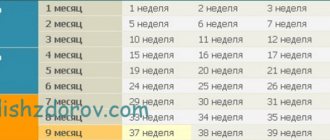
According to the recommendations of the World Health Organization, there are 4 categories of prematurity in infants:
- deep prematurity (up to 1 kg) - if birth occurred at 22–28 weeks (about 5% of the total number of births);
- heavy (up to 1.5 kg) - it accounts for 15%, 28–30 weeks;
- medium degree of prematurity (up to 2 kg) - covers about 20%, 31–33 weeks;
- mild degree (up to 2.5 kg) - children are born at 34–36 weeks.
In some maternity hospitals, the period is still counted from 28 weeks, due to the lack of equipment for caring for this group of babies.
Interesting Facts
| Options | Indications |
| Time from conception | 34 weeks |
| Period by month | 36 weeks |
| What month | 9 |
| Dimensions and weight of the fetus | 475 mm, 2600 g |
| Uterus dimensions | VDM - 32-34 cm |
| Pregnant weight | Gain from the beginning of pregnancy is 10-14 kg; over the last week 400-500 g |
Your baby is the size of
Papaya
475 mm Size
2600 g Weight
Congratulations! You are at the finish line. By the end of the 36th week of pregnancy, all organs and systems of the baby are fully formed. Now he is engaged in building up fat tissue. Your task is to accumulate strength, rest at the first opportunity and tune in to a positive mood.
Treatment for premature birth
The goal is to reduce the tone of the myometrium and reduce uterine contractions. This is achieved by blocking oxytocin receptors - it is the hormone oxytocin that triggers the birth process.
Such oxytocin receptor antagonists are tocolytics. One of the modern representatives of this group of drugs is atosiban.
The product is effective, but has contraindications. It is prohibited to administer treatment to pregnant women less than 24 and more than 33 weeks pregnant, with uterine bleeding, growth retardation, distress or intrauterine fetal death, severe preeclampsia, rupture of the membranes after 30 weeks, placenta previa or abruption.
5 stages of preterm labor management
Stage one is predicting their occurrence. Depends on the situation: the process is starting, has begun, or we are talking about its threat.
Stage two is the prevention of respiratory distress syndrome in a child. Doctors stimulate lung maturation. Drugs from the group of glucocorticoids are used.
Stage three - prolongation of pregnancy. Doctors are trying to delay premature birth - to give the baby's lungs and placenta time to mature. For this purpose, tocolytics are used - they inhibit the contractile activity of the uterus. Prevention is usually carried out - tocolysis is carried out before contractions. Once started, therapy is ineffective. Duration of treatment is a maximum of 48 hours.
Stage four is preparation for the birth of a premature baby. The woman in labor is transferred to a higher level hospital. The physiology of premature birth is no different from the birth of a child at term. But doctors require close attention to minimize complications for mother and baby.
Stage five - prevention of infections and their complications. At risk are women in labor whose waters have broken. If the patient gives birth before 34 weeks, she may be given a course of dexamethasone. It accelerates the maturation of the placenta and internal organs of the baby, reducing the risk of complications.
Feelings of the expectant mother
Due to your heavier belly, enlarged breasts and stiffness in your movements, you may feel tired and overwhelmed at 36 weeks. But breathing, most likely, has become easier, and the heartburn has subsided, because at this stage the stomach drops into the pelvis, and the uterus no longer puts pressure on the diaphragm and stomach.
Precursors of labor in first-time mothers
About 2 weeks before the expected birth, instead of progesterone, estrogens begin to play a dominant role in the hormonal background, the concentration of which determines the rate of dilatation of the cervix at the onset of labor. A pregnant woman may feel the following changes in sensations and well-being:
- weight loss and disappearance of swelling - this is how the body gets rid of excess fluid before childbirth;
- changes in stool - thinning to the point of diarrhea and frequent urges - another way to eliminate fluid;
- discharge of the mucus plug from the cervical canal - this is a jelly-like discharge, light or yellowish, sometimes mixed with blood;
- training contractions are chaotic contractions of the uterus that last a few seconds; the woman notes that she is pulling in her lower abdomen, but the pain goes away on its own.
