The series of January holidays has ended, and with it the rich meals that lasted for 10 days this year. This could not but affect the general well-being of the gastrointestinal tract. Which only takes a couple of days to “go astray” due to gluttony. All this requires restoration, because microflora and the digestive process play an extremely important role in our body. Starting from the formation of immunity, ending with the complete absorption of nutrients.
Today we suggest you consider the drug Linex. We'll tell you when and how to take it correctly.
How to take Linex and antibiotic correctly
If the patient has been prescribed antibacterial therapy, you should not wait for the first symptoms to appear, which will indicate a microflora disorder. When taking antibiotics, not only pathogenic microorganisms suffer, but also beneficial ones that participate in the digestive process. Therefore, the main rule for simultaneous use of Linex with antibiotics is that the course of Linex should be started on the same day when the first dose of antibacterial medication was taken.
It is better if the patient refers to the instructions for the antibiotic. In it, you need to pay special attention to the section on the half-life of the drug. It is at this interval that it would be wise to drink Lines in order to achieve the best effect.
Contraindications
Intolerance to drug components or dairy products (lactose), fructose.
Special Recommendations
- Linex should never be washed down with hot drinks or taken with alcohol, because this destroys beneficial bacteria.
- If you have a temperature above 38 degrees, there are traces of blood or mucus in the stool, diarrhea lasts more than 2 days with acute abdominal pain, dehydration and weight loss, have chronic diseases such as diabetes, you should consult a doctor before taking the drug.
- When using the drug during the treatment of diarrhea, you should constantly replenish lost fluid and electrolytes in the body.
- The composition of the drug allows it to be taken simultaneously with other medications, even with antibiotics and chemotherapy drugs.
- Linex does not have any effect on psychophysical activity.
Linex for newborns and children
After birth, children begin to adapt to the new extrauterine world and form their own microflora due to contact with the environment. In the first months of a baby’s life, this process is accompanied by colic, constipation or diarrhea, so according to true indications, you can help his body.
It is recommended for a newborn child up to one year to take drops, and from one year to 7 years, you can take the medicine in sachet form.
Linex and digestion
Linex restores and supports digestion, namely, restores the intestinal microflora and stabilizes the functions of the gastrointestinal tract.
Linex and chronic diseases
Linex can be taken for chronic diseases. But if you have diabetes or immunological deficiencies (AIDS, HIV), you should definitely consult a doctor. The doctor must select a course of treatment, if necessary. In case of intolerance, prescribe an analogue.
Linux and alcohol
The medicine restores the microflora, and alcohol only causes harm. It puts stress on the kidneys and liver and promotes the production of toxins. Alcohol damages the capsule shell, and the beneficial microorganisms included in it die. Linex and alcohol are two incompatible products.
How to properly breed Linex for children
For babies, there is a powder form of Linex, which is packaged in sachets. The powder is identical to that contained in the adult capsule shell. Infants are prescribed Linex as a preventive measure for intestinal colic between the ages of 3 weeks and 3 months. The powder can be diluted in an adapted milk formula if the child is bottle-fed. If you are breastfeeding, you can express some breast milk into a bowl to dilute the powder in it. You can give your child the mixture prepared in this way from a teaspoon.
Instructions for use
Newborn babies and children under 2 years of age can be given 1 capsule 3 times a day. A child aged 2-12 years can be given no more than 2 tablets 3 times a day. Children over 12 years of age and adults can take 2 capsules 3 times a day.
If the drug is prescribed to a child over 6 years of age who has diarrhea, the medication should be taken under the supervision of a doctor. The method of administration and permissible dosage are established taking into account the severity of the child’s condition. If diarrhea does not resolve within 48 hours, a change in treatment regimen will be required.
If the child is very small and has problems swallowing capsules, then you can split them and pour the contents into 1 tsp. drinking water. The resulting mixture must be taken immediately.
Since gastric juice can have a negative effect on lactobacilli, it is better to take the drug with food.
Capsules should not be taken with alcohol or hot liquid.
The duration of the treatment course is determined by a specialist. If no adverse reactions occur, then Linex can be taken until the patient’s condition completely improves. In some cases, it is recommended to take more medicine 2 days after the condition improves.
