms of aging and longevity” is the Science for Life Extension Foundation. The audience award was sponsored by Helicon.
Competition sponsors: Biotechnology Research Laboratory 3D Bioprinting Solutions and Scientific Graphics, Animation and Modeling Studio Visual Science.
Tobacco yesterday and today
Everyone knows that the American Indians taught Europeans to use tobacco. Soon after Columbus's expeditions at the end of the 15th century, the Spaniards began cultivating tobacco. Tobacco owes its scientific name (lat. Nicotiana) to the French ambassador to Portugal Jacques Nicot, a famous popularizer of tobacco products in the second half of the 16th century. Niko's authority was so great that tobacco quickly began to be used not only for entertainment purposes, but also in medical practice. Thus, in 1571, the Spanish physician Nicolas Monardes wrote a book about medicinal plants, in which he stated that tobacco healed 36 diseases [2].
The fight against tobacco smoking began in the 17th century. The English king James I was one of the first to pursue an anti-tobacco policy. In his 1604 treatise, “A Counterblaste to Tobacco,” he called smoking “a custom that is disgusting to the sight, offensive to the smell, injurious to the brain, and dangerous to the lungs.” The treaty was followed by a 40-fold increase in the duty on tobacco. In the Ottoman Empire, smoking was banned in 1633 by decree of Sultan Murad IV and was punishable by death, but the ban was soon replaced by a tax. In pre-Petrine Russia, smokers were beaten and even exiled or executed. In many other European and Asian countries, barriers to the spread of tobacco have existed for quite a long time [3, 4].
In 1828, scientists from Heidelberg isolated nicotine in its pure form and concluded that it was a strong poison. Soon after, nicotine began to be used as an insecticide. Around the same time, cigarettes appeared, still inferior in popularity to cigars. Despite the global spread of tobacco, tobacco smoking has not yet been recognized as a global problem. Thus, by 1889, only 140 cases of lung cancer were documented worldwide. In the same year, the English physiologist John Newport Langley described the effect of nicotine on the conductivity of the nerve ganglia: nicotine blocked impulse transmission in the sympathetic nervous system [5].
At the beginning of the 20th century, cigarettes became the main tobacco product, and the largest tobacco companies in the world were based in the United States. In 1912, oncologist Isaac Adler first pointed out the connection between smoking and lung cancer. Lung cancer remained a rare disease until the First World War, after which smoking became a widespread habit due to the inclusion of cigarettes in army rations.
In the 1930s, the connection between smoking and lung cancer, as well as a reduction in life expectancy, was strictly proven. Nevertheless, the popularity of tobacco continued to grow at an unprecedented rate. It was only in the 1980s that nicotine addiction was recognized worldwide, followed by restrictions on the advertising and distribution of tobacco products. It was since the 1980s that health care structures around the world began to fight tobacco smoking, despite which, the tobacco industry is still thriving and increasing its turnover every year.
Risk of developing cancer due to smoking
The main harm of smoking (cigarettes, cigars and pipes) is their ability to cause cancer. This addiction can lead to malignant neoplasms 11:
- lungs;
- lips, tongue and other parts of the oral cavity;
- pharynx;
- larynx;
- esophagus;
- stomach;
- pancreas;
- liver;
- Bladder;
- kidney;
- cervix;
- colon.
In 30-35% of cases, nicotine is the main cause of the development of the above diseases11.
Tobacco smoke is the most common known carcinogen12 Smoking causes irreparable harm to the body : components of cigarette smoke are capable of forming mutagenic compounds with DNA, which lead to gene damage, the occurrence of mutations and the subsequent development of cancer12.
Tobacco consumption not only increases the risk of tumors , but also reduces life expectancy after cancer and increases the risk of relapse13.
Thus, quitting tobacco products helps prevent cancer: it helps prevent the emergence of new mutations , and also has a beneficial effect on the prognosis of existing cancers13.
Up to contents
The mechanism of development of nicotine addiction
Tobacco definitely would not have become so popular if it were not addictive. However, the mechanism of nicotine's effect on the nervous system has become known relatively recently. To understand this mechanism, it is necessary first of all to know how the transmission of nerve impulses occurs.
