Mycoplasmosis is a urogenital infection that causes inflammation of the tissues and mucous membranes of the genitourinary organs. The causative agent of the infection is several types of microorganisms that are present in the opportunistic flora of the male genital organs.
Treatment of mycoplasma in men
These include:
- Mycoplasma hominis;
- Mycoplasma genitalium;
- Ureaplasma urealyticum;
- Gardnerella vaginalis.
The bacteria are similar in morphological properties and structure. Therefore, in medicine they are often equated to one type of infection and treated with antibiotics. Bacteria are transmitted mainly through sexual contact, during unprotected sex. However, there are known cases of infection of men through domestic means - through common household and hygiene items.
Mycoplasma penetrates the cell structure and parasitizes, disrupting its natural growth. As a result, inflammation develops, which can develop into a serious illness. During the period of exacerbation of mycoplasma genitalia in men, treatment is necessary. Diagnosis and treatment of genital mycoplasmosis in men is performed by a urologist, venereologist, and andrologist.
Infectious agents
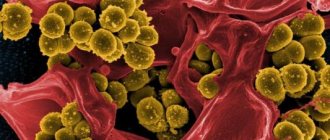
Representatives of the mycoplasma class are the smallest free-living microorganisms with a unique structure.
The absence of a cell wall makes these infectious agents similar to viruses, but in the scientific community mycoplasmas are still considered bacteria. Also, the unique biological properties of these microorganisms include the ability to maintain vital activity in a cell-free environment and the absence of a nucleus. Mycoplasmas are not Gram stained and cannot be identified using a light microscope. The absence of a rigid cell wall explains the numerous protective properties of mycoplasmas. These bacteria are resistant to many antimicrobials, including beta-lactam antibiotics. Conditionally pathogenic representatives of mycoplasmas live in the mucous membranes of various anatomical areas, including the genitourinary and respiratory tracts. Active spread of these microorganisms into the submucosa and bloodstream is observed only in immunosuppressive conditions. In this case, the bacteria can cause a systemic infection.
Representatives of mycoplasmas and associated diseases:
- Mycoplasma pneumoniae is a well-studied infectious agent that causes atypical pneumonia;
- Ureaplasma urealyticum and Ureaplasma parvum are responsible for the occurrence of nonspecific urethritis and other inflammatory processes in the genitourinary system;
- Mycoplasma hominis and Mycoplasma genitalium also affect the organs of the excretory and reproductive systems;
- Mycoplasma incognitos can provoke the development of disseminated infection.
Scientists also know of individual representatives of this bacterial class that can cause inflammatory processes in HIV-infected people. Further study of mycoplasmas will help doctors improve treatments for these diseases.
Complications of mycoplasmosis in women who do not go to the clinic in a timely manner
If the symptoms are ignored and there is a neglectful attitude towards health, mycoplasmosis in women provokes the development of complications. The consequences of advanced infection affect the reproductive system and musculoskeletal system.
Reproductive dysfunction
A prolonged course of infection causes inflammatory diseases of the genitourinary organs, contributing to the development of infertility:
- Endometritis. A chronic infectious process prevents the appearance of the secretory type of endometrium in the second phase of the menstrual cycle. Because of this, the fertilized gamete (egg) cannot attach to the uterine wall for further growth and development.
- Salpingoophoritis (adnexitis). Lack of treatment leads to the formation of adhesions, which impede the passage of the egg into the uterine cavity. The gamete dissolves in the pelvic organs, pregnancy does not occur.
Due to untimely treatment of mycoplasmosis, a woman loses the ability to conceive a child.
Reiter's disease
Long-term parasitism by Mycoplasma genitalium and Mycoplasma hominis affects the health of a woman’s joint system. A rheumatic disease develops, affecting the interphalangeal, ankle, and knee joints. Inflammation is accompanied by intense pain, swelling, and limited movement. The chronic course of Reiter's disease leads to loss of ability to work (disability).
Risk of infection during pregnancy
Infection with mycoplasmas during the perinatal period threatens the health of the unborn child. Delayed diagnosis of infection provokes:
- spontaneous termination of pregnancy;
- premature birth;
- amniotic sac rupture;
- excess amniotic fluid volume (polyhydramnios);
- underweight in a newborn;
- infection of a child with mycoplasmosis during childbirth.