Linux for children: what helps
Babies that are born still have a sterile intestine, which is not inhabited by any bacteria. Having passed through the mother's birth canal, taking the mother's breast into his mouth for the first time, the child receives the first portion of bacteria, which, of course, is not enough to ensure a complete digestion process.
At three weeks of age, newborns experience infantile colic. This is due to the fact that it is difficult for the intestines to process the lactose contained in milk. Hence the flatulence and spasms. To help the child adapt to the environment and teach the intestines to break down lactose, children are given Linex. It populates the gastrointestinal tract with all the necessary types of bacteria, due to which the severity of colic is reduced, the child becomes calmer, sleeps better, and more actively absorbs nutrients from food.
Pharmacology
Linex is a drug of combined action. It contains 3 important bacteria that are able to maintain normal microflora in the intestines.
Microorganisms, penetrating the human body, activate the regulation of microflora and help maintain its natural balance.
Bacteria take an active part in the production of beneficial vitamins. Improvement in well-being occurs due to the fact that lactic acid bacteria prevent harmful microbes from attaching to the intestinal walls.
The active substances produce bacteriocins, which are responsible for antibacterial activity. Under their influence, immunity in the intestines is stimulated.
As a result, Linex allows you to stabilize the intestinal microflora and restore the disturbed balance of microorganisms, as a result of which microbial and bacterial infections appear and spread in the body. The occurrence of such infections is associated with taking various medications and antibiotics.
Preclinical studies classify Linex as a probiotic. Consequently, it is absolutely harmless and does not have any negative or toxic effects on the human body.
How much to drink Linex for thrush
Thrush is a fungal infection that affects the genitals of both men and women. The causative agent is a fungus - candida, which in itself is not a pathogenic flora. A large percentage of people are carriers of candida, which live in the intestines without causing any negative reactions.
This healthy state of the intestines containing candida fungi is explained by the “armed truce” of the flora. In other words, the intestines maintain a balance in the number of bacteria and fungi, which inhibit the reproduction of each other. As soon as for some reason there are fewer beneficial bacteria than fungi, candidiasis develops.
Linex restores the balance of the flora, as a result of which thrush recedes. To speed up recovery, you can apply antifungal agents topically and supplement therapy with a course of Linex until complete recovery.
Intestinal dysbiosis and antibiotic-associated diarrhea, diagnosis and treatment
The study of intestinal microflora began in 1886, when F. Escherich described Escherichia coli (Bacterium coli communae). In 1908, Nobel laureate Russian scientist Ilya Ilyich Mechnikov proved the necessity of intestinal bacteria for health and longevity. To date, the presence of 500 types of microbes has been established in the intestines of a healthy person. Normal microbial flora is one of the barriers to bacteria entering the intestines. It stimulates immune defense and increases the secretion of IgA into the intestinal lumen. Escherichia coli, enterococci, bifidobacteria, acidophilus bacilli have antagonistic properties and are able to suppress the growth of pathogenic microorganisms. Violation of the microflora composition leads to a decrease in the body's resistance to intestinal infections.
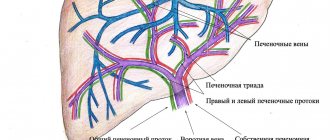
There are mucoid microflora (M-microflora) - microorganisms associated with the intestinal mucosa, and cavity microflora (P-microflora) - microorganisms localized in the intestinal lumen.
In relation to the macroorganism, representatives of the intestinal biocenosis are divided into 4 groups:
- obligate microflora (main intestinal microflora - bifidobacteria, lactobacilli, normal E. coli, propionobacteria, peptostreptococci, enterococci);
- facultative (opportunistic and saprophytic microorganisms - bacteroides, staphylococci, streptococci, peptococci, yeast-like fungi, veyonella, fusobacteria, bacilli);
- transient (occasional microorganisms that are not capable of long-term residence in the body - flavobacteria, pseudomonads);
- pathogenic (pathogens of infectious diseases - Shigella, Salmonella, Yersinia, etc.).
When microbes utilize indigestible carbohydrates (fiber), short-chain fatty acids are formed. They provide intestinal cells with energy carriers, improving the trophism of the mucous membrane. Insufficient fiber in the diet leads to decreased synthesis of short-chain fatty acids. As a result, dystrophic changes in the epithelium occur and the permeability of the intestinal barrier to antigens of food and microbial origin increases.