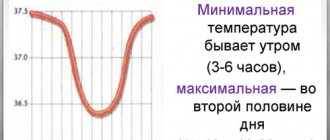
Neurons, as a result of the energy-dependent output of three Na+ ions from the cell in exchange for the input of two K+ ions, create an electrochemical gradient on their membrane [6]—the cell is polarized (a negative charge accumulates inside, and a positive charge accumulates outside). When the cell is stimulated, depolarization occurs: channels open in the cell membrane, equalizing Na+ concentrations on both sides. The opening of channels in one place triggers a chain depolarization throughout the cell. If the sodium channels remained open, the neuron would be constantly in a depolarized state. However, this does not happen because the sodium channels open only for a few milliseconds, followed by the opening of other channels that remove K+ from the cells, which promotes repolarization. The wave-like opening of sodium and potassium channels is called an action potential (AP).
Transmission of action potentials from one neuron to another differs from intracellular transmission. When the AP reaches the contact of two neurons, it is no longer Na+ that enters the excited cell, but many Ca2+ ions, which are a signal for the release of neurotransmitters into the intercellular gap* Neurotransmitters, by binding to ion channels (receptors) on the membrane of the receiving cell, trigger AP in it.
* - The story surrounding the transport and secretion of neurotransmitters in nerve fibers is exciting and beautiful. For its study, the Nobel Prize was awarded in 2013 [7], and already in 2015, an amazing comic book depicting these processes appeared on the “biomolecule”: “How the release of a neurotransmitter occurs” [8]. - Ed.
Nicotine is structurally similar to one of the most common neurotransmitters in the body—acetylcholine (Ach)—and imitates its action, which is why some cellular Ach receptors are called nicotinic [9].
Figure 1. Diagram of signal transmission in neurons. a - symbols on the diagram, b - the diagram itself. At rest, a neuron, with energy consumption, creates tension on its membrane. When exposed to an external stimulus, the neuron depolarizes, which leads to the release of neurotransmitters (green circles), which trigger depolarization in the next neuron. Depolarization is necessarily followed by repolarization, returning the cell to its original state.
When the body relies on externally supplied nicotine instead of AHC, addiction occurs. More precisely, the formation of nicotine addiction is caused by the substitution of ACh in the tegmentum, also known as the pleasure center. With natural concentration of ACh, excitation and suppression of the pleasure center are balanced.
But with regular use of nicotine, neurons adapt: there are fewer nicotinic receptors in synapses, leading to inhibition of the tegmentum (α4β2), when the number of receptors leading to its activation (α7) remains the same. It is also worth considering that nicotine is very stable and therefore leads to a much longer stimulation of the pleasure center than ACH, which decomposes in synapses in a matter of milliseconds.
Stimulation of the tegmentum is a key point in the formation of various types of addictions and behavior in general. But the pleasant sensations caused by nicotine are only one side of the coin. Don't forget about withdrawal syndrome, which is why most smokers who decide to quit relapse again and again.
Withdrawal syndrome consists of loss of concentration, anxiety, depression, insomnia and increased appetite when quitting nicotine. You can often hear that cigarettes help cope with stress, but stress and withdrawal symptoms are very similar from a physiological point of view, which casts doubt on the calming properties of nicotine. At the moment, it is not known exactly how the removal of nicotine from the body leads to withdrawal syndrome. However, it is clear that an important role in its occurrence is played by the center of discontent - the habenula, which suppresses the tegmentum when we do not get what we want. The functioning of this part of the brain is also highly dependent on nicotine receptors, and most likely, neuroadaptation also occurs there, leading to unpleasant sensations due to a lack of nicotine [10].
Figure 2. Formation of nicotine addiction. Normally, the neurotransmitter acetylcholine (Ach) maintains the balance of stimulation and inhibition of the pleasure center (tegmentum). Nicotine produces pleasant sensations by binding to α7 receptors and reducing the number of α4β2 receptors. When nicotine levels drop, another part of the brain, the habenula, suppresses the pleasure center. These two phenomena lead to the formation of nicotine addiction.