Infected children have reduced immunity from birth. Newborns are susceptible to respiratory diseases, conjunctivitis, and urogenital diseases.
Methods of infection
When considering the etiology of mycoplasmosis, it is necessary to take into account that many opportunistic representatives of these bacteria can be present in human mucous membranes without clinical manifestations. The prevalence of carriage of the infection varies from 8% to 16%. Exclusively pathogenic types of mycoplasmas are transmitted sexually, but other modes of infection are also possible.
Methods of infection and risk factors.
- Unprotected oral or vaginal intercourse. Mycoplasmosis, transmitted in this way, is often combined with herpes, candidiasis and chlamydia.
- Household transmission due to the sharing of personal care items.
- Intrauterine damage to the fetus and transmission of infection during childbirth.
- Disruption of the immune system, leading to active reproduction of opportunistic flora.
- Personal history of other genitourinary infections.
- Promiscuous sexual intercourse.
Due to their asymptomatic course, patients can continue to infect other people, so it is important to be screened for genitourinary infections even in the absence of complaints. It is noted that carriage and latent course of mycoplasmosis is more typical for women.
Get tested for mycoplasmosis
Causes of the disease
The main cause of infection with genital mycoplasmosis in men is unprotected sexual contact with a partner who is infected with the causative agent of this disease.
Also, some factors can contribute to the reasons for the development of mycoplasmosis in men:
- Decreased immunity;
- Presence of other sexually transmitted diseases;
- Recurrent genitourinary inflammatory diseases.
Since the disease may not manifest itself for many years and is in a latent state, these factors can serve as an impetus for its further development.
Symptoms
Asymptomatic disease occurs in approximately 10% of patients. In carriers of the infection, mycoplasmosis can also manifest itself when exposed to unfavorable factors, such as deterioration of local immunity. Typically, in the early stages, bacteria affect the mucous membrane of the urethra, but as the disease progresses, mycoplasmas can retrogradely spread to the uterus, ureters, kidneys and other organs. Also, ascending infection is a cause of fetal damage in pregnant women.
Possible symptoms:
- pain in the lower abdomen;
- discharge of clear viscous fluid from the urethra and cervix;
- increased body temperature (fever) in acute infection;
- vaginal bleeding not associated with menstruation;
- pain during urination and sexual intercourse;
- menstrual irregularities;
- weakness and fatigue;
- decreased libido.
Due to frequent co-infection, doctors are not always able to identify the symptoms of mycoplasmosis, so the main diagnostic methods are based on laboratory indicators.
To a woman about preparing for tests
The objectivity of the results is enhanced by preliminary preparation for taking a blood test, including:
- refusal to take medications, drink alcoholic beverages;
- limiting physical activity on the eve of blood sampling;
- fasting for 8–12 hours before taking the test;
- quitting nicotine an hour before the procedure.
The rules for preparing for a smear collection include:
- three-day sexual abstinence;
- avoiding douching and vaginal suppositories before visiting a doctor;
- refusal to drink heavily on the day of the test;
- One hour before the procedure, you are prohibited from emptying your bladder.
A smear is taken on any day of the menstrual cycle, except for the first week of the follicular phase (the period of bleeding).
Diagnostics
To undergo an examination, you must contact a urologist or gynecologist. The doctor will ask the patient about complaints, collect anamnestic information and conduct an initial examination of the genitourinary system. Mycoplasmosis does not have specific external and symptomatic signs, so to make a final diagnosis, a specialist will need the results of several laboratory tests. A visual examination of internal organs may also be necessary to identify complications of the disease.
Reliable diagnostic methods.
- Isolation of bacterial culture. This test is suitable for the detection of Mycoplasma hominis and Ureaplasma urealyticum. Based on the resulting bacterial culture, it is also possible to determine the susceptibility of microorganisms to antibiotics.
- A smear followed by microscopic examination to rule out other bacterial infections.
- Polymerase chain reaction - obtaining specific sections of bacterial DNA. This method makes it possible to identify the causative agent of the disease with high accuracy.
- Serological studies aimed at detecting specific immunoglobulins in the patient’s blood.
- Ultrasound examination of the kidneys and bladder.
Based on the data obtained, the doctor will have to make a conclusion about which infectious agent causes the clinical manifestations of the disease. In the chronic form of the pathology, it is important to conduct an antibiotic sensitivity test before starting treatment.