Under the influence of microbial enzymes in the ileum, bile acids (BAs) are deconjugated and primary FAs are converted into secondary FAs. Under physiological conditions, 80–95% of FAs are reabsorbed, the rest are excreted in the feces in the form of metabolites. The latter promote the formation of feces, inhibit the absorption of water, preventing excessive dehydration of feces. Excessive bacterial contamination of the small intestine leads to premature deconjugation of fatty acids and secretory diarrhea.
Thus, the morphological and functional state of the intestine depends on the composition of its microflora.
In the jejunum of healthy people there are up to 100,000 bacteria per 1 ml of contents. The main part of them are streptococci, staphylococci, and lactic acid bacilli. In the distal ileum, the number of microbes increases due to enterococci, Escherichia coli, bacteroides and anaerobic bacteria.
The microbial composition of feces does not reflect the complete picture of the intestinal biocenosis and does not provide operational information about the composition of microorganisms in the intestine. In practice, data on only 15–20 types of microbes contained in feces are taken into account. Usually the number of bifidobacteria, lactobacilli, enterobacteria, E. coli, Proteus, Enterococcus, Staphylococcus aureus, Pseudomonas aeruginosa and Candida are examined.
Intestinal dysbiosis is a violation of the ecological balance of microorganisms, characterized by a change in the quantitative ratio and qualitative composition of indigenous microflora in the microbiocenosis. The term “dysbacteriosis” was first introduced by A. Nissle in 1916.
The severity of dysbiosis is determined by the degree of decrease in bifidobacteria and other obligate microorganisms and an increase in the number of opportunistic and pathogenic species.
I degree - a decrease in the number of obligate representatives (bifidobacteria and/or lactobacilli) by 1–2 orders of magnitude, without an increase in opportunistic microflora (OPM), an increase in the number of OPM with a normal number of bifidobacteria. II degree - moderate or significant decrease in the number of bifidobacteria, combined with pronounced changes in aerobic microflora (reduction of lactobacilli, appearance of altered forms of Escherichia coli, UPM in high quantities). III degree - a large number of UPM, both of one type and in associations, isolation of pathogenic microorganisms (Mekhtiev S.N., Grinevich V.B., Zakharenko S.M.).
In the clinic of dysbiosis, the following key syndromes are distinguished:
- dyspeptic (decreased appetite, regurgitation, belching, nausea, vomiting);
- intestinal syndrome (bloating, rumbling intestines, tendency to constipation or loose stools with undigested food debris);
- secondary malabsorption syndrome (persistent diarrhea with impaired absorption of monosaccharides and electrolytes),
- polyhypovitaminosis (dry skin, hair loss, brittle nails, cheilitis, stomatitis).
New approaches to the diagnosis of dysbiosis
An alternative to routine bacteriological studies is chemical methods for differentiating microorganisms and, in particular, gas chromatography (GC) combined with mass spectrometry (GC-MS). The method is based on identifying the components of bacterial cells that appear as a result of their natural death or attack by the immune system. Minor lipid components of microbial membranes are used as markers. Based on their content, up to 170 species of bacteria and fungi in various biological environments can be determined within a few hours.
Almost 50% of the biomass of the wall microflora are actinomycetes, which occupy an intermediate position between bacteria and fungi. About 25% of the microbial flora is represented by aerobic cocci (staphylococci, streptococci, enterococci and coryneform bacteria). The number of bifido- and lactobacilli ranges from 20 to 30%. Other anaerobes (peptostreptococci, bacteroides, clostridia, propionobacteria) make up about 10% in the small intestine and up to 20% in the large intestine. Enterobacteriaceae account for 1% of the total number of microflora of the mucous membrane.
Up to 90–95% of colon microbes are anaerobes (bifidobacteria and bacteroides) and only 5–10% of all bacteria are strict aerobic and facultative flora (lactic acid and E. coli, enterococci, staphylococci, fungi, proteus).
Dysbiosis is not an independent disease. Its appearance is facilitated by disorders of intestinal digestion, motility, local immunity, antibiotics, antacids and other medications. It is necessary to establish the cause that caused dysbiosis, and not try to “cure” the intestinal microflora based on its bacteriological analysis of stool.
The properties of microbes inhabiting the intestines are not always taken into account when prescribing antibiotics. Antibacterial drugs suppress the growth of not only pathogenic microorganisms, but also normal microflora. As a result, saprophytic microbes with high resistance to drugs multiply and acquire pathogenic properties.