Lose weight on tobacco?
Smoking in general causes your metabolism to speed up. The body spends energy more actively and burns reserves. Therefore, yes, of course, you can lose weight with cigarettes. But is the result worth it? “Weight loss from tobacco is of the same nature as weight loss from cancer
or from improper functioning of the thyroid gland,” says Galina Sakharova, Doctor of Medical Sciences, Deputy Director of the Research Institute of Pulmonology of the Federal Medical and Biological Agency of Russia. “A smoker loses weight because the body is trying to cope with the negative consequences of smoking.”
Why quit smoking?
You have given up smoking. What will happen tomorrow, in two weeks and in a few months? Only good.
Physiological effects of nicotine
Nicotine can be consumed in many ways, but smoking cigarettes is the most common. During smoking, most of the nicotine is burned in the flame, but the small amount of nicotine inhaled is compensated by the gigantic surface of the lungs, through which it is absorbed into the blood. When chewing tobacco is used, nicotine concentrations in saliva are up to 6 orders of magnitude higher than the concentration in lung fluids after one cigarette.
Nicotine entering the body in one way or another stimulates nicotinic receptors not only in the brain, but also in all other tissues. In the lungs, nicotine stimulates the division of mucosal cells by activating the corresponding receptor. Excessive division, combined with DNA damage caused by tobacco carcinogens, can lead to lung carcinoma. Similar phenomena are observed in cells throughout the body, which is why nicotine consumption (even not through smoking) increases the risk of breast, uterine and food tract cancers.
The effect of tobacco smoke and nicotine on the immune system is extremely interesting and controversial. Depending on the frequency, length of smoking, and individual differences, tobacco smoke (TS) can either stimulate or suppress the immune system. For example, TD is rich in reactive oxygen species, which cause chronic inflammation of the lungs, that is, it generally stimulates the immune system. And although some studies have shown that TD activates immune T cells, this does not mean that tobacco is good for the immune system: medical statistics say that smokers suffer more often and more seriously from colds, pneumonia and tuberculosis than non-smokers [11]. In addition, in other studies, where more attention is paid specifically to antiviral immunity, it was shown that TD reduces the body’s resistance to viruses [12].
Smoking also affects the course of autoimmune diseases [13]. Smoking is known to aggravate rheumatoid arthritis, Crohn's disease (but alleviate ulcerative colitis!) [14] and contribute to the development of emphysema. Relatively recently, people began to understand the reasons for this: activated T cells begin to produce antibodies to the structural protein of the lungs, arteries and skin - elastin [15]. Such antibodies target the smoker’s immunity to his own body. The autoimmune aspect is one example of the irreversible impact of TD on health, since once formed, antibodies will continue to be synthesized even years after quitting smoking.
You can often hear that smoking leads to diseases of the cardiovascular system. In many ways, these diseases are triggered by the factors already mentioned: oxidative stress and inflammation.
Reactive oxygen species TD reduce the activity of the enzyme responsible for relaxing blood vessels and lowering blood pressure - NO synthase. This enzyme produces nitric oxide NO, which, when reacted with reactive oxygen species, becomes the toxic molecule peroxynitrite [16]. Thus, by reducing NO levels, smoking leads to hypertension, the main cause of ischemic diseases. Smoking causes impotence through the same mechanism: a lack of NO leads to vasoconstriction and reduced blood flow in all organs.
Another problem that only male smokers may experience is the loss of the male Y chromosome. Swedish scientists have discovered that the blood of smokers contains 3-4 more cells that have lost this purely male part of the genome. This phenomenon may be related to general genetic instability caused by tobacco smoke mutagens and is very likely to contribute to the development of cancer [17].
Chronic pneumonia in smokers activates leukocytes throughout the body, including in the blood. Against the background of this inflammation, the number of endothelial progenitor cells decreases, which ensure the restoration of damaged vessels [18], and blood clotting increases [19].
HOW TO QUIT SMOKING?
You can quit smoking at once, when a person quits smoking once and for all, and gradually, slowly, in stages.