Multiparous women experience the same symptoms, the only difference is that they may appear 1-2 weeks earlier and be more pronounced also because an experienced mother can already distinguish them from other conditions.
Prevention of premature birth
It is divided into 2 stages: before conception and after.
Preventive measures before conception
It is advisable to carry them out to mothers from the risk zone. The gynecologist limits intrauterine manipulations, such as curettage. During IVF, the number of embryos for transfer is regulated taking into account the age of the expectant mother and her health. Inform about the possibility of premature birth during conception through reproductive technologies.
Hydration is indicated - increased drinking regimen. It improves fetoplacental blood flow and reduces the risk of premature birth.
Eliminate infections. It is advisable to do this at the planning stage, since treatment with antibiotics during pregnancy is harmful to the fetus.
It is recommended to wait until after the birth of an older brother or sister to conceive a child. Mommy's body needs to recover from the previous pregnancy. This requires him at least 2 years. During this time, the uterus will return to its previous state, strength, vitamin reserves and body reserves will be restored.
If there is a predisposition to premature birth, vitamin complexes are prescribed for planning and expectant mothers. Protein-rich dietary supplements are beneficial. They strengthen the immune system, improve blood circulation, protect the pregnant woman from infections - and therefore the child.
Secondary prevention of early delivery
If there is a threat of premature birth, the pregnant woman’s condition is monitored at critical periods: from 2 to 12 and from 18 to 22 weeks. During these periods, it is better to stay in the hospital of the perinatal center. Doctors prescribe medications to maintain and prolong pregnancy.
Therapy is selected on an individual basis.
With a short cervix from 1 to 2.5 cm, progesterone suppositories are prescribed vaginally. The hormone is also indicated for previous premature births. This tactic reduces their risk by 35%. We are talking about a natural hormone. It is effective and safe. It is prescribed in the first trimester. The synthetic hormone is harmful: it can cause gestational diabetes.
If there is a threat of early birth of the baby, stitches are placed on the neck. An expectant mother outside the risk zone may not need stitches in this situation.
Another option is to install a pessary on the neck.
These methods reduce the statistics of premature births. But the incidence of newborn mortality is not affected.
When carrying twins, circular or U-shaped sutures can be applied. In most cases, such tactics with a short cervix during multiple pregnancies can provoke premature birth. Vaginal progesterone is not prescribed.
For infections (for example, bacteriuria, gonococcus, syphilis, β-hemolytic streptococcus, bacterial vaginosis, chlamydia), antibacterial prophylaxis is prescribed. Depending on the diagnosis, penicillin, ampicillin, metronidazole, erythromycin, ceftriaxone, and josamycin may be prescribed.
conclusions
Premature birth is one of the fears of many expectant mothers. No one is immune from this. But you can minimize the risks. Follow the recommendations of the gynecologist, take care of yourself, listen to your body, and do not refuse to remain in the hospital at the perinatal center.
Don't think negative thoughts. Modern medicine successfully cares for premature babies and reduces the risks of complications and consequences.
What happens to the fetus
At 36 weeks of pregnancy, the baby's weight averages 2.6 kg, and it becomes increasingly difficult for him to move freely. Therefore, the mother feels all the movements and even the way the child hiccups quite clearly. Usually by this time the fetus is turned head down, arms and legs are pressed to the body. He will remain in this position until he is born.
There is less lanugo and cheese-like lubricant on the baby’s body. The baby swallows them along with the amniotic fluid, which is how meconium is formed - the baby's first stool.
Who's at risk
Any pregnant woman can give birth prematurely. Some expectant mothers have a higher chance of giving birth prematurely. Pregnant women at risk include:
- under 17 and over 35 years old;
- carry more than one fetus;
- have structural features of the uterus or its cervix;
- use harmful substances - drugs, alcohol, smoke;
- have heavy physical activity;
- have experience of premature birth;
- work in hazardous work;
- are subjected to sexual and emotional violence, stress, and mental stress.