Antibiotic-associated diarrhea
Patients receiving antibiotic therapy may develop diarrhea caused by intestinal dysbiosis (AAD - antibiotic-associated diarrhea). The frequency of such diarrhea ranges from 5–25%. The reason for this is a decrease in the number of microbes sensitive to the antibiotic and the emergence of resistant strains that are not normally present. The most well-known representative of such microorganisms is the pathogenic strain Clostridium difficile (Cl. difficile), but the cause of diarrhea associated with antibiotics can also be other microbes that can enhance the secretion of ions and water and damage the intestinal wall. These are staphylococci, Proteus, yeast fungi, enterococci, Pseudomonas aeruginosa, Klebsiella. Based on the type of diarrhea, AAD is usually classified as secretory and inflammatory types.
Antibiotic-associated diarrhea is most often caused by lincomycin, ampicillin, clindamycin, benzylpenicillin, cephalosporins, tetracyclines, and erythromycin. The method of administration of the antibiotic does not matter much. When taken orally, in addition to the eradication of microorganisms, the antibiotic affects the mucous membrane of the small intestine. When administered parenterally, antibiotics affect the intestinal biocenosis, excreted with saliva, bile, and secretions of the small and large intestines.
Symptoms of AAD in most patients usually appear during treatment, and in 30% - within 7-10 days after its cessation.
Most researchers consider clostridia, in particular Cl., to be the etiological factor of AAD. difficile. Among the adult population, the level of its carriage is low and equal to 2–3%. Reproduction conditions for Cl. difficile are an anaerobic environment and suppression of normal intestinal microflora.
Clinical manifestations of AAD range from mild diarrhea to severe pseudomembranous colitis (PMC). MVP is an acute intestinal disease that is a complication of antibacterial therapy. It has been established that it is caused by Cl. difficile.
Symptoms
The main symptom of AAD is profuse, watery diarrhea, the onset of which is preceded by the administration of antibiotics for several days or more. Then cramping pain in the abdomen appears, subsiding after stool. In cases where fever occurs, leukocytosis increases in the blood, and leukocytes appear in the stool, PMH should be suspected.
After discontinuation of the antibiotic, in some patients the symptoms quickly disappear. With MVP, despite the cessation of antibiotic therapy, in most cases the frequency of stool increases, dehydration and hypoproteinemia appear. In severe cases, dehydration quickly sets in, toxic dilatation and perforation of the colon develop, and death is possible.
Diagnosis
The diagnosis of AAD is made based on the association of diarrhea with the use of antibiotics. The diagnosis of MVP is confirmed by bacteriological examination of stool and determination of the Cl toxin in it. difficile. The frequency of detection of the toxin in the stool of patients with AAD does not exceed 15%.
In patients with diarrhea associated with Cl. difficile, significant leukocytosis is observed. There is evidence that patients with leukocytosis of 15800 and above are highly likely to develop MVP caused by Cl. difficile. This is explained by the fact that toxin A, secreted by Cl. difficile causes inflammation, fluid secretion, fever and convulsions. Therefore, in all patients with AAD, occurring with intoxication and leukocytosis, 15800 and above should be considered the cause of diarrhea Cl. difficile.
Parfenov A.I., Osipov G.A., Bogomolov P.O used the GC-MS method to assess the composition of the microbial flora of the small intestine in 30 patients with AAD and found that diarrhea can be associated not only with an infectious agent (Cl. difficile) , but with a significant change in the normal microflora towards an increase in the number of 7 to 30 out of 50 controlled microorganisms. In this case, the total colonization of the small intestine increases 2–5 times compared to the norm.
In patients with AAD, most often there are no morphological changes in the colon. In severe cases, endoscopy reveals 3 types of changes: 1) catarrhal inflammation (swelling and hyperemia) of the mucous membrane; 2) erosive-hemorrhagic lesion; 3) pseudomembranous lesion.
The endoscopic picture of MVP is characterized by the presence of plaque-like, ribbon-like and solid “membranes”, soft but tightly fused to the mucous membrane. The changes are most pronounced in the distal parts of the colon and rectum. The mucous membrane is edematous, but not ulcerated. Histological examination revealed subepithelial edema with round cell infiltration of the lamina propria, capillary stasis with the release of red blood cells outside the vessels. At the stage of formation of pseudomembranes, infiltrates are formed under the surface epithelium of the mucous membrane. The epithelial layer is raised and absent in places: the bare areas of the mucous membrane are covered only by desquamated epithelium. In later stages of the disease, these areas may occupy large segments of the intestine.