The first method is suitable for people who have recently started smoking, and quitting smoking does not cause significant withdrawal symptoms (depression, loss of appetite, insomnia, nausea, etc.).
The second method is gradual withdrawal, in which the number of cigarettes smoked daily is reduced until the person completely quits smoking. Not every smoker manages to avoid withdrawal symptoms. During this period, the following come to the rescue: self-hypnosis, hypnosis, acupuncture, the use of medications (as prescribed by a doctor), as well as walks in the fresh air, physical exercise, and a balanced diet.
Where to begin?
- It is necessary to determine at what moments a strong desire to smoke arises and try to abstain from a cigarette. Try not smoking for a whole day or sharply reducing the number of cigarettes you smoke. If this works, you can confidently say: “I am able to quit smoking!”
- Change your surroundings, go on vacation and under no circumstances touch a cigarette.
- You need to prepare to quit smoking. To do this, set a specific date, mentally tune in to it and practice:
- Do not finish the cigarette until the very end, because the most harmful components of tobacco smoke are in the last third;
- Try not to drag on;
- Reduce the number of cigarettes you smoke daily;
- Don't smoke on an empty stomach;
- Never smoke in company.
Considering that the first days without nicotine are the most difficult and to make this stage go faster and easier, use some tips:
- Drink more fluids - water, juices, fruit drinks, weak tea with lemon.
- Avoid drinking strong tea and coffee, spicy and spicy foods, and alcoholic beverages, all of which exacerbate the craving for a cigarette.
- Eat more vegetables and fruits, dairy products.
- Do physical exercise, it not only distracts you from smoking, but also clears your breath, improves your mood, and increases your vitality.
- Try to change your usual routine: get rid of the routine, for example, choose a different route to work, change the time and place of breakfast and lunch.
- Relax! To reduce stress, take a hot bath, do gymnastics, read a book.
- Count how much money you saved by giving up cigarettes. Buy yourself a gift with this money.
Modern means of combating nicotine addiction
In developed countries, every year half of smokers try to quit their bad habit, but only 2% of them succeed. This low success rate is due to the fact that smokers usually decide to quit suddenly and try to do it without resorting to auxiliary means.
The most popular way to treat nicotine addiction is nicotine replacement therapy (NRT). It is based on the idea that taking nicotine in controlled and constantly decreasing doses will ultimately lead to recovery from addiction. The first NRT drug was nicotine chewing gum released in 1971 by the Swedish company Nicorette. Today, pharmacies sell dozens of drugs from different companies based on the “wedge by wedge” principle: nicotine patches, inhalers, lollipops, sprays and, of course, chewing gum. A number of studies have shown that NRT is twice as effective as placebo [20] and could help an additional three percent of smokers quit.
Much less known are other, sometimes much more effective, anti-smoking medications.
One such drug is cytisine, a broom alkaloid. This plant has been known in traditional medicine for centuries, and during World War II, people began to consider it as a substitute for tobacco. Cytisine appeared on the market even earlier than nicotine chewing gum - in 1964 it began to be produced in Bulgaria under the Tabex brand.
Cytisine, like nicotine, can bind to nicotinic receptors in the brain. But, firstly, it binds to them more tightly, that is, it does not allow nicotine to approach them, and secondly, it activates them weaker. Thus, cytisine interferes with the reinforcement of addiction, even if the person continues to consume nicotine. If a person has stopped smoking and experiences discomfort, then cytisine stimulates the pleasure center enough to eliminate withdrawal symptoms, but not enough to form a new addiction.
This drug is not widely used outside Central and Eastern Europe [21]. According to 2011 data, cytisine is 3.5 times more effective than nicotine replacement therapy drugs [22]. However, it is worth considering that in general less research has been carried out on cytisine than on other drugs, which actually hinders its spread throughout the world.
Varenicline, a drug from the largest pharmaceutical corporation Pfizer, produced since 2006, has a similar mechanism of action. Varenicline has undergone rigorous clinical trials and is sold worldwide. Its effectiveness during long-term therapy is slightly greater than that of NRT, while the drug itself is noticeably more expensive than nicotine gum and cytisine [23].