Expectant mothers who did not register during pregnancy or ignore ultrasound, screenings, and laboratory tests are at risk.
The threat of early premature birth is more common with diagnoses: diabetes, anemia, hypertension, genitourinary infections, hypothyroidism, weight problems before conception (deficiency or obesity), thrombophilia, vaginal bleeding. There is also a risk when conceiving through IVF, with congenital malformations of the fetus.
If a woman has previously given birth to a child prematurely, the chances of premature birth remain in subsequent pregnancies. The same applies to the weight of the baby: if the first-born was born with a deficiency of body weight, then his brother or sister may also be underweight.
Risk factors
Doctors point to a number of factors that take place long before a child is conceived. These include:
- Gynecological diseases suffered in childhood or adolescence;
- Early onset of intimate life;
- Hereditary factor;
- Pathologies of previous pregnancy: gestosis, placental insufficiency, premature birth;
- Excessive distension of the uterus during multiple pregnancy, polyhydramnios;
- Threat of miscarriage in the early stages.
Another risk factor is surgery or trauma to the abdominal organs during pregnancy.
Tests and ultrasound
The thirty-sixth week of pregnancy is the optimal time for the following studies:
- biochemical blood test - to assess the general health of the mother, hemoglobin levels, hormones, etc.;
- test for HIV, sexually transmitted infections - to determine labor tactics;
- gynecological smear - will reveal the presence of pathogenic microflora;
- A general urine test will indicate possible problems in the functioning of the kidneys and urinary system.
You will also need to undergo a CTG: the fetal heartbeat can be used to diagnose hypoxia and other disorders in a timely manner.
Ultrasound at the 36th week of pregnancy is performed according to indications, if it has not been prescribed previously or for additional diagnostics with accompanying symptoms.
Nutrition
Nutrition of a pregnant woman at the 36th week of gestation
As we said earlier, nutrition from the 36th week needs to be reviewed. A woman should reduce the amount of meat she eats and increase the proportion of vegetables. It is advisable to consume them raw. This is necessary to increase the amount of fiber, which allows you to maintain normal digestion.
Additionally, from this period it is worth limiting the consumption of exotic fruits. It is recommended to organize nutrition in the last weeks before childbirth according to certain rules:
- Eat simple, easily digestible food;
- Last hearty dinner 2-3 hours before bedtime;
- Stop eating until you feel full;
- Do not include harmful foods in your diet: processed foods, smoked foods, pickles, fast food;
- Drink about 1 liter of fluid per day;
- Minimize the amount of salt consumed;
- Do not drink strong tea or coffee unless otherwise prescribed by your doctor.
Vitamins
In most cases, taking vitamins from the 36th week has already been discontinued. If the gynecologist did not do this at the previous appointment, it is worth asking him about the need to receive additional beneficial substances in the form of dietary supplements directly.
The removal of fortified complexes is carried out in order to prevent excessive weight gain of the fetus, so that the woman can avoid difficulties during childbirth. By this week, the fetus has completed its development, and the incoming nutrients from food will be enough to maintain the normal weight of the unborn child.
What to discuss with your doctor
- If tests reveal that you have low hemoglobin levels, talk to your doctor about what medications you can take. This condition cannot be corrected with diet, and your lack of iron means the same deficiency in your child.
- Breech presentation, that is, with the buttocks toward the cervix, is the reason for cesarean section in many cases. But in general, the baby has another 1-2 weeks to roll over. Find out from your gynecologist what exercises can help with this and when you should come for a follow-up ultrasound to check how the fetus is lying.
- Is intimate relations possible at 36 weeks of pregnancy? Check with your doctor to see if you have any contraindications. Usually, experts in the third trimester advise “not to get carried away,” and also to use a condom during sex, as the risk of infection is high, especially if the mucus plug begins to come off.
Good to know
Why does premature birth occur?
Which baby is considered premature?