Differential diagnosis
The association of diarrhea with antibiotic therapy usually does not create difficulties in diagnosing AAD. In severe cases, the picture of MVP may resemble cholera or a fulminant form of ulcerative colitis, Crohn's disease. However, the latter are characterized by more or less pronounced bloody diarrhea, which is not typical for MVP. Nevertheless, the possibility of developing erosive-hemorrhagic changes in the mucous membrane during AAD does not exclude the appearance of bloody discharge from the rectum in some patients.
Treatment of AAD
Etiotropic therapy of AAD and MVP caused by Cl. difficile, most authors consider the prescription of vancomycin and metronidazole (Trichopol, Metrogyl).
Immediately discontinue the antibiotic that caused the diarrhea. Vancomycin is prescribed at an initial dose of 125 mg orally 4 times a day, if necessary, the dose is increased to 500 mg 4 times a day. Treatment is continued for 7–10 days. Metronidazole is given 0.5 g orally 2 times a day (or 0.25 g 4 times a day).
Bacitracin is also used at a dose of 25 thousand IU orally 4 times a day. Treatment is carried out for 7–10 days. Bacitracin is almost not absorbed, resulting in a high concentration of the drug in the colon. For dehydration, infusion therapy and oral rehydration (Regidron, Citroglucosolan) are used. Cholestyramine is prescribed to bind toxin A.
There are reports of the possibility of treating AAD also with large doses of probiotics. S. Perskyp and L. Brandt (2000) found that normal human microflora is able to eliminate diarrhea caused by Cl. difficile. The bactericidal effect of normal microflora ensures recovery in more than 95% of patients with AAD associated with Cl. difficile. It prevents the appearance of chronic clostridial and other infections, which can cause chronic gastrointestinal disorders in some patients. Probiotic therapy for AAD and MVP should be started as early as possible, without waiting for confirmation of the diagnosis.
Since the number of microbes that provide a therapeutic effect is several orders of magnitude higher than the doses of conventional bacterial preparations, the issue of local delivery of probiotics to the intestines is being discussed. This can be done using saline enemas, a nasoduodenal tube, or a colonoscope. The latter method attracts attention because it involves introducing probiotics directly into the proximal colon.
One of the main probiotic drugs used to treat AAD is Linex. This is a combined drug containing components of natural microflora from different parts of the intestine. Containing bifidobacteria, lactobacilli and non-toxigenic lactic acid enterococcus maintain the balance of intestinal microflora and ensure its physiological functions: create unfavorable conditions for the reproduction and activity of pathogenic microorganisms; participate in the synthesis of vitamins B1, B2, PP, folic acid, vitamins K and E, ascorbic acid, provide the body with vitamins B6, B12 and biotin; by producing lactic acid and reducing the pH of the intestinal contents, they create favorable conditions for the absorption of iron, calcium, and vitamin D. Lactic acid bacteria carry out the enzymatic breakdown of proteins, fats and complex carbohydrates; carbohydrates and proteins that are not absorbed in the small intestine undergo deeper breakdown in the large intestine by anaerobes ( including bifidobacteria). The bacteria that make up the drug are involved in the metabolism of bile acids.
Linex contains lactic acid bacteria that are resistant to antibiotics. Adults and children over 12 years of age are prescribed 2 capsules 3 times a day after meals with a small amount of liquid. The duration of treatment is on average 1–2 months. When using the drug in recommended doses, no side effects were noted. Contraindications: hypersensitivity to the components of the drug or dairy products. Studies have not revealed that Linex has a teratogenic effect, and no negative effects of the drug have been reported during pregnancy and lactation. To preserve the viability of the components of the drug, it is not recommended to drink Linex with hot drinks; you should refrain from drinking alcohol.
The clinical manifestations of an allergy to lactic acid bacteria are similar to those of an allergy to dairy products, therefore, if allergy symptoms appear, the drug should be stopped to determine its causes. There have been no reported cases of Linex overdose. There were no undesirable interactions with other drugs. The composition of Linex allows it to be taken simultaneously with antibacterial agents.