Therapy
The treatment regimen for mycoplasma genitalium involves antibiotics. Depending on the strain of the microorganism and its sensitivity to the group of drugs, the doctor prescribes treatment. Therapy takes from 7 to 14 days. Additionally, medications that improve immunity may be prescribed. The procedures include lavage of the urethra to reduce inflammation.
The microorganism quickly develops resistance to the antibiotic, so after the course it is necessary to take a second test. If the pathogen is detected again, you need to undergo another course of antibiotic therapy, but with a different drug.
Treatment
Treatment methods depend on the specific causative agent of the disease, the presence of a secondary infection and the clinical manifestations of mycoplasmosis. Conditionally pathogenic representatives of mycoplasmas, including Mycoplasma hominis and Ureaplasma urealyticum, may be components of the natural microflora of the urogenital tract, so the issue of mandatory elimination of these microorganisms in the absence of complaints from the patient remains controversial. On the contrary, the detection of Mycoplasma genitalium in laboratory tests undoubtedly indicates the need for drug therapy.
Main methods of treatment:
- doxycycline or azithromycin are recommended antibiotics for mycoplasmosis;
- tetracycline antibiotics, macrolides, fluoroquinolones as alternative antimicrobial therapy;
- topical antimicrobial agents and antiseptics;
- antifungal drugs to exclude opportunistic infections;
- physical therapy to eliminate complications.
Medicines can only be prescribed by a doctor. It is important to observe the dosage and frequency of taking antibiotics to prevent the disease from becoming chronic. During pregnancy, it is important to choose safe medications that do not affect the condition of the fetus. On average, drug therapy for mycoplasmosis continues for 2-3 weeks, after which the doctor evaluates laboratory parameters and decides to stop treatment.
Urologists
Erkov Igor Viktorovich Urologist andrologist
Cost of admission 2500
₽
Make an appointment
Fomenko Alexander Pavlovich Urologist andrologist
Cost of admission 2500
₽
Make an appointment
Prognosis and complications
Timely use of antibiotics can eliminate the symptoms of mycoplasmosis in most patients. With a latent form of pathology, many women and men turn to the doctor too late, resulting in various negative consequences. Mycoplasmosis does not cause life-threatening complications for the patient, but the risk of developing a secondary infection must be taken into account.
Possible complications.
- Male and female infertility. Such negative consequences of infection develop when the reproductive organs are affected.
- Various complications during pregnancy, including miscarriage. Mycoplasmas are transferred to the fetal tissue through the bloodstream and disrupt the development of the new organism.
- Inflammation of the pelvic organs.
- Inflammation of the meninges and heart.
- Mycoplasma pneumonia, characterized by severe course.
People with weakened immune systems are at greatest risk of complications. First of all, these are HIV-infected patients. The pathological influence of other pathogenic microorganisms developing against the background of mycoplasmosis should also be taken into account.
Prevention
Infectious diseases caused by mycoplasma are not as easily preventable as other sexually transmitted infections. This is primarily due to conditionally pathogenic species of bacteria present in the natural microflora of the urogenital tract. These microorganisms can begin to multiply when the human body is exposed to any unfavorable factors. However, there are methods to prevent the transmission of Mycoplasma genitalium from one person to another.
Recommended methods of prevention:
- using a latex condom during intimate contacts;
- in order to avoid disruption of the natural urogenital microflora, it is recommended to avoid frequent ejaculation into the vaginal area;
- careful hygiene of the external genitalia.
Thus, mycoplasmosis is highly treatable. Because of the risk of asymptomatic infection, sexually active men and women are recommended to undergo regular screening for sexually transmitted infections. Screening is also necessary when planning pregnancy.
References
- Plakhova, K.I. Clinical significance of genetic variability of genital mycoplasmas. – Bulletin of Dermatology and Venereology, 2015. – No. 2. — P.76-83.
- Savicheva A.M., Shpitsina, E.V. Genital mycoplasmas. - Doctor, 2009. - No. 1. — P.9-12.
- Federal clinical guidelines for the management of patients with urogenital diseases caused by Ureaplasma spp., Mycoplasma Hominis; Moscow, 2015. - 24 p.
- Dessi, D., Margarita, V., Cocco, A. et al. Trichomonas vaginalis and Mycoplasma hominis: new tales of two old friends. - Parasitology, 2021. - Vol. 146(9). — P. 1150-1155.