How to test for amniotic fluid leakage at home
What is “oligohydramnios” during pregnancy?
Malpresentation of the fetus
How does childbirth occur with a breech presentation of the fetus?
All texts for pages about mother and baby were kindly provided by RAMA Publishing - these are chapters from the book by Svetlana Klaas “Your Favorite Little Man from Conception to Birth”, reviewer Irina Nikolaevna Kononova, Candidate of Medical Sciences, Associate Professor of the Department of Obstetrics and Gynecology of the Ural State Medical Academy (Ekaterinburg).
Possible complications
Many pregnant women complain of the following unpleasant symptoms at 36 weeks.
Pubic bone hurts
This happens under the influence of the hormone relaxin, which prepares muscles and ligaments for childbirth, making them softer and more elastic.
The belly becomes hard at 36 weeks of pregnancy
This feeling is associated with contractions - true ones, when labor begins, and training ones. You can tell them apart by measuring the time between contractions. During childbirth, they occur at regular intervals, and the pain increases. Training sessions are usually chaotic and will soon pass on their own. Uterine tone at 36 weeks may also be associated with this symptom. It is characterized by severe and prolonged pain.
The child moves less
This feeling may be subjective and due to the fact that the baby has become more crowded in the womb. However, if you really have doubts, it is better to tell your gynecologist about it. Using CTG or ultrasound, he will be able to quickly assess the condition of the fetus.
Legs become very swollen
This is sometimes inevitable in the third trimester of pregnancy. Don't limit yourself to fluids. Contrary to popular belief, this will only increase swelling if it appears. But in this case it is necessary to reduce salt consumption. If, against the background of swelling, nausea occurs, blood pressure or temperature increases, immediately consult a gynecologist: these are symptoms of gestosis in pregnant women.
Symptoms of premature birth
Let's list the signs by which you may suspect that the baby is in a hurry to be born ahead of time.
Spasms above the pubis. They are similar to period pain.
Pain, pressure and discomfort in the genital area, hips, pelvis. A dull pain occurs in the lumbar region.
Feeling of abs , pressure in the back.
Diarrhea , cramps and pain in the intestines.
Vaginal discharge - it gets worse. May be watery, pink, brown, or bloody.
Contractions of varying degrees of intensity. Touch your stomach with your fingertips and feel the contraction and relaxation of the uterus. Counted more than 4 contractions in 60 minutes? Call an ambulance - you need an urgent examination by an obstetrician.
The following symptoms are also dangerous: sudden blurred vision, flashes and “floaters” before the eyes, ongoing migraines, swelling of the face or hands, temperature 38º C or higher, painful urination, abdominal trauma, decreased fetal activity in the 3rd trimester (less than 10 movements in 12 hours).
Any of these symptoms indicate a risk of premature birth. Seek medical attention.
Preparing the breasts for lactation
The recommendation to “harden your breasts” by rubbing your nipples with a towel after a shower is hopelessly outdated. This method will not only not help in any way, but will also harm the delicate skin of the areola: irritation will appear, and during feeding, cracks will appear.
But what you should definitely pay attention to is the shape of the nipple. If it is flat or retracted, you will need to be patient and persistent because your newborn will have a hard time holding the breast properly in his mouth at first.
We advise you to buy a nipple shaper in advance - a shell-shaped device that will help it rise. Learn comfortable feeding positions and ways to help your baby latch on correctly.
Checklist for 36 weeks of pregnancy
- Don't miss any opportunity to relax. It is better to lie down, raising your legs or sitting on your left side. This way you will restore strength, improve blood circulation and cope with swelling in your legs.
- Install a contraction counter on your phone. Easy-to-use apps will help you differentiate between practice contractions and real ones.
- Sing, read and just talk to your child. This has a positive effect on both his well-being and your emotional state. There is an opinion that the baby, while in the womb, remembers the sounds of the mother’s lullaby, and will calm down and fall asleep easier after birth.
Do you have any questions? We will be happy to answer them during a consultation at any time convenient for you. Leave a request on the website.