For the symptomatic treatment of diarrhea, the following are also used: attapulgite adsorbent, 1.2–1.5 g after each loose stool; loperamide, 2–4 mg orally after each bowel movement (not more than 8 mg/day); diphenoxylate/atropine (Lomotil), 5 mg orally 4 times daily until diarrhea stops; belladonna tincture, 5–10 drops orally 3 times a day before meals; hyoscyamine (Levsin) 0.125 mg sublingually as needed or 0.375 mg orally 2 times a day; antispasmodic dicycloverine, 20 mg orally 4 times a day; codeine, 30 mg orally 2–4 times a day; octreotide (100–600 mg/day subcutaneously in 2–4 doses) is a synthetic analogue of somatostatin; enterosorbents (Smecta, Espumisan).
Treatment of dysbiosis itself
Standard therapy for dysbiosis is aimed at eliminating excess bacterial contamination of the small intestine, restoring normal microflora, improving intestinal digestion and absorption, restoring intestinal motility and increasing the body's immunoreactivity.
Antibacterial drugs are used according to indications to suppress the growth of pathogenic microflora in the small intestine. Antibiotics from the group of fluoroquinolones, penicillins, cephalosporins, tetracyclines or metronidazole are usually prescribed. The drugs are taken orally in normal doses for 7–10 days.
It is optimal to use agents that have a minimal effect on the symbiont microflora and suppress the growth of Proteus, staphylococci, yeasts and other aggressive strains. These include antiseptics: Intetrix, Enterol, Bactisubtil, Nifuroxazide, etc. For severe forms of staphylococcal dysbiosis, antibiotics are used: ofloxacin, oxacillin, amoxicillin. They are prescribed for a period of 10–14 days. If fungi appear in feces or intestinal juice, the use of natamycin, fluconazole and other mycostatics is indicated.
Bacterial preparations (probiotics) can be prescribed without prior antibiotic therapy or after it. They use Bifidumbacterin, Probifor, Bificol, Lactobacterin, Linex, Bifiform, Normoflorin L, D, B, Polybacterin, Narine, Acipol, Nutrolin V, Travis.
Another way to treat dysbiosis is to influence pathogenic microbial flora with metabolic products of normal microorganisms (prebiotics). One of these drugs is Hilak-Forte, a sterile concentrate of metabolic products of normal microflora: lactic acid, lactose, amino acids and fatty acids. These substances help restore the biological environment in the intestines necessary for the existence of normal microflora, suppress the growth of pathogenic bacteria, and improve the trophism and function of epithelial cells and colonocytes. One milliliter of the drug contains biologically active substances of 100 billion normal microorganisms. Hilak-Forte is prescribed 60 drops 3 times a day for a period of 4 weeks in combination with antibacterial drugs or after their use.
In addition, lactulose syrup (Duphalac, Portalac) is used, which acidifies intestinal juice and inhibits the growth of pathogenic microflora. The active substance is a synthetic disaccharide that is not hydrolyzed in the small intestine and enters the colon unchanged, where it is broken down under the influence of colon flora to form low molecular weight organic acids, which leads to a decrease in the pH of the intestinal contents.
Under the influence of the drug, the absorption of ammonia by the colon and its removal from the body increases, the growth of acidophilic bacteria (including lactobacilli) is stimulated, the proliferation of proteolytic bacteria is suppressed and the formation of nitrogen-containing toxic substances is reduced. The clinical effect occurs after 2 days of treatment. The drug in the form of a syrup for oral administration is prescribed to adults at a dose of 15–45 ml/day, the maintenance dose is 10–25 ml/day. The drug should be taken 1 time/day in the morning with meals, with water or any other liquid or food.
Side effects from the digestive system: in the first days - flatulence (which goes away on its own after 2 days); with long-term use in high doses, abdominal pain and diarrhea are possible. Contraindications: galactosemia; intestinal obstruction; hypersensitivity to the components of the drug. Lactulose can be used during pregnancy and lactation according to indications. The drug should be prescribed with caution to patients with diabetes mellitus.