Another common treatment for nicotine addiction is bupropion. This drug has been produced since 1989 and is positioned primarily as an antidepressant. Its ability to make smoking cessation easier is only a side effect: bupropion binds to nicotinic receptors in the brain, but does not activate them. The effectiveness of this substance is comparable to nicotine replacement therapy [24].
Figure 3. Nicotine is chemically similar to acetylcholine (one of the substances that transmit nerve impulses between neurons) and imitates its action. Modern medications for nicotine addiction are structurally similar to nicotine, but have a different effect on the nicotinic receptors of neurons, easing withdrawal symptoms.
The action of all the described drugs is based on the binding of nicotinic receptors in the brain. In recent years, there has been active development of a fundamentally different approach to the treatment of nicotine addiction - nicotine vaccination.
As with conventional vaccination, this therapy produces antibodies in the patient's body. Antibodies bind nicotine, thereby preventing it from entering the brain and depriving it of physiological activity.
Vaccines of this kind can help not only against nicotine, but also against any other chemical addiction (except alcohol). The body typically does not produce antibodies against small molecules of psychoactive substances, so vaccines combine these molecules with larger proteins that trigger an immune response.
There have already been successful trials of nicotine, methamphetamine, cocaine and opiate vaccines. With vaccination, the side effects of treatment are much weaker, and the effect is more stable than with drug therapy. But there are also disadvantages: vaccination has no effect at all on a quarter of addicts. In addition, anti-nicotine vaccination can be frightening due to its duration: the course consists of 4-5 injections over three months [25].
Recently, the genetic approach to the study of nicotine addiction has become extremely popular. Thanks to massive research into the genome of smokers, thousands of mutations have already been identified that affect the likelihood of starting or quitting smoking and determining the severity of nicotine addiction. The data obtained can help in the creation of new tools for quitting smoking or help select the most effective of those already available [26].
Tobacco is stronger than marijuana
Comparative studies have shown that tobacco causes physiological dependence more than caffeine and marijuana, “losing” to alcohol, heroin and cocaine. As for psychological addiction, it is ahead of everyone, including heroin and cocaine. This is because nicotine increases the level of dopamine (also called the pleasure hormone) in the brain and, at the same time, smoking suppresses monoamine oxidase, a special enzyme that breaks down dopamine. The brain receives pleasure signals, but quickly gets used to the increased pleasure. Over time, the dose is required more and more, but the pleasure becomes less and less
. A drug is a drug.
And the smoke of the fatherland is sweet and pleasant to us...
The popularization of smoking began about a hundred years ago, and since then the number of smokers has been growing steadily. Today there are about a billion smokers living on Earth. However, in recent decades there has been a trend towards a decrease in the proportion of smokers in the population. Thus, in 1980, 40% of men and 10% of women in the world smoked daily; in 2012, these numbers dropped to 30% and 6%, respectively.
The popularity of smoking is falling globally, but unfortunately not in Russia, where 38 million people smoke on average more than 20 cigarettes a day, the same as 40 years ago. Russia today ranks second in the world in tobacco consumption after China [27].
We can only hope that the development of tobacco legislation in Russia will soften these harsh statistics, but we must remember that responsibility for our health lies primarily with ourselves, and not with the state.
I wish you good health, your author, a former smoker with five years of experience.
What to do next?
Avoid situations that provoke smoking. Don't go on smoke breaks with everyone else, it will be difficult for you to give up a cigarette, and you will automatically become a passive smoker.
Find a like-minded person, quit smoking together, support and morally help each other.
Practice self-hypnosis or autogenic training. Repeat to yourself more often: “Smoking disgusts me,” “It’s easier to breathe when you don’t smoke,” “I’m no longer drawn to a cigarette. My complexion has improved, my hair and clothes don’t smell of tobacco. The bad breath is gone." Say these phrases constantly when you wake up or fall asleep, when you really want to smoke.