Other prebiotics include calcium pantothenate (participates in the processes of acetylation and oxidation in cells, carbohydrate and fat metabolism, acetylcholine synthesis, is utilized by bifidobacteria and helps increase their mass), aminomethylbenzoic acid (Pamba, Amben) - an inhibitor of fibrinolysis, inhibits proteolytic enzymes conditionally. pathogenic bacteria, stimulating the growth of normal microflora, lysozyme (has bifidogenic, immunomodulatory, anti-inflammatory effects, improves digestion, suppresses pathogenic flora).
It is recommended to use herbal remedies in the treatment of dysbiosis. They are intestinal antiseptics, suppress pathogenic microflora and preserve saprophytic microflora. Herbal infusions normalize appetite, improve digestion, intestinal motility, have antimicrobial and immunomodulatory effects, and promote mucosal regeneration. St. John's wort, calendula, eucalyptus, yarrow, bloodroot, sage, oregano, lingonberry, and plantain have a pronounced bactericidal effect. Nettle, lemon balm, coltsfoot, plantain, tricolor violet, and string have an immunocorrective effect. Lingonberries, nettles, raspberries, currants, rowan, and rose hips are rich in vitamins.
Patients with impaired cavity digestion are prescribed pancreatic enzymes (Creon, Pancitrate). To improve absorption function, Essentiale forte N, loperamide (Imodium) and trimebutine are used.
To increase the reactivity of the body in weakened patients with severe dysbiosis, it is advisable to prescribe Anaferon, Immunal, Likopid and other immunomodulators. The course of treatment should last an average of 4 weeks. At the same time, vitamin and mineral complexes are prescribed (Vitamineral, Alphabet, etc.).
For questions regarding literature, please contact the editor.
V. V. Skvortsov , Doctor of Medical Sciences Volgograd State Medical University , Volgograd
How many days should you take Linex?
Regardless of what reason provoked the imbalance of beneficial microorganisms in the intestines, Linex will help to cope with it. The duration of treatment directly depends on the symptoms and condition of the patient. As a rule, a 7-day course is enough to restore the functioning of the gastrointestinal tract. But in cases where the patient was prescribed antibacterial therapy lasting 10 days, taking Linex becomes longer. First of all, you should take the supplement throughout your course of antibiotics. After which it is better to continue drinking Linex for another week to help the body fully recover.
Linex tool
Creates and regulates the balance of intestinal microflora. The drug includes three main groups of bacteria - Lactobacilli, Bifidobacteria, Enterococci. And other auxiliary components. The bacteria were pre-dried and frozen. This manufacturing technology allows Linex to be stored at room temperature.
The bacteria included in the composition are identical to those found in the intestines. They oxidize the digestive environment, quickly and effectively restore microflora after taking antibiotics, certain diseases and their complications.
The medicine is suitable for people with good tolerance to fermented milk products. It is prescribed to both adults and children.
Linex composition and dosage
The capsule of the drug contains - Lebenin powder 280 mg, (1 gram of powder contains Lactobacillus - 300 mg, Bifidobacteria - 300 mg, Enterococcus 300 mg, as well as excipients lactose - 50 mg, potato starch - 50 mg.) and the excipient magnesium stearate – 8.4 mg.
The capsule shell consists of methylhydroxybenzoate - 0.19 mg, propylhydroxybenzoate - 0.08 mg, titanium dioxide 0.98 mg and gelatin up to 63 mg.
In powder form, the product has the following composition: lyophilized bifidobacteria powder - 100 mg, as well as an excipient - maltodextrin - 1400 mg.
Drops for children are also available. They contain: sucrose, sunflower oil, lyophilized bifidobacteria, maltodextrin, antioxidant sodium ascorbate.
Release form
- Linex is produced in capsules (packs of 16 and 23 capsules);
- Sachets in powder form (packs of 10 and 20 sachets);
- Linex drops for children are available in an 8 ml bottle with a dropper dispenser. The medicine is packaged in a cardboard box.
Each package of medicine contains printed instructions with graphic elements in the form of a logo that glow under UV radiation.
How to take Linex for constipation
Constipation is difficulty defecating or no bowel movements for three days in a row. If constipation occurs as a result of poor nutrition, Linex can help restore the formation and movement of stool lumps towards the exit. However, it is important to understand that one dose of Linex will not save you from chronic bowel dysfunction if the patient does not change his attitude towards food. It is important to increase the amount of fluid consumed, as well as fresh fruits and vegetables, which, thanks to their fiber, help facilitate bowel movements and form soft stools.