Literature
- Kroemer N. B., Guevara A., Vollstädt-Klein S., Smolka M. N. (2013). Nicotine alters food-cue reactivity via networks extending from the hypothalamus. Neuropsychopharmacology, 38, 2307–2314;
- Randall RV The history of tobacco. Boston: Boston University Medical Center, 1999;
- King James I of England. A counterblast to tobacco (1604). London: G. Putnam and Sons, 1905;
- Borio G. (2003). Tobacco Timeline: The Seventeenth Century—The Great Age of the Pipe. Website tobacco.org;;
- Kaminsky M. Ein primäres Lungencarcinom mit verhornten Plattenepithelien. Greifswald: Inaug. Diss. Germany, 1898;
- Formation of the resting membrane potential;
- Nobel Prize in Physiology or Medicine (2013): vesicular transport;
- How does neurotransmitter release occur?
- The molecule of sanity;
- https://biomolecula.ru#;
- Kolappan C, Gopi P G (2002). Tobacco smoking and pulmonary tuberculosis. Thorax, 57, 964–966;
- Klareskog L., Stolt P., Lundberg K., Källberg H., Bengtsson C., Grunewald J. et al. (2006). A new model for an etiology of rheumatoid arthritis: smoking may trigger HLA-DR (shared epitope)-restricted immune reactions to autoantigens modified by citrullination. Arthritis Rheum. 54 (1), 38–46;
- Modestou M. A., Manzel L. J., El-Mahdy S., Look DC (2010). Inhibition of IFN-gamma-dependent antiviral airway epithelial defense by cigarette smoke. Respira. Res. 11, 64;
- Parkes G. C., Whelan K., Lindsay J. O. (2014). Smoking in inflammatory bowel disease: impact on disease course and insights into the aetiology of its effect. J. Crohns. Colitis. 8 (8), 717–725;
- Lee S.H., Goswami S., Grudo A., Song L.Z., Bandi V., Goodnight-White S. et al. (2007). Antielastin autoimmunity in tobacco smoking—induced emphysema. Nat. Med. 13, 567–569;
- Toda N. and Toda H. (2010). Nitric oxide-mediated bloodflow regulation as affected by smoking and nicotine. Eur. J. Pharmacol. 649, 1–13;
- Smoking harms the Y chromosome;
- Drug delivery based on receptor-mediated endocytosis;
- Takajo Y., Ikeda H., Haramaki N., Murohara T., Imaizumi T. (2001). Augmented oxidative stress of platelets inchronic smokers. Mechanisms of impaired platelet-derived nitric oxide bioactivity and augmented platelet aggregability. J. Am. Coll. Cardiol. 38 (5), 1320–1327;
- Moore D., Aveyard P., Connock M., Wang D., Fry-Smith A., Barton P. (2009). Effectiveness and safety of nicotine replacement therapy assisted reduction to stop smoking: systematic review and meta-analysis. BMJ, 338 , b1024;
- Tutka P. and Zatoński W. (2006). Cytisine for the treatment of nicotine addiction: from a molecule to therapeutic efficacy. Pharmacol. Rep. 58 (6), 777–798;
- West R., Zatonski W., Cedzynska M., Lewandowska D., Pazik J., Aveyard P., Stapleton J. (2011). Placebo-controlled trial of cytisine for smoking cessation. N.Engl. J. Med. 365 (13), 1193–1200;
- Mills E. J., Wu P., Spurden D., Ebbert J. O., Wilson K. (2009). Efficacy of pharmacotherapies for short-term smoking abstinence: A systematic review and meta-analysis. Harm reduction. J. 6, 25;
- Wu P., Wilson K., Dimoulas P., Mills E. J. (2006). Effectiveness of smoking cessation therapies: a systematic review and meta-analysis. BMC Public Health. 6, 300;
- Kosten T. R. and Domingo C. B. (2013). Can you vaccinate against substance abuse? Expert Opin. Biol. Ther. 13 (8), 1093—1097;
- Thank you, dear Ministry of Health, for warning me!;
- Ng M., Freeman MK, Fleming TD, Robinson M., Dwyer-Lindgren L., Thomson B. et al. (2014). Smoking prevalence and cigarette consumption in 187 countries, 1980-2012. JAMA. 311 (2), 183